All published articles of this journal are available on ScienceDirect.
Comparison between Trans-articular and Subacromial Stabilization with Ligament Repair for Acute Acromioclavicular Dislocation
Abstract
Background:
Although numerous treatment options for acromioclavicular joint dislocation have been reported, the treatment strategy is not yet standardized.
Objective:
The purpose of this study was to evaluate the clinical and radiographic results of coracoclavicular ligament repair with temporary acromioclavicular stabilization using suture anchors and Kirschner wires, and to compare the results between temporary trans-articular fixation and subacromial stabilization of the acromioclavicular joint.
Methods:
Thirty-three cases with displaced acromioclavicular joint dislocation were retrospectively evaluated. In the first 14 cases, the wires temporarily penetrated the joint for an average of 7 weeks (trans-articular group), while the acromioclavicular joint was temporarily stabilized by wires passing under the acromion that were inserted into the distal clavicle for an average of 13 weeks in the latter 19 cases (subacromial group). Clinical and radiographic results were evaluated and compared between the two groups.
Results:
The average UCLA score was 32.0 points in the trans-articular group and 32.8 points in the subacromial group, indicating no difference between the two groups (P = 0.418). Coracoclavicular distance ratio after surgery was significantly smaller in the subacromial group (P ≤ 0.035), and acromioclavicular dislocation ratio after removal of the wires was also smaller in the subacromial group (P ≤ 0.001) compared with the trans-articular group.
Conclusion:
This study revealed that coracoclavicular ligament repair with temporary acromioclavicular stabilization leads to favorable clinical results, with the subacromial group showing better maintenance of joint reduction compared with the trans-articular group. Subacromial wire stabilization is a viable option for long-term temporary fixation of acute displaced acromioclavicular joint dislocation.
1. INTRODUCTION
Acromioclavicular dislocation is a common injury in active patients [1], and numerous treatment options for acromioclavicular joint dislocation have been described [2]. However, loss of reduction [3-5] and postoperative osteoarthritis of the acromioclavicular joint [5, 6] are often observed after surgery, and the treatment strategy has not yet been standardized [7]. The main pathology in acromioclavicular joint dislocation is disruption of the suspension mechanism of the clavicle following the rupture of the coracoclavicular ligament [8], with the resultant dislocation causing abnormal kinematics of the shoulder girdle [9, 10]. Thus, reconstruction of the suspension mechanism is an integral part of the surgical treatment of displaced acromioclavicular dislocation.
For the reconstruction of the suspension mechanism of the coracoclavicular ligament, the ruptured coracoclavicular ligament is repaired using anchoring sutures [11-13]. To protect the repaired ligament, the acromioclavicular joint is temporarily fixed using two Kirschner wires that penetrate the joint [14] in the earlier cases, and the wires are removed 6 to 8 weeks after surgery. However, our earlier cases often showed postoperative correction loss after the removal of the wires. Hence, we commenced stabilizing the acromioclavicular joint by inserting Kirschner wires below the acromion for 12 to 14 weeks, along with coracoclavicular ligament repair in the latter cases. Patients who underwent repair by this technique were allowed to move their shoulders during subacromial stabi- lization.
The purpose of this study was to evaluate the clinical and radiographic results of coracoclavicular ligament repair with temporary acromioclavicular stabilization for displaced acro- mioclavicular joint dislocation, and to compare the results between temporary trans-articular fixation and subacromial stabilization.
2. MATERIALS AND METHODS
During the period between December 2009 and April 2017, we surgically treated displaced acromioclavicular joint dislocation by coracoclavicular ligament repair with temporary acromioclavicular joint stabilization using two suture anchors and two Kirschner wires. Inclusion criteria in this study were 1) acute displaced acromioclavicular dislocation, in which the coracoclavicular distance exceeded that on the contralateral side on plain antero-posterior radiographs by 200%; 2) early surgical intervention within 3 weeks after injury, 3) a more than 6-month follow-up period. Two cases were lost to follow-up, and a total of 33 cases (31 men, 2 women) were retros-pectively evaluated. The patients’ average age was 40.6 ± 15.8 years (range, 14 - 66 years). The dominant shoulder was invol- ved in 25 cases (75.8%), and the nondominant in 8 cases (24.2%).
