All published articles of this journal are available on ScienceDirect.
Relief of Lower Back and Leg Pain after Myelography
Abstract
Introduction:
It is well-known that many patients will have adverse reactions such as headache and nausea after undergoing myelography, but we have often seen cases where symptoms such as lower back pain and leg pain were alleviated following myelography. To the best of our knowledge, such clinical cases of post-myelographic alleviation have not been reported.
Materials and Methods:
A total of 325 patients with a degenerative lumbar spinal disorder who underwent myelography were prospectively investigated at four hospitals from April 2012 to March 2014 to survey the post-myelographic alleviation of lower back and leg pain prospectively. The severities of lower back pain, leg pain and numbness of the lower extremities were evaluated and intermittent claudication distance was measured before myelography. The magnetic resonance imaging (MRI) findings and myelographic findings were also evaluated for the patients that their symptoms were improved.
Results:
Thirty-five of 325 cases (10.8%) of these patients had their symptoms alleviated after undergoing myelography; 26 cases of lower back pain, two cases of leg pain, two cases of numbness of the lower extremity, and five cases of intermittent claudication.
Conclusion:
In the patients of a degenerative lumbar spinal disorder, about 10% cases with lower back pain or intermittent claudication had post-myelographic alleviation. Intradural injection therapy might be a therapeutic method to alleviate these symptoms.
INTRODUCTION
While headache and nausea are widely known as adverse reactions following myelography, we have often seen cases where symptoms such as lower back pain and leg pain were alleviated following myelography. However, such clinical cases of post-myelographic alleviation have not been reported. In this study, the types and rates of symptoms that were alleviated after myelography were reviewed.
METHODS
A total of 325 patients with a degenerative lumbar spinal disorder who underwent myelography for its evaluation at our university or affiliated hospitals were surveyed prospectively. We did myelography for all patients who were planned to undergo surgery from April 2013 to March 2015. The patients’ mean age was 68.2 years (32-96 years), and the patients included 148 men and 177 women; the principal symptoms were lower back pain (178 cases), leg pain (263 cases), numbness of the lower extremity (214 cases), and intermittent claudication (211 cases). The mean duration of symptoms up to the time of myelography was 9 months (one month - five years). The maximum compression level of the dural tubes on MRI findings was L3/4 in 49 cases, L4/5 in 173 cases, L5/S1 in 91 cases, and others in 12 cases. Omnipaque 240® (Iohexol, Daiichi Sankyo Company, Tokyo, Japan) was used as a contrast medium.
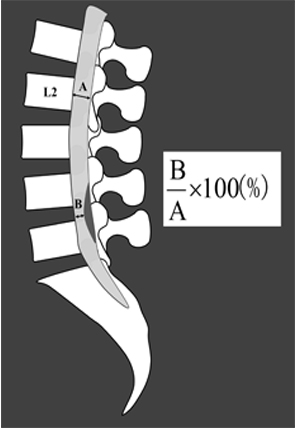
The severities of lower back pain, leg pain, and numbness of the lower extremity were evaluated using a visual analogue scale (VAS) immediately before and on the day after myelography, and the intermittent claudication distance was also measured. The MRI findings were evaluated by (B/A) × 100 as the MRI constriction rate, where the maximum anteroposterior diameter of the dural tube at the mid L2 vertebra was defined as A, and the anteroposterior diameter of constriction was defined as B on the T2-weighted sagittal section (Fig. 1). Myelographic findings were evaluated in three stages, as no block, incomplete block, and complete block. When the VAS of lower back pain, leg pain, and numbness of the lower extremity was improved by 20 mm or more and the intermittent claudication distance was improved by 50 m or more, the symptom was considered alleviated. We checked MRI and myelography findings of the patients that their symptom were improved to know radiological features in patients with post-myelographic alleviation. This research was conducted with the approval of our university’s ethical committee (approval number 1677).
RESULTS
Patients whose symptoms were alleviated by myelography accounted for 35 of 325 cases (10.8%): 26 cases of lower back pain, two cases of leg pain, two cases of numbness of the lower extremity, and five cases of intermittent claudication. The MRI constriction rate in patients whose symptoms were alleviated by myelography was not higher than 25% in one case, 25% to less than 50% in 25 cases, 50% to less than 75% in six cases, and not less than 75% in three cases, and the myelographic finding was no block in two cases, incomplete block in 32 cases, and complete block in one case.
DISCUSSION
The present study results showed that symptoms such as lower back pain and leg pain were alleviated in about 10% of patients after myelography. Thorstensen et al. studied 99 patients with lumbar myelography. They reported that 39% of the patients had their back pain alleviated, 15% had their thigh pain alleviated, and 11% had their calf pain alleviated [1]. The potential mechanisms of post-myelographic alleviation of symptoms are discussed below.
In this study, the patients who complained of lower back pain tended to have their pain alleviated, and they had mild stenosis of the dural tubes on MRI and incomplete block on myelography. This suggests the possibility that passage of contrast medium through the constricted site caused physical changes in the internal pressure of the dural tubes or radicles. In patients with complete block on myelography, the contrast medium could not pass through the constricted site and could not change the internal pressure.
Damage and degeneration of the components of the spine may be the cause of lower back pain. Schwarzer et al. studied 92 patients with chronic lower back pain and reported that there were 36 patients with discogenic pain, eight patients with pain derived from the facet joint, and three patients with both [2]. Moreover, though the reason is unclear, it is known that lower back pain is improved with surgery in some patients with lumbar spinal stenosis. Alimi et al. reported that the lower back pain of 50% of patients with lumbar spinal stenosis was improved after decompression surgery [3]. In the present study, lower back pain might have improved due to the decompression-like effect of contrast medium, but it is very hard to prove this scientifically.
Regarding the symptoms of lumbar spinal stenosis, it is said that not only mechanical deformation, but also circulatory disturbance plays an important role. Delamarter et al. [4] studied the effect of compression of the cauda equina in dogs. They reported that edema, loss of myelin, and venous congestion occurred in the roots of the lumbar spine with 50% constriction of the cauda equina, and in addition, severe arterial narrowing occurred with 75% constriction. Kobayashi et al. [5] studied imaging of cauda equina edema in dogs. They concluded that occlusion of the subarachnoid space by stenosis of the lumbar canal resulted in congestion and degeneration of the nerve root. At that time, the blood-nerve barrier was broken down, leading to an increase in endoneurial pressure. It is known that some contrast medium has high osmotic pressure. In this study, it is not clear whether arterial ischemia or venous congestion contributed to the symptoms, but the contrast medium might contribute to alleviation by improving blood circulation and nerve edema.
The present study may have limitations because: the duration of alleviation of lower back or leg pain was not evaluated; no control group of dural puncture was set up to rule out a placebo effect; and no detailed clinical information on the nature of lower back pain and leg pain was obtained.
CONCLUSION
In the patients of a degenerative lumbar spinal disorder, about 10% cases with lower back pain or intermittent claudication had post-myelographic alleviation. The present study results suggest that intradural injection therapy might be a therapeutic method to alleviate lower back and leg pain.
ETHICAL STANDARDS AND PATIENT CONSENT
We declare that all human have been approved by our university’s ethical committee (approval number 1677), and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
AUTHORS' CONTRIBUTION
R. Guo drafted the manuscript, did first selection of articles, and assessed the quality of the papers. T. Sakakibara, K. Akeda and T. Kondo had data collection. T. Mizuno assessed the quality of the papers, and revised the manuscript critically for its content. Y. Kasai helped to draft and to correct the manuscript. All authors read and approved the final manuscript.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


