All published articles of this journal are available on ScienceDirect.
Physeal Sparing Proximal Femoral Endoprosthetic Reconstruction with a Short Distal Segment: A Case Report
Abstract
Background:
A custom endoprosthesis allowed for the preservation of the distal femoral physis with a short remaining metaphyseal segment after osteosarcoma resection in a 10-year-old boy. CASE
Case Presentation:
This case illustrates a reconstructive alternative allowing physeal sparing with minimal remaining metaphyseal bone. At the three-year follow-up, the patient has remained complication-free with distal femoral growth maintaining symmetric limb length.
Conclusion:
When intercalary biologic reconstruction is not an option and the sacrifice of physis necessitates an extendible total femoral prosthesis, custom physeal sparing short segment press-fit fixation is an appropriate solution.
1. INTRODUCTION
In skeletally immature patients, physeal sparing sarcoma resection may prevent severe debilitating limb length discrepancy and allow joint preservation [1]. Distal femoral growth plate preservation should be the goal when oncologically safe to avoid total femoral replacement or an ablative procedure. In this case, a novel custom distal femoral fixation of a proximal femoral hemiarthroplasty is presented. This case is unique in using a press-fit stem design with an extramedullary phage plate and screw fixation in a short remaining distal femoral bone segment to preserve physis.
2. CASE
A 10-year-old male presented with gradual onset of activity-related, progressive proximal right thigh pain. X-rays showed an extensive permeative proximal femoral metadiaphyseal osteoblastic bone lesion extending from the lesser trochanter to the distal metaphysis with aggressive periosteal reaction and suggestion of circumferential soft tissue extension, suggestive of osteosarcoma (Fig. 1A-C).
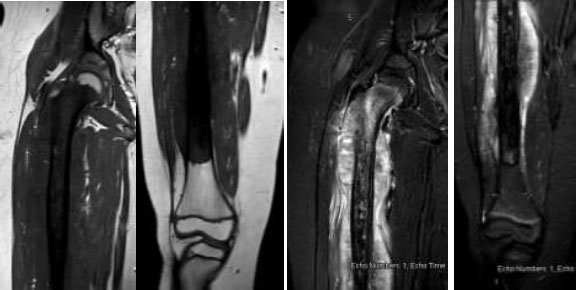
MRI showed an enhancing intramedullary lesion component extending from the femoral neck to within 5 cm of the distal femoral growth plate with circumferential extraosseous soft tissue (Fig. 2A-D). CT chest showed multiple bilateral lung nodules. Tc99 nuclear medicine scan showed no bone metastases. Open femur biopsy showed high-grade osteoblastic osteosarcoma. Neoadjuvant chemotherapy was initiated under Children’s Oncology Group AOST (All group OSTeosarcoma) 0331 protocol).
Because of the proximal involvement of the femoral neck, preservation of any proximal femur was deemed oncologically unsafe, necessitating proximal femoral intra-articular resection. Distal physeal-sparing resection was possible if an appropriate reconstruction with physeal sparing was devised. Accepting a 1 cm bone margin distally, 3.5 cm of bone remained from the distal cut to physis. A custom distal femoral short segment was designed for intra- and extra-medullary fixation with a short porous intramedullary stem with dual plate and screw fixation.
Restaging MRI after chemotherapy showed no changes in the tumor’s intraosseous or extraosseous extent or chest nodules by CT. Subsequent lung nodule resection was elected. Primary proximal femoral intra-articular resection with distal physeal sparing osteotomy was performed. To precisely achieve a clean margin leaving the planned 3.5 cm of distal metaphyseal bone to accommodate the custom implant, a custom cutting jig was affixed to the anteromedial metaphyseal periosteal surface just proximal to the planned osteotomy, pinned with 1.6 mm pins. After confirming a clear distal bone margin histologically, reconstruction was accomplished with the custom endoprosthesis (Onkos Surgical, New Jersey, USA) (Fig. 3A-D). Final permanent pathology evaluation showed all bone and soft tissue margins were clear with 95% tumor necrosis.
Chemotherapy was resumed 2 weeks postoperatively for four months. Three months after the local control procedure, thoracotomy with right upper and lower lobe nodule resections confirmed metastatic osteosarcoma with 100% necrosis. Restorative physical therapy (PT) with active motion, quad strengthening, and crutch toe touch weight bearing was initiated post-operatively. A hinged knee brace was locked in full extension for 6 weeks except during PT.
