All published articles of this journal are available on ScienceDirect.
Importance of Restricting Sportive Activity and Time from Injury to Surgery in Anterior Cruciate Ligament Reconstruction
Abstract
Objectives :
It is unclear that how long reconstruction may be delayed before additional intraarticular injuries occur. Our aim was to determine the relationship of time period from injury to surgery with the incidence of meniscal and chondral injuries recorded at the time of surgical treatment for ACL tears. The effect of sportive activity restriction, grade of chondral lesions and their locations were also evaluated
Patients and Methods :
213 patients who underwent arthroscopic anterior cruciate ligament reconstruction were evaluated retrospectively. Data were analyzed for association between time period before surgery and patients sportive activity restriction with rates of meniscal and chondral injuries. According to time from initial trauma to surgery less than 12 months grouped as group I (101 patients) and 12 months and longer defined as group II (81 patients). Patients who had surgery before 12 months were divided into groups of smaller time scales (0 to 3 months, 4 to 6 months, 7 to 9 months, 10 to 12 months) to examine the relationships more closely. For sportive activity restriction a functional scale was used that described restricted activities including military training.
Results :
One hundred eighty-two patients were included to the study. 81 patients restricted sportive activity before surgery. 18 (% 22.2) of these patients had chondral injury [6 (% 33.3) operated before 12 months and 12 (% 66.7) operated after 12 months]. The difference was statistically significant (p=0,005). 81 patients (group II) were operated after 12 months. There were 44 (% 54.3) patients with chondral injury in this group [32 (% 72.7) patients were who continued their sportive activity and 12 (% 27.3) patients who restricted their sportive activity]. The difference was statistically significant (p=0,026). Correlation analysis showed that with increasing time from initial trauma to surgery chondral lesion incidence and grade of these lesions increases (p<0,001, p=0,001).
Conclusion :
The results indicate that the prolonged time from injury to surgery and continuing sportive activity before surgery increases the incidence of the chondral lesions. Also, time limit of 12 month is important to prevent chondral injury in anterior cruciate ligament reconstruction.
INTRODUCTION
Anterior cruciate ligament (ACL) injury is very common. Reconstruction of anterior cruciate ligament is one of the most commonly performed orthopedic surgeries. Some patients with anterior cruciate ligament injury deny surgical treatment or delay their surgical treatment. However delayed surgical reconstruction or intense sports activity during conservative treatment can cause repeating incidences of giving way. This may lead to additional intraarticular injuries. In recent studies Magnussen RA et al. and Ghodadra N et al. mentioned that additional medial compartmental cartilage injuries increased in patients with delayed anterior cruciate ligament reconstruction [1, 2]. Sri-Ram K et al. conclude that the chance of additional meniscal injury increased by a factor of two if surgery delayed more than five months and by a factor of six if surgery was delayed more than twelve months [3]. Incidence of meniscal lesions and chondral injuries is not documented well in patients who did not restrict their sportive activities. Also it is unclear that how long reconstruction can be delayed before additional intraarticular injuries occur. Dumont GD et al. found active daily life and increasing time from injury to surgery has higher risk of re-injury and higher prevalence of intraarticular injury [4]. Patients who had anterior cruciate ligament injuries are usually active patients who participate in sportive activities. These patients may have the idea that, by restricting their sportive activities they can delay their surgery with no harm. It is unclear that which is more important to avoid additional injuries restricting sportive activity or not delaying surgery. If restricting sportive activity is important it is possible for these patients to delay their surgery before additional intraarticular pathologies occur. Our aim was to determine the relationship of time period from injury to surgery with the incidence of meniscal and chondral injuries recorded at the time of surgical treatment for ACL tears. The effect of sportive activity restriction, grade of chondral lesions and their locations were also evaluated.
