RESEARCH ARTICLE
Multiple Acetabular Revisions in THA - Poor Outcome Despite Maximum Effort
O Bischel*, 1, JB Seeger1, M Krüge2, BG Bitsch2
Article Information
Identifiers and Pagination:
Year: 2012Volume: 6
First Page: 488
Last Page: 494
Publisher ID: TOORTHJ-6-488
DOI: 10.2174/1874325001206010488
Article History:
Received Date: 5/8/2012Revision Received Date: 3/10/2012
Acceptance Date: 4/10/2012
Electronic publication date: 16/11/2012
Collection year: 2012

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
A consecutive series of 52 acetabular revisions was evaluated retrospectively. Inclusion criteria for all patients were at least one former exchange of the acetabular component. Reconstruction was performed with reliable techniques and implants other than extensively porous coated device (e.g. tantalum). The mean follow up was 5.63 (0.01-14.05) years. Cumulative survival at 14.05 years with removal of the acetabular component due to aseptic loosening or the worst case criterion (removal of the acetabular component for any cause and/or lost to follow-up) as the end point was 66.38 (95 % C.-I.: 47.80-84.96) % and 58.42 (95 % C.-I.: 41.01-75.83) %, respectively. The cumulative survival rate with mechanical failure of the acetabular reconstruction as the endpoint was significantly lower in patients with two or more previous revisions in comparison to those with only one former procedure (log rank test: p=0,0112 respectively). The mean Merle d’Aubignée-score improved from 7.3 (0-14) preoperatively to 10.6 (0-17) points at latest follow up examination.
Survival of acetabular reconstructions with common techniques and implants is decreasing with the number of previous revisions. This may cause major concerns with regard to the rising number of patients needing repeated revisions. Maximizing durability of primary THA, precise preoperative planning as well as improved techniques and implants for revision may decrease this problem in the long term.
BACKGROUND AND PURPOSE
Although hip arthroplasty has become one of the most reliable and successful procedures in orthopaedics, durability of joint reconstruction still is limited. As indication for primary joint replacement was widened constantly and due to the demographic change, the number of revisions is rising steadily. Projections for the next three decades based on actual data causes major concerns not only with regard to the large quantity of revisions but also to resulting costs [1, 2].
During the last three decades a great variety of implants and operative techniques for revision arthroplasty have been developed and some procedures established reliable results in medium to long term follow-up studies [3-9]. Patients after repeated exchange of implants undergoing a further revision may represent the most challenging cases. Durability of joint reconstruction is not only limited through excessive bone defects and resulting technical difficulties. Defect regeneration and implant integration is hindered by thinning and sclerosis of host bone stock.
There is no data available for a consecutive series of acetabular revisions in patients with more than one former acetabular replacement procedure. The aim of this study was to evaluate whether survival and functional outcome of acetabular revision procedures with established implants and techniques is influenced by the number of revisions.
METHODS
Patients and Operative Technique
A consecutive series of 52 acetabular hip revision arthroplasties in 39 patients performed in our institution between 1994 and 2005 was evaluated. 32 patients were female and seven were male, one was treated on both sides. All included cases had at least one former revision of the acetabular component (Table 1). Consecutive acetabular revisions on the same side due to failure were performed in nine patients (seven patients had two and two had three further revisions). All revisions were included in the study.