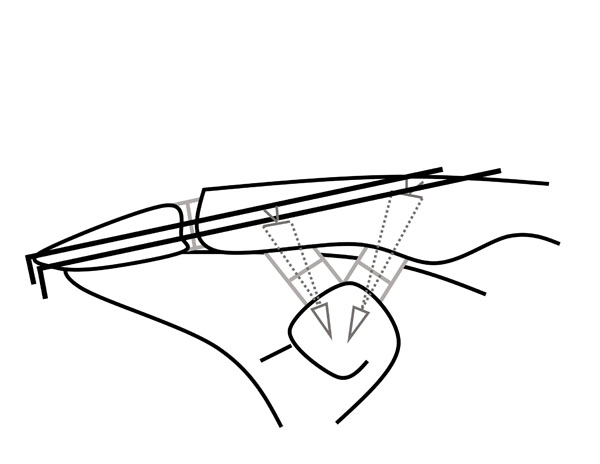
Surgical intervention was performed by a single surgeon on an average of 8.5 ± 3.5 days (range, 3 - 17 days) after the injuries. During surgery, the patients were placed in the beach chair position. Through a 6-cm skin incision from the midshaft to the lateral end of the clavicle, the fascia of the trapezius and deltoid muscles was exposed. After detaching the anterior deltoid from the distal clavicle, the superior portion of the coracoid process was exposed. Two suture anchors (Mitek G2® Anchor or PANALOK® Anchor, Depuy Synthes, Mitek Sports Medicine, Raynham, MA, USA) were inserted on the coracoid process. Using 1.2-mm diameter Kirschner wires, two bone tunnels corresponding to the insertion of the trapezoid ligament onto the distal clavicle and two bone tunnels corresponding to the insertion of the conoid ligament were created. The bone tunnels for the trapezoid ligament were located in the anterior part of the distal clavicle, and their inferior holes coincided with the insertion of the ruptured trapezoid ligament. Bone tunnels for the conoid ligament were located in the posterior portion of the distal one-third of the clavicle at the conoid tuberosity, and their inferior holes coincided with the insertion of the ruptured conoid ligament [15]. Through the ruptured conoid and trapezoid ligaments, which were attached to the undersurface of the distal clavicle, both ends of the threads of the suture anchors were respectively guided into the bone tunnels, and the threads were left untied (Fig. 1A).

Then, the dislocated acromioclavicular joints were reduced and temporarily stabilized with two Kirschner wires (1.8 mm in diameter) inserted through two 1-cm skin incisions lateral to the acromion process under fluoroscopic control. In the first 14 shoulders, the wires penetrated the acromioclavicular joint (trans-articular group). After stabilization of the acromiocla- vicular joint, the threads of the suture anchors were tied over the clavicle. Then, the fascia of the deltoid and trapezius muscles were imbricately repaired [16]. The distal ends of the wires were bent and were cut 2 cm from the bent point. The wires were left under the skin and the wound was closed (Fig. 1B). Shoulder motion was limited to 90-degrees of elevation during temporary fixation. After removal of the wires under local anesthesia at an average of 7.1 ± 0.7 weeks after the surgery (range, 6 - 8 weeks), the patients were allowed to move their shoulder without any restriction, and to return to sports activities 3 months after the surgery.
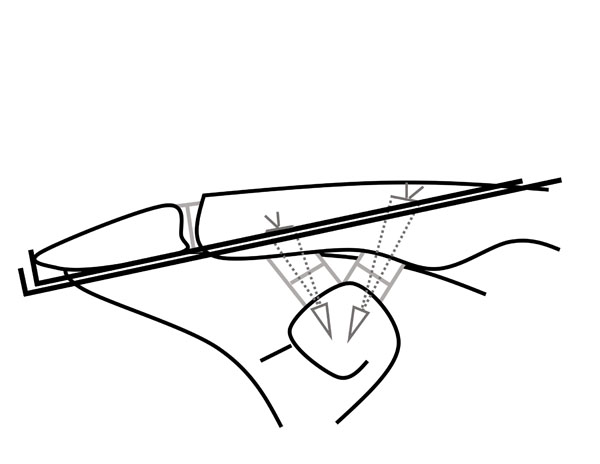
In the latter 19 cases, the acromioclavicular joint was stabilized with two wires inserted under the acromion through two 1-cm skin incisions lateral to the acromion process (subacromial group). The wires were passed under the acro- mion and were inserted into the distal end of the clavicle without penetration. Then, the threads of the suture anchors were tied over the clavicle, and the fascia of the deltoid and trapezius muscles were imbricately repaired [16]. The distal ends of the wires were bent and were cut 2 cm from the bent point and, the wires were left under the skin (Fig. 1C). In the subacromial group, the patients were allowed to move their shoulder without limitation during temporary stabilization. After removal of the wires under local anesthesia at an average of 13.3 ± 1.1 weeks after surgery (range, 12 - 14 weeks), the patients were allowed to return to sports activities and heavy labor.
