All published articles of this journal are available on ScienceDirect.
Extended Long-Term (5 Years) Outcomes of Triangle Tilt Surgery in Obstetric Brachial Plexus Injury
Abstract
Objective:
We evaluated the "extended" long-term (5 years) functional outcomes in obstetric brachial plexus injury (OBPI) patients, who underwent triangle tilt surgery between February 2005 and January 2008.
Methods:
Twenty two children (9 girls and 13 boys, mean age at surgery was 5.8 years; ranging 2.1-11.8 years old), who initially presented with medial rotation contracture and scapula deformity secondary to obstetric brachial plexus injury were included in this study. Functional movements were evaluated pre-operatively, and 5 years following triangle tilt surgery by modified Mallet scale.
Results:
Here, we report long-term (5 years) follow-up of triangle tilt surgery for 22 OBPI patients. Upper extremity functional movements such as, external rotation (2.5±0.6 to 4.1±0.8, p<0.0001), hand-to-spine (2.6±0.6 to 3.4±1.1, p<0.005), hand-to-neck (2.7±0.7 to 4.3±0.7, p<0.0001), hand-to-mouth (2.3±0.9 (92º±33) to 4.2±0.5 (21º±16), p<0.0001), and supination (2.6±1.1 (-8.2º ±51) to 4.1±0.7 (61±32)) were significantly improved (p<0.0001), and maintained over the extended long-term (5 years). Total modified Mallet functional score was also shown to improve from 14.1±2.7 to 20.3±2.5.
Conclusions:
The triangle tilt surgery improved all shoulder functions significantly, and maintained over the extended long-term (5 years) in these patients.
INTRODUCTION
Recent published epidemiological study identified an incidence of about 0.15% obstetric brachial plexus injury in live births in USA [1]. Despite the advances in technology, the rate of occurrence has remained stable [2]. Although, most injuries are transient and recover function spontaneously within the 3 months of life, some result in prolonged and persistent disability. Traditional approaches to treat OBPI are nerve and tendon transfers, muscle releases, axillary nerve decompression and derotational osteotomy of the humerus [3-11]. These surgical procedures may lead to better shoulder abduction and flexion, and improve the resting position of the arm. However, these procedures may not address the glenohumeral dysplasia and joint incongruity, which impair the bone growth and development [12]. The triangle tilt surgery was developed by the surgeon (RKN) to mainly correct this bony deformity and shown to have a high success rate [13-23].
The short (1 year), and long-term (2 years) benefits of triangle tilt surgery in OBPI patients were previously demonstrated by examination of their radiological reports as well as the modified Mallet functional scale [13, 19]. Now, we evaluated the "extended" long-term functional outcomes (5 years) of triangle tilt in 22 OBPI patients, who underwent this surgery between February 2005 and January 2008 at our institute.
METHODS AND PATIENTS
266 OBPI patients have undergone triangle tilt surgery between February 2005 and January 2008, at our institute. 22 patients were included in this study, who have completed 5-year follow-up. The brachial plexus injuries involved C5-C6 nerve roots in 11 patients, C5-C7 nerve roots in 7 patients, and C5-C8 or C5-T1 nerve roots in 4 patients. All the patients in this study had already undergone the modified Quad soft tissue release procedure [11] to improve their shoulder abduction. Some of the patients have had primary nerve surgery, and other secondary procedures, such as posterior glenohumeral capsulorrhaphy, and humeral osteotomy at other institutions. However, these procedures failed to resolve the shoulder deformity in these patients. The medial rotation contracture was still persistent in these patients, even after the patients have undergone one or two of the above mentioned procedures, physiotherapy and/or splinting.
The triangle tilt operative technique includes osteotomies of the clavicle, neck of the acromion and scapula in order to release the distal acromioclavicular triangle and allow it to reorient itself in a more neutral position into the glenoid [13-23]. The lead author and surgeon, who has over 17 years of experience with obstetric brachial plexus injury, performed all the surgical procedures, and evaluated the pre- and postoperative shoulder functions of these patients in the clinic. Further, the trained scientist (independent of the surgeon) also scored modified Mallet from photo/video records of these patients [24].