Summary
| Patients | ||
|---|---|---|
| No. of cases | N=52 | |
| Mean age at index operation (range) in years | 65.9 (38.4-89.0) | |
| Mean follow up in years | 5.63 (0.01-14.05) | |
| Indication for primary THA | ||
| Primary osteoarthritis (OA) | 21 | |
| Secondary OA due to dysplasia | 17 | |
| Secondary OA after trauma | 8 | |
| Secondary OA due to avasc. necrosis/Perthes | 2 | |
| Secondary OA due to rheumatism | 4 | |
| Indication for index operation | ||
| Aseptic loosening | 42 | |
| Septic revision (one-stage/two-stage) | 7 (2/5) | |
| Recurrent dislocation | 2 | |
| Breakage of acetabular component | 1 | |
| Revised components |
Acetabulum Acetabulum and femur |
29 23 |
| Side |
Left Right |
20 32 |
| No. of acetabular revisions (index operation included) |
2nd 3rd 4th 5th 6th |
27 11 8 5 1 |
| Methods | ||
| Surgical approach | Anterior | 5 |
| Transgluteal | 39 | |
| Transtrochanteric | 8 | |
| Acetabular component | Cemented PE | 8 |
| Roof Reinforcement Ring | 29 | |
| Reconstruction Ring | 15 | |
| Allogenous bone transplant | None | 8 |
| Massive | 2 | |
| Massive and Morselized | 12 | |
| Morselized | 30 | |
| Results: function and defect situation | ||
| Merle d’Aubignée-score (range) in points | Preop. latest follow-up |
7.3 (0-14) 10.6 (0-17) |
| Pain (range) in points | Preop. latest follow-up |
1.4 (0-6) 3.4 (0-6) |
| Movement (range) in points | Preop. latest follow-up |
4.4 (0-6) 5.0 (0-6) |
| Mobility (range) in points | Preop. latest follow-up |
1.5 (0-5) 2.2 (0-5) |
| No. of cases with ‘poor/tolerable/good’ Merle-Score (<9, 9-14, >14 pts.) | Preop. latest follow-up |
32/20/ 0 13/31/8 |
| Bone defect at latest follow-up (no. of cases) |
Increasing Constant Partial restoration Complete |
12 13 13 14 |
Reconstruction was done after removal of acetabular hardware with use of common implants and techniques (cemented low profile PE-cups, Mueller or Ganz roof reinforcement rings, Schneider Burch or Contour reconstruction rings) with or without frozen, non-irradiated allogenous bone grafts (Table 1). Metal wire mesh for coverage of a central acetabular defect was used in two hips; one in combination with morselized bone graft and an AR, the other with a cemented PE cup.
Indication for primary THA and index operation and the number of revised acetabular and/or femoral components are summarized in table 1. Isolated revision of a failed femoral component was not performed after index operation. Radiologically all stems remained stable until latest follow-up.
All operations were performed by 12 surgeons. 36 hips were revised by four surgeons who did more than five procedures in this collective. All patients were placed in supine position.
All patients were evaluated clinically and radiologically. The mean follow-up period was 5.61 (0.01-14.05) years with the most recent follow-up, removal of the acetabular component for any cause or death as the end point (Table 1).
All clinical and radiological evaluation was performed by the same author. Various radiographic measurements were made as MRI and/or CT scans and X-ray films were available for all patients pre-, postoperatively and during follow-up. According to three common classification systems, only plane radiographs (a-p and lateral views) were used for preoperative assessment of the defect type (Table 2) [10-12]. Intraoperative description of the bone defect was also assessed for central, ventral, cranial and/or dorsal defects. A division of the deficiency into cavitary/contained, segmental/uncontained or combined defect was done. Quantitative radiographic determination of bone defect was performed preoperatively, immediately post-operatively and at latest follow-up. The latest follow-up radiographs were compared to post-operative x-rays for any change in bone deficiency. Development of bone defect during follow up was rated as ‘increasing’, ‘constant’ and ‘partial’ or ‘complete’ osseous restoration.
Bone Defect Classification (No. of Cases)
| Paprosky | 1 | 2A | 2B | 2C | 3A | 3B | ||||||||||
| No. | 1 | 3 | 6 | 10 | 10 | 22 | ||||||||||
| D’Antonio/AAOS | 0 | I | II | III | IV | IVa | IVb | |||||||||
| No. | 0 | 8 | 11 | 29 | 4 | 0 | 4 | |||||||||
| Saleh | I | II | III | IV | V | |||||||||||
| No. | 2 | 15 | 13 | 18 | 4 | |||||||||||
Allografts were assessed for incorporation in host bone as evidenced by trabecular bridging of the host-graft interface. Breakdown of the transplanted bone or a clear reduction of density was defined as non-integration of the graft and bone resorption.