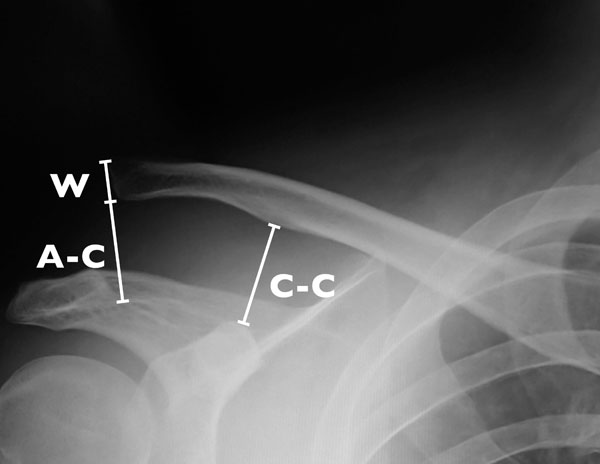
The UCLA shoulder score at the time of final follow-up in the two groups was assessed and compared using Mann-Whitney U tests. In radiographic evaluation, coracoclavicular distance ratio, which is calculated as the ratio of the coracoclavicular distance on the affected side to that on the contralateral side on plain antero-posterior radiographs, and acromioclavicular dislocation ratio, which is calculated as the ratio of the distance between the undersurface of the acromion and distal clavicle to the width of the distal end of the clavicle on plain antero-posterior radiographs, was evaluated at the time of injury, immediately after surgery, 3 months after surgery, 6 months after surgery, and at final follow-up (Fig. 2). Coracoclavicular distance ratio and acromioclavicular dislocation ratio were compared between the two groups using the Mann-Whitney U test. Calcification of the repaired ligaments and arthritic changes in the acromioclavicular joint were evaluated on radiographs at the time of final follow-up, and both groups were compared using chi-squared tests. The significance level was set at 0.05 for all analyses.
3. RESULTS
The average follow-up period was 13.5 ± 10.2 months (range, 6 - 43 months). No major complications were found in both groups, and all cases returned to their usual jobs and sports activities at the time of the final follow-up. Displacement of the inserted wires was identified in one case in the trans-articular group and one case in the subacromial group, both of which were managed by resting the affected shoulder. The subacromial disorder was not found during the follow-up period in the subacromial group. The average UCLA shoulder score at the final follow-up was 32.0 ± 2.3 (range, 28 - 35) points in the trans-articular group and 32.8 ± 2.3 (range, 29 - 35) points in the sub-acromial group, indicating no difference between the two groups (P = 0.418).