Modified Mallet functional evaluation was performed for five-year follow-up (at the mean time of 62 months,), and these data were compared statistically with pre-operative data.
The paired student’s t-test statistics was applied to compare the pre- and post-triangle tilt mean Mallet scores using the Analyze it plug in (Leeds, UK) for Microsoft Excel 2003. A value of p< 0.05 was considered statistically significant.
RESULTS
There was an overall significant upper extremity functional improvements (Table 1), and significant difference in total modified Mallet score following 5-year after triangle tilt surgery in these patients (Fig. 1). Pre- and post-operative hand to mouth, and supination angles were compared statistically and reported (Figs. 2, 3). Modified Mallet functional movements and apparent supination were evaluated for each patient and reported (Figs. 4, 5).
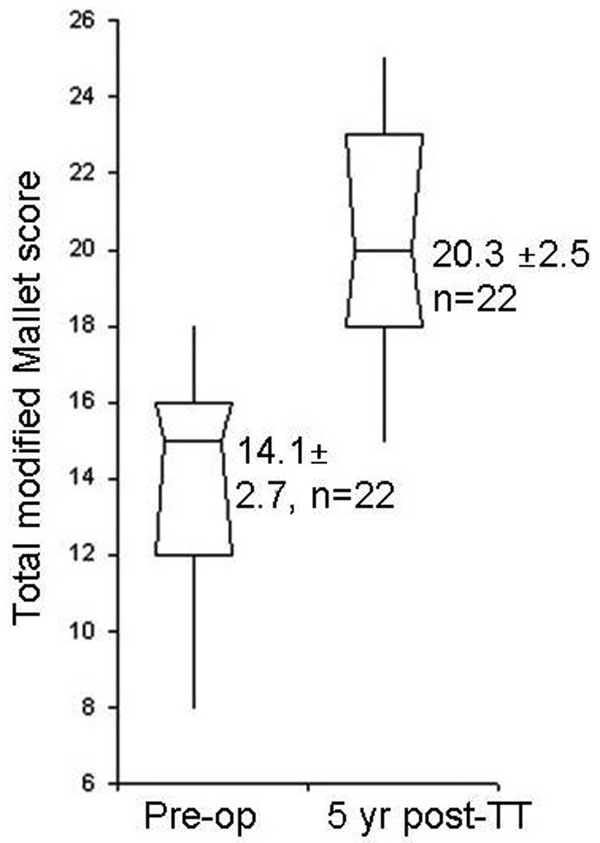
Comparison of total modified Mallet score pre-operatively and five-year follow-up of triangle tilt surgery in 22 OBPI patients. p < 0.0001.
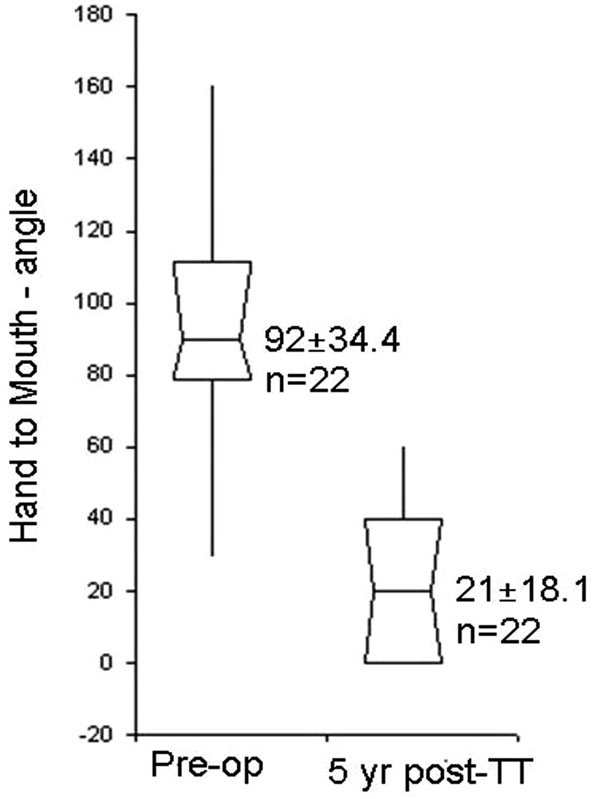
Comparison of hand-to-mouth movement (angle) pre-operatively and five-year follow-up of triangle tilt surgery in 22 OBPI patients. p < 0.0001.