PATIENTS AND METHODS
213 patients who underwent arthroscopic anterior cruciate ligament reconstruction evaluated retrospectively. Approval of the Ethics Committee was included in the study. All patients were male military personnel and their mean age was 25 years (ranging 20 to 47 years). Clinical history, time from initial trauma to surgery, age and activity level during preoperative time was recorded. Details of inclusion criteria are shown at Table 1. The type of chondral lesions and their locations were recorded by same surgeon to a standard form. Chondral lesions were recorded according to International Cartilage Repair Society classification. Grade I and II lesions considered as low grade lesions whereas grade III and IV lesions considered as high grade lesions. The localization of chondral lesions was defined according to the location in the articulation surface. Six different localizations for lesions were described as follows: medial femoral condyle (MFC), lateral femoral condyle (LFC), femoral articulation surface of patella (P), femur trochlear articulation surface (FT), medial tibial plateau (MTP) and lateral tibial plateau (LTP). Total of 182 patients’ met the criteria and included the study. All operations made in the same institute by same surgeon. Patient’s initial MRI’s were investigated and only isolated ACL injury patients included to the study. All of the records were reviewed to evaluate the incidence of meniscal and chondral injuries. Additional details such as a mechanism of injury, type of reconstruction were also recorded. Localization of the chondral and meniscal injury was also documented. Patients were grouped according to time period after initial trauma that caused ACL injury. According to time from initial trauma to surgery less than 12 months was grouped as group I (101 patients) and 12 months and longer was defined as group II (81 patients). Then the patients who had surgery before 12 months were divided into groups of smaller time scales to examine the relationships more closely. These were: A) 0 to 3 months; B) 4 to 6 months; C) 7 to 9 months; D) 10 to 12 months. As regards the groups with smaller time scales, there were 23 patients in group A, 35 in group B, 19 in group C and 24 in group D. Later in all groups patients were subdivided into two; one who restricted their sportive activity and the other who didn’t restricted their sportive activity before ACL reconstruction surgery. Restricted physical activities were listed in a form which includes basic physical training activities and combat physical training activities (Table 2). Incidence of meniscal tears and chondral lesions was determined and compared with the time of surgery and patients sportive activity.
Statistical Analysis
IBM SPSS Statistic Version 20.0 software was used for statistical analysis. In evaluation of the data descriptive statistical methods (mean, standard deviation) and Spearman’s rank correlation test was used to test whether time from initial trauma to surgery was significantly correlated with the presence or absence of cartilage lesions and grade of cartilage lesions. For crude analysis of independent groups of qualitative data, Fisher’s exact test, Chi-square test and Chi-square trend test were used. A 95% confidence interval, significance at p <0.05 were accepted.
RESULTS
In between these 182 patients there were 81 patients who restricted their sportive activity before surgery. In between
these 18 patients (% 22.2) had chondral injury [6 (% 33.3) patients were operated before 12 months and 12 (% 66.7) patients were operated after 12 months]. The difference was statistically significant (p=0,005). Also 55 (% 67.9) patients had meniscal injury 33 (% 60) operated before 12 months 22 (% 40) operated after 12 months. There were no statistical difference between them (p=0,642). According to time from initial trauma to surgery there were 101 (% 55.5) patients in group I which had surgery before 12 months and in group II there were 81 (% 44.5) patients which had surgery after 12 months. In Group I (time from initial trauma to surgery less than 12 months) there were 15 (% 14.9) patients with chondral injury. In between these patients 9 (% 60) were who continued their sportive activity and 6 (% 40) patients were who restricted their sportive activity. There were no statistically significant difference between them (p=0,425). Also in Group I there were 66 (% 65.3) patients with meniscal injury. In between these patients 33 (% 50) were who continued their sportive activity and 33 (% 50) were who restricted their sportive activity. There were no statistically significant difference between them (p=0,831). Also after applying smaller time scales as A) 0 to 3 months; B) 4 to 6 months; C) 7 to 9 months; D) 10 to 12 months there were no significant difference between them in respect to chondral and meniscal injury (Table 3). In group II (time from initial trauma to surgery more than 12 months) there were 44 (% 54.3) patients with chondral injury. In between these patients 32 (% 72.7) patients were who continued their sportive activity and 12 (% 27.3) patients were who restricted their sportive activity. And the difference was statistically meaningful (p=0,026). Also in Group II (time from initial trauma to surgery more than 12 months there were 62 (% 76.5) patients with meniscal injury. In between these patients 40 (% 64.5) were who continued their sportive activity and 22 (% 35.5) were who restricted their sportive activity. There were no statistically significant difference between them (p=0,351). The correlation coefficient, between time from initial trauma to surgery and chondral lesion was 0.395 (p<0,001) and between time from initial trauma to surgery and grade of these lesions was 0.244 (p=0,001). Correlation analysis showed that with increasing time from initial trauma to surgery chondral lesion incidence and grade of these lesions increases (p<0,001, p=0,001). The localization of chondral lesions was defined according to the location in the articulation surface (Fig. 1).