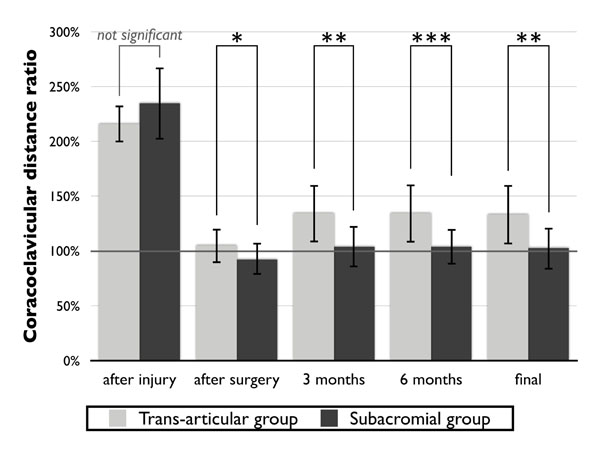
All 33 cases were classified as type V acromioclavicular joint injury according to the Rockwood classification at the time of injury [17]. At the time of final follow-up, the trans-articular group showed 4 cases of Rockwood type I (28.6%), 3 cases of type II (21.4%) and 7 cases of type III acromioclavicular joint injuries (50.0%), while the subacromial group had 15 cases of Rockwood type I (78.9%), 3 cases of type II (15.8%) and 1 case of type III injury (5.3%). Average coracoclavicular distance ratio was 226.7 ± 28.5% at the time of injury (range, 200% - 314%) and 115.7 ± 26.9% at the time of final follow-up (range, 73% - 186%). Coracoclavicular distance ratio did not differ between the trans-articular and subacromial groups at the time of injury (215.8% and 234.8%, P = 0.084), although the ratio was significantly higher in the trans-articular group than in the subacromial group immediately after surgery (105.0% and 92.3%, P = 0.035), 3 months after surgery (134.5% and 103.7%, P = 0.001), 6 months after surgery (134.4% and 103.7, P < 0.001) and at the final follow-up (133.3% and 102.7%, P = 0.001) (Fig. 3A). Average acromioclavicular dislocation ratio was 121.4 ± 40.7% at the time of injury (range, 71% - 250%) and 14.0 ± 21.3% at the time of final follow-up (range, -15% - 63%). Acromioclavicular dislocation ratio was not different between the two groups at the time of injury (125.6% and 124.6%, P = 0.529) and immediately after surgery (0.9% and -4.6%, P = 0.132), although the ratio was significantly smaller in the subacromial group than in the trans-articular group at 3 months after surgery (27.4% and 0.4%, P < 0.001), 6 months after surgery (28.7% and 2.8%, P < 0.001), and at the final follow-up (29.3% and 1.6%, P < 0.001) (Fig. 3B).

Five cases in the trans-articular group (36%) and nine cases in the subacromial group (47%) showed calcification of the repaired ligaments, with no difference being observed between the two groups (P = 0.503). However, the progression of arthritic changes in the acromioclavicular joint was significantly higher in the trans-articular group (8 cases, 57%) compared with the subacromial group (2 cases, 11%) (P = 0.004).
4. DISCUSSION
The present study evaluated the clinical and radiographic results of coracoclavicular ligament repair with temporary acromioclavicular stabilization for the treatment of acute acromioclavicular joint dislocation. Since disruption of the suspension mechanism of the clavicle following rupture of the coracoclavicular ligament is the main pathology of acromioclavicular joint dislocation [8], we repair ruptured coracoclavicular ligaments using anchoring sutures [11-13]. Additionally, the acromioclavicular joint is temporarily stabilized until the repaired ligaments are thought to have healed. This study revealed that coracoclavicular ligament repair with temporary acromioclavicular stabilization leads to favorable clinical results, with subacromial stabilization for an average of 13 weeks achieving superior reduction of the dislocation compared with a trans-articular fixation for an average of 7 weeks.

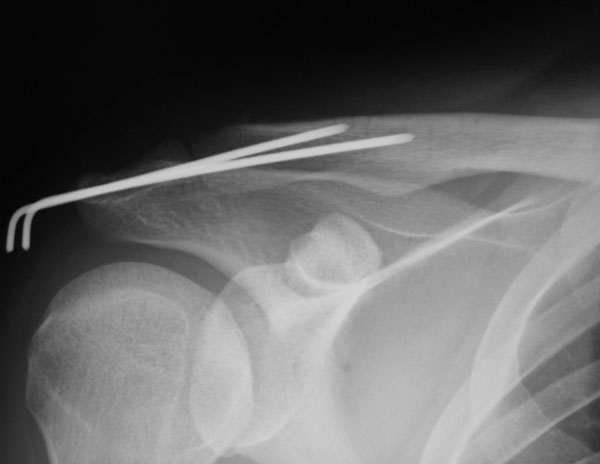
Traditionally, temporary fixation using Kirschner wires inserted into the acromioclavicular joint with or without additional reconstruction has been utilized for the treatment of acromioclavicular dislocation [5, 14]. Phemister [14] stated that a period of 6 weeks to 2 months is required for healing of the ligament, and hence, the wires should be removed 2 months after fixation. Although the clinical results of all patients were acceptable, our trans-articular group frequently showed a loss of reduction of the joint (Fig. 4A-C). The repaired coracoclavicular ligaments, which suspend the shoulder girdle against gravity in the natural sitting or standing position, have to be strong enough to support the weight of the upper extremity all day long when protection of the joint is removed. The present results indicate that the strength of the repaired coracoclavicular ligaments using anchoring sutures is insufficient to support the weight of the arm for up to 2 months after surgery.