Pre- and postoperative functional assessment was done using the Merle d’Aubignée-score. Statistical analysis was performed with JMP® 8 for Windows (SAS Institute Inc., Cary, North Carolina). A survivorship-analysis with 95 % confidence intervals was performed using the Kaplan-Meier method with removal of the acetabular component/THA for mechanical failure/aseptic loosening, infection, instability and worst case (removal of the cup/THA for any cause and/or lost to follow up) as failure criteria. The p-value for non-crossing survival curves were calculated with the log-rank-test, for crossing curves with the Wilcoxon-test. Associations or correlations between a continuous and/or discrete variable were tested by Student’s T-, Paired T- or Chi square-test. All tests were two-sided and a p value ≤ 0.05 was considered significant.
RESULTS
No patient was lost to follow-up, data was available for all cases (n=52) until death, exclusion from the study or latest follow-up. Six patients died after a mean period of 6.50 (2.28-11.30) years after surgery. For analysis of the follow-up results, the data of these patients were included.
Complications and Minor Revisions without Removal of Acetabular Component
In one patient with a cavitary defect type II according to AAOS, fracture of the sclerotic bottom occurred during preparation of the acetabulum. A stable reconstruction was possible using massive and morselized allograft and an acetabular roof reinforcement ring with hook (AR). Dislocation of the hip occurred in seven cases. Until latest follow-up, six hips remained stable after closed reduction. Due to persisting instability despite exchange of the femoral head and acetabular liner four weeks before, replacement of a well fixed Ganz roof reinforcement ring by a Schneider-Burch reconstruction device was performed 0.74 years after index operation. The reconstruction stayed stable until latest follow-up.
Additional minor revisions without exchange of the THA occurred in four hips. One minor revision was necessary due to a fixed drain four days postoperatively. In this case, a two stage revision of THA was necessary due to low grade infection with removal of the hip arthroplasty 0.73 years postoperatively.
Functional Evaluation
The development of the Merle d’Aubignée-score and its underlying parameters (pain, movement, mobility) are summarized in (Table 1).
There was no significant difference neither between patients with only two compared to those with at least three revisions nor when the re-revisions were excluded with regard to pain, motion, mobility and Merle-score.
Radiographic Evaluation
Breakage of fixation screws of acetabular reconstructions during follow-up was visible in 15 cases. 13 of those migrated early and were revised due to aseptic loosening.
Preoperative defect classification is shown in table 2. Graft incorporation was visible in 33 of the 44 hips with allogenous bone transplants; complete ingrowth was stated in 17 cases. Two patients with bulk allograft alone showed no sign of incorporation. There was no significant relation between type of allograft (massive vs morselized) and incorporation (partial or complete vs non-integration).
Increasing bone defect at the acetabulum was stated in 12, constant situation in 13 and an at least partial restoration of the defect in 27 (complete in 14) cases (table 1). Age, gender, body weight, number of previous operations, diabetes, and use of non-steroidal anti-inflammatory drugs, cortisone, alcohol or nicotine showed no influence on defect regeneration and/or integration of allogenous bone transplants.
Survivorship Analysis
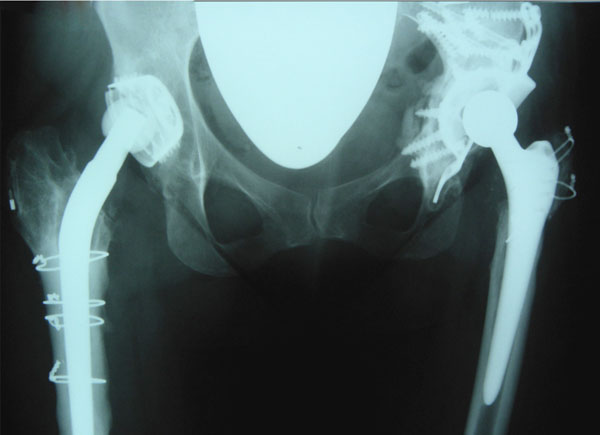
17 hips needed rerevision. Survival of the acetabular reconstruction with the worst case criterion (removal due to any cause and/or lost to follow-up) or revision due to aseptic loosening (11 cases) was 58.42 (95 % C.-I.: 41.01-75.83) % and 66.38 (95 % C.-I.: 47.80-84.96) % after 14.05 years respectively (Figs. 1, 2). Repositioning of the acetabular component was performed 0.74 years after index operation in one case with recurrent dislocation despite exchange of the acetabular liner and femoral head four weeks before. The survival rate with instability as failure criteria was 97.92 (95 % C.-I.: 93.88-100) % after 14.05 years.