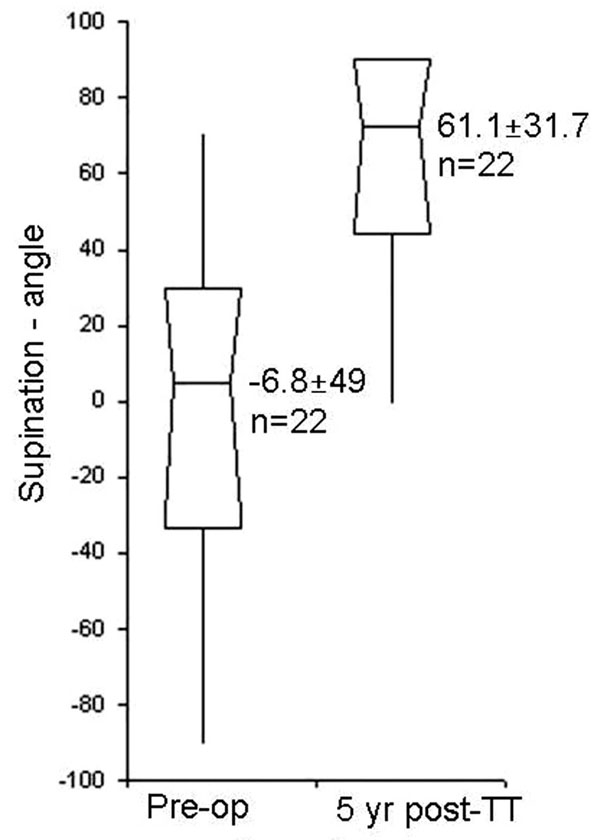
Comparison of supination angle pre-operatively and five-year follow-up of triangle tilt surgery in 22 OBPI patients. p < 0.0001.

Comparison of pre- and post-operative hand-to-mouth movement in OBPI patients. Preoperative photograph of a 5.8-year old girl (A), 2-year-old boy (C), and a 4.2-year-old boy (E), demonstrating limitation of hand-to-mouth function with typical bugler’s position. Same patients, 59, 61 and 62 months after triangle tilt surgery respectively (B, D and F).
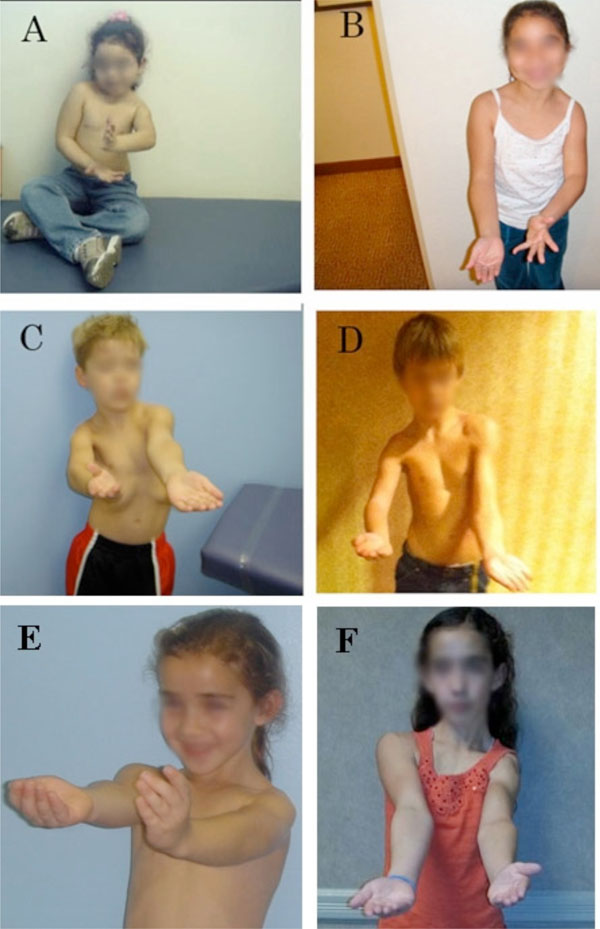
Comparison of pre- and post-operative apparent supination in OBPI patients. Preoperative photograph of a 5.8-year old girl (a), a 4.2 year old boy (C) and a 6.2 year old girl (E), demonstrating limitation of apparent supination; same patients, 59, 62 and 60 months after triangle tilt surgery respectively (B, D and F).