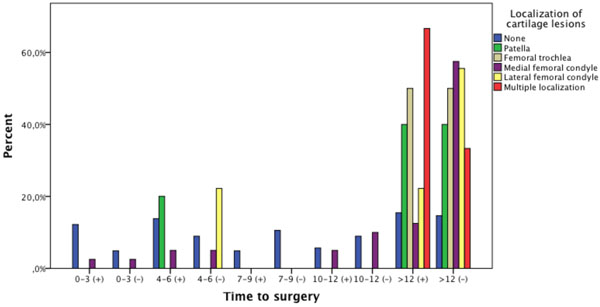
Distribution of chondral lesions in the patients according to time from initial trauma to surgery and sportive activity. (+) Restricted sportive activity, (-) continued sportive activity.
Details of the inclusion criteria.
| Age ‹ 50 years at time of surgery No associated injury to the medial collateral ligament, posterolateral complex or posterior cruciate ligament Isolated ACL injury in initial MRI No revision of reconstruction of the ACL No previous knee surgery |
List of restricted physical training activities.
| Basic Physical Training |
| Pushup |
| Sit up |
| Rope-climb |
| High-jump |
| Long-jump |
| Ladder exercise |
| 100 m sprint |
| 1600-2500 m run |
| Vault exercise |
| Cushion exercise |
| Combat Physical Training |
| Hurdle run |
| Chest to chest combat |
| 3 km run with rifle and equipment |
| 5 km run without rifle and equipment |
| 5 km run with rifle and equipment |
| Shooting target by running |
| Jump out and cringe from moving vehicle |
| Military pentathlon |
| Walk with skies and pallets |
| Mountaineering, nature sports and likewise sportive contests. |
Distribution of meniscal and chondral lesions according to time period and sportive activity before surgery. Patient number (n) and percentage (%).
| Patients Who Did Not Restricted Their Sportive Activity | p | Patients Who Restricted Their Sportive Activity | p | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A(0-3) | B(4-6) | C(7-9) | D(10-12) | A(0-3) | B(4-6) | C(7-9) | D(10-12) | ||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||||
| chondral lesion | no | 6 | 14,3 | 11 | 26,2 | 13 | 31 | 12 | 28,6 | 0,191 | 15 | 31,4 | 17 | 13,6 | 6 | 13,6 | 6 | 33,3 | 0,472 |
| yes | 1 | 11,1 | 4 | 44,4 | 0 | 0 | 4 | 44,4 | 1 | 16,7 | 3 | 50 | 0 | 0 | 2 | 33,3 | |||
| meniscal lesion | no | 3 | 16,7 | 7 | 38,9 | 5 | 27,8 | 3 | 16,7 | 0,390 | 5 | 29,4 | 5 | 29,4 | 3 | 17,6 | 4 | 23,5 | 0,481 |
| yes | 4 | 12,1 | 8 | 24,2 | 8 | 24,2 | 13 | 39,4 | 11 | 33,3 | 15 | 45,5 | 3 | 9,1 | 4 | 12,1 | |||
Fisher’s Exact Test.