In the conservative treatment of ligament rupture of the ankle, joint stability reportedly requires more than 3 months for recovery [18]. Similarly, in a previous series, the nonoperative treatment of ruptured medial collateral ligaments of the knee resulted in functional recovery 3 months after injury [19]. Temporary hook plate placement is also reported to yield good outcomes for acromioclavicular dislocation [20], and the plates are frequently removed approximately 3 months postoperatively [7]. When wires penetrate and completely fix the acromioclavicular joint, however, breakage of the wires often occur [21, 22], and long-term fixation of the joint might cause postoperative contractures and arthritis. In contrast, subacromial stabilization without penetration of the joint does not fix the acromioclavicular joint, but stabilizes it by the placement of the wire below the inferior surface of the acromion. Thus, we are able to leave the wires in place for 3 months, while still allowing shoulder elevation during stabilization. In our series, patients who underwent temporary subacromial stabilization for 3 months experienced significant maintenance of the reduced position even after removal of the wires (Fig. 5A-C). During subacromial stabilization, the dislocation needs to be a bit over-corrected to insert the wires at the distal end of the clavicle, which might be an advantage for the healing of the repaired ligaments. Furthermore, unlike hook plates [20], subacromial stabilization does not damage the repaired fascia of the trapezius and deltoid muscles, which are important for joint stability, as occurs during the removal of metal implants. Temporary subacromial stabilization, thus, appears to be a good and viable treatment option for long-term stabilization of the acromioclavicular joint.


Postoperative arthritic changes in the acromioclavicular joint are also found after surgical intervention for acromioclavicular joint dislocation [5, 6]. Despite the short-term follow-up period, our trans-articular group frequently showed radiographic arthritis of the acromioclavicular joint. Damage to the articular cartilage might be caused by the initial trauma, residual instability of the joint after surgery, and iatrogenic invasion by wires during surgery. Since the acromioclavicular joint is small in size, two 1.8-mm diameter Kirschner wires might be too invasive for the articular cartilage. In some cases, furthermore, multiple trials of wire insertion were needed for stable temporary fixation of the small joint due to technical problems. Subacromial stabilization, in which the wires do not penetrate the small joint, being less invasive for the articular cartilage than trans-articular fixation, might, therefore, decrease the incidence of postoperative arthritis of the acromioclavicular joint.

Calcification of the coracoclavicular ligaments is often found after operative and nonoperative treatment of acute acromioclavicular joint dislocation [23-25]. Fourteen cases showed calcification of the repaired coracoclavicular ligaments in the present study, but no difference was observed between the trans-articular group and the subacromial group. Calcification of the ligaments appears not to be correlated with the clinical symptoms, and the result was consistent with past reports [24, 25]. Although its pathological significance remains unclear, ligament calcification might reflect one of the healing mechanisms of the repaired coracoclavicular ligament in cases with acromioclavicular dislocation.
The present study evaluated the clinical and radiographic results of coracoclavicular ligament repair with temporary wire stabilization for the treatment of displaced acromioclavicular joint dislocation, and compared the results between temporary trans-articular fixation and temporary subacromial stabilization. However, the small number of cases and the short follow-up period are limitations of the current study. Although we found no further displacement at 6 months after surgery in our cases, long-term follow up of more than 1 year might reveal different results. Further investigation will be needed to clarify the advantage of temporary subacromial stabilization after coracoclavicular ligament repair.
CONCLUSION
This study revealed that coracoclavicular ligament repair with temporary joint stabilization for acute acromioclavicular dislocation leads to favorable clinical results, with the subacromial group showing better maintenance of joint reduction compared with the trans-articular group. Temporary subacromial stabilization is a viable option for long-term temporary fixation of acute displaced acromioclavicular joint dislocation.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Institutional Review Board of Keio University School of Medicine (No. 20130147).
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was taken from all the patients when they were enrolled.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