Comparison of Modified Mallet Score in OBPI Patients in Long-Term (5 Years) Follow-Up of Triangle Tilt Surgery
** P value <0.005 (N=22)
* P value < 0.0001. (N = 22).
Upper extremity functional movements such as, external rotation (2.5±0.6 to 4.1±0.8, p<0.0001), hand-to-spine (2.5±0.6 to 3.4±1.1, p<0.005), hand-to-neck (2.7±0.7 to 4.3±0.7, p<0.0001), hand-to-mouth (2.3±0.9 (92º±33) to 4.2±0.5 (21º±16), p<0.0001), and supination (2.6±1.1 (-8.2º ±51) to 4.1±0.7 (61±32)) were significantly improved (p<0.0001), and maintained over the extended long-term (5 years). Total modified Mallet functional score was also shown to improve from 14.1±2.7 to 20.3±2.5 (p<0.0001).
DISCUSSION
We have previously reported short-term (1 year) follow-up of triangle tilt surgery for 44 patients [13], and 2 year follow-up of this surgery for 61 patients [19]. Further, we report here extended long-term follow-up (5 years) of triangle tilt procedure for 22 patients.
All the patients included in this study had undergone a modified Quad procedure [11] prior to triangle tilt surgery, which significantly improved their shoulder abduction to a mean score of 4.3 or about 160°. Modified Quad procedure releases the soft tissue contractures, which greatly improves the shoulder abduction and flexion, but does not correct the glenohumeral joint incongruence. In order to address this, the triangle tilt [13-23], a unique bony surgical intervention has been performed on these patients. This procedure realigns the glenohumeral joint, and improves the other upper extremity functions such as external rotation, hand to mouth, and neck [13-23].
Though several surgical procedures have been explored in an effort to treat abnormal shoulder development of these OBPI patients [25, 26], only a few procedures are successful in long-term of improvements both functionally and anatomically. Investigators in this field demonstrated the use of tendon transfer/lengthening, and open reduction to improve shoulder functions and glenohumeral deformity in selected OBPI patients with mild-to-moderate glenohumeral deformity with posterior subluxation [25].
Patients (2 to 12 years) treated with triangle tilt surgery in our present study were with more severe initial deformity of the glenohumeral joint according to the grading criteria [27, 28]. Posterior subluxation ranged from –60% to 40% and glenoid version ranged from –75° to –8° for affected shoulders preoperatively (data not shown). After the triangle tilt surgery, patients gained remarkable functional improvements (Table 1 and Figs. 1-5), even for those with more severely deformed glenohumeral joints, which is consistent with our previously published study [13]. These functional movements continued to improve as shown in Figs. (1-5) in 5 year follow-up, when compared to the short term follow-up [13], and further these functions were maintained over long-term. We have demonstrated earlier that these patients also showed significant glenohumeral remodeling or reservation of glenoid congruence [19] in 2 year (over a mean time of 27 months) follow-up of triangle tilt surgery.
CONCLUSIONS
The triangle tilt surgery improved all shoulder functions highly significantly in 5-year follow-up, and further the functions were maintained over extended time in these patients.
AUTHORS’ CONTRIBUTIONS
RKN designed the study, performed the surgeries, and revised the manuscript. CS carried out the measurements, performed the statistical analysis and wrote the manuscript. Both authors read and approved the final manuscript.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