DISCUSSION
Our aim was to determine the relationship of time period from injury to surgery with the incidence of meniscal and chondral injuries recorded at the time of surgical treatment for ACL tears. Also the effect of sportive activity restriction, grade of chondral lesions and their locations were also evaluated. Our findings show a significant increase in chondral injury of the knee in patients undergoing reconstruction of the ACL more than 12 months, also continuing sportive activity increases chondral injury incidence in this group. Some patients with ACL tear delays their treatment some refuses the surgical treatment. Some of the studies imply that delaying ACL reconstruction surgery causes additional meniscal and chondral lesions [5, 6]. Previous studies have revealed that meniscal and chondral lesions are associated with worse outcomes after late ACL reconstruction [6-8]. Although meniscal tears can occur at the time of ACL rupture subsequent meniscal injury is increased after ACL rupture secondary to abnormal loading and shear forces [9]. Some studies have shown a higher incidence of meniscal injury in the chronic ACL deficient knee [10, 11]. In a study which reviewed 5086 patients’ data they found an increasing incidence of medial meniscal tears and chondral injuries. They couldn’t state same increase in respect to lateral meniscus. Also they stated an increase of these injuries by a factor of six if surgery was delayed after 12 months [1]. A study found meniscal tear incidence % 27 in acutely injured ACL and % 90 in chronic ACL tears [12]. There is also data in literature that ACL reconstruction was protective against subsequent meniscal injury and decreases subsequent meniscal reoperation [5, 13, 14]. A retrospective study comparing ACL deficient knees and ACL reconstructed knees of army personnel showed the subsequent meniscus injury was two times higher in ACL deficient knees [15]. But in the prospective study authors didn’t find a difference in meniscal injury occurring in 56% of acute and 56% of chronically injured knees [16]. Our findings correlate with this study as there was no significant increase in meniscal lesions before or after 12 months (% 65.3 to % 76.5]. Also in addition, restricting or continuing sportive activity doesn’t change this finding statistically. Articular cartilage is a unique, biologically active tissue. Shift in the normal load bearing surfaces of the knee joint after ACL injury leads to progression of osteoarthritis due to cartilage damage [17]. Kinematics of the knee changes in chronically ACL deficient knee [18]. Persistent laxity results in increased shear stress and additional cartilage injury [17, 19]. Chondral lesion frequency is in between % 11 and % 45 in ACL tears [20, 21]. Studies imply when surgical time delays of chondral lesion frequency increases [9, 22-24]. In the chronic ACL deficient knee, additional chondral injury may be the result of repeated increased tibia-femoral translation. In a study authors stated ACL tear greater than 8 weeks and patient’s age are significant factors in medial compartment chondral pathology and delayed reconstruction may increase these injuries [2]. In a cohort study with 15783 patients authors stated that male gender, age, previous surgery and time from injury to surgery more than 12 months are as risk factors for full-thickness cartilage lesions in anterior cruciate ligament injured knees [25]. One study indicates the importance of time to surgery and they found reconstruction carried out in one year of injury was related with a very low incidence of degenerative change in the knee joint [26]. These findings correlates with our results as we showed that there is no significant difference in chondral injury incidence before 12 months even with smaller time scales. Incidence of meniscal and chondral injuries is not documented well in patients who did not restrict their sportive activities. In a study authors found higher incidence of chondral injuries in the group where patients didn’t restrict their daily activities [24]. Another study with 541 patients who underwent ACL reconstruction authors mentioned preoperative episodes of instability predicted medial meniscal tears. Also they stated male sex, sports injuries lesser than 6 weeks from surgery predicted medial meniscal tears [27]. We found a statistically significant increase in chondral injuries with the group who have more than 12 months injury time specially restricting sportive activity is very important to prevent chondral injury in this group. Also our work showed that with increasing time from initial trauma to surgery chondral lesion incidence and grade of these lesions increases. Interestingly we cannot state same result about meniscal injury. Therefore chondral injuries may be the main dilemma of the patients who had ACL reconstruction after 12 months and who didn’t restrict their sportive activity. Some recent studies showed male gender as a risk factor of additional chondral injuries [25, 27]. Consequently all male population of our study limits to generalize these findings to similar populations. Also restriction of patient numbers when analyzing subgroups is another limitation of our study.
CONCLUSION
The results indicate that the time of injury and continuing sportive activity before surgery significantly increases the chondral lesions. When time from initial trauma to surgery increases chondral lesions and grade of these lesions increases. Time of injury and restricting sportive activity is very important to prevent chondral injury in delayed anterior cruciate ligament reconstruction.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The data discussed in this manuscript were partially presented as a poster presentation at the 16th ESSKA Congress 14- 17 May 2014.