Femoral imaging every 3 months showed consistent femoral growth. The latest follow-up three years post reconstruction showed no instability or loosening and continued distal femoral growth (Fig. 4A-C).



A dedicated limb length study at 21 months showed symmetric limb lengths (Fig. 5A-B) Chest CT remained clear through the most recent visit 30 months post right upper and lower lobe metastasectomies.
3. DISCUSSION
We present a case of a 10-year-old male with osteosarcoma surgically managed with proximal femoral replacement and custom distal short-segment physeal sparing fixation. Three years post-op, the ipsilateral distal femoral growth plate remains open with no limb length discrepancy.
Potential limb length discrepancies after pediatric oncologic limb salvage surgery must be considered when planning resection and reconstruction. This is particularly relevant in the distal femur, the primary contributor to lower extremity growth, typically accounting for 40% of overall growth [2-7]. Growth plate preservation during resection is the simplest step to avoid limb-length discrepancy [3, 5]. Had resection of the entire femur been done, a total femoral prosthetic would have been the reconstruction of choice for limb sparing. Total femur replacements do poorly in the skeletally immature population with the potential for multiple procedures to correct leg length discrepancies, poor functional outcomes, and postoperative complications [3-13].
In the only published series of custom physeal-sparing endoprostheses like the one presented here, Tsuda et al. reported 18 patients, 11 with femoral tumors [14]. Overall results showed 79% five-year implant survival and only 3/18 implant failures. Physeal growth averaged 3.3 cm with maximum of 14 cm. However, 61% had complications, and 39% required additional surgery. In their three distal femoral cases, a similar construct to ours was used, although they used a cemented stem with a porous coated undersurface of the extramedullary phlanges, for which a press-fit ingrowth stem and non-porous coated plates were used.
Alternatives to custom prostheses for distal femoral growth plate preservation include allograft and vascularized fibular graft (VFG) reconstructions [9]. An eminent group from Buenos Aires, Argentina, has reported their results of allograft reconstruction [12]. Focusing on physeal preservation, they reported 13 patients with intercalary allografts for distal metaphyseal osteosarcomas in 2005 and 35 patients with proximal tibial and distal femoral osteosarcomas in 2015 [10]. Complications of these reconstructions, despite the arguably unparalleled allograft experience of this group, were frequent, as 7/11 (64%) of the patients had major complications, and 54% requiring additional surgery for complications [9]. Vascularized fibula grafts, either alone or in combination with allografts achieve high rates of healing and graft preservation, but fracture rates can be as high as 62% and donor site morbidities are concerning [10, 12]. Allograft Vfg reconstruc-tions popularized by the Rizzoli orthopedic oncology group achieved excellent functional results, but in their series of 81 pediatric sarcoma patients, complications were seen in nearly 30% (24/81) [5]. These options would not have been practical for this patient due to proximal femoral tumor extension.
Use of custom short-segment fixation endoprosthetic reconstruction of the proximal femur following distal femoral physeal sparing surgery maintains skeletal growth, preserves the native knee joint, and avoids complications associated with extendable endoprosthesis. Alternatives that maintain preservation of the distal physis also include extracorporeal devitalized autografts and 3D printed implants with tissue integration. Extracorporeal autografts are difficult for patients like this one with disease involving his femoral neck that require articular reconstructions. However, they have been shown to be a successful method for physis-preservation and functional outcome in long term follow-up [4].
The use of 3D printed reconstructions offers another uniquely patient specific custom approach. The 3D printed trabecular meshwork is thought to be more biocompatible and to have intrinsic osteogenic properties [6]. This technology is under development [9].
Establishing the safety and efficacy of the custom endoprosthesis in treating skeletally immature patients will require large, pooled numbers of patients at many large academic medical centers with much longer follow-up data. Although the findings are reassuring in this patient, further follow-up will be done to evaluate for long term prevention of limb-length disparity and safety [15, 16].

CONCLUSION
A 10-year-old boy has been treated with a custom physeal sparing short segment press-fit fixation due to minimal remaining metaphyseal bone. This solution is appropriate and allows for the avoidance of an extendable endoprosthetic. On three year follow up, the patient had no limb length discrepancy, preserved the joint, and avoided multiple surgeries with potential complications. Further studies are necessary to evaluate larger case series with longer follow-up to evaluate the long-term safety and viability of this approach.
LIST OF ABBREVIATIONS
| VFG | = Vascularized Fibular Graft |
| PT | = Physical Therapy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written consent was obtained for this patient from the patient’s parents.
STANDARDS OF REPORTING
CARE guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