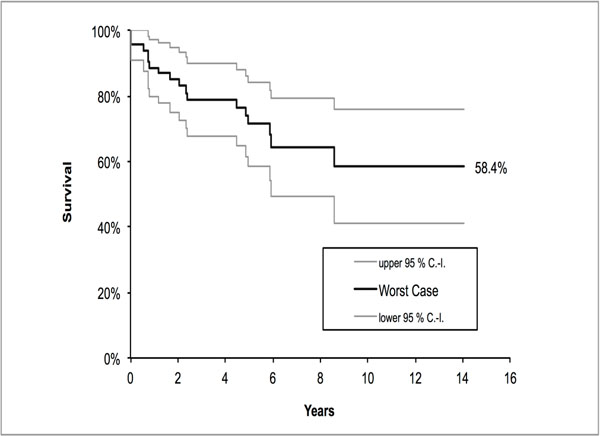 |
Fig. (1). Survivorship analysis: worst case criterion. |
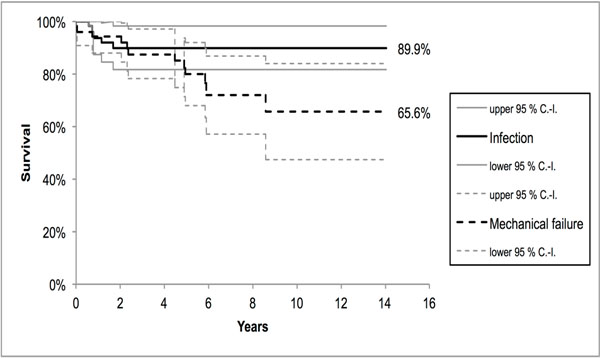 |
Fig. (2). Survivorship analysis: aseptic loosening and infection. |
Removal of the acetabular component due to infection was necessary in five cases implying a cumulative survival rate of 89.87 (95 % C.-I.: 41.01-75.83) % after 14.05 years. Although three of them had former revisions due to infection, Wilcoxon test for crossing survival curves was not significant for the groups ‘hips with former infection (n=13)’ vs ‘no former infection until index operation (n=39)’ (p=0.0550).
Cumulative survival of the different reconstructions with aseptic loosening as the end point was 100 % for the PE cups after 13.97 years, 58.77 (95 % C.-I.: 32.62-84.92) % for the AR’s after 11.30 years and 69.14 (95 % C.-I.: 38.25-100.00) % for RR’s after 14.05 years. There was no significant difference of the survival of the used cup types neither for the worst case criterion (AS vs RR: Wilcoxon test, p=0.4368; PE vs RR: log rank test, p=0.8912; PE vs AS: log rank test, p=0.7987) nor for aseptic loosening (AS vs RR: Wilcoxon test, p=0.3713; PE vs RR: log rank test, p=0.2432; PE vs AS: log rank test, p=0.1649).
With respect to defect classification systems, there was no correlation between the survival rates of the reconstruction and the grading of the different systems. Even a division within the systems (e.g. AAOS: type I vs II-IV; I+II vs III+IV or I-III vs IV; Paprosky: exclusion of the subtypes A, B, C and/or type 1 vs 2+3 or 1+2 vs 3) showed no tendency or significance.
There was no correlation between contained or uncontained defects and survival of the reconstruction. Survival was neither dependent on localization of a segmental defect (central, ventral, cranial or dorsal) nor on the number of concerned segments (only one, two, three or four deficient segments including the bottom).
Survival of the reconstruction with mechanical failure as the endpoint was significantly lower in patients with two or more previous revisions compared to those where the index operation was the second revision procedure (log rank test: p=0.0112). Cumulative survival with mechanical failure as the endpoint was 91.7 % after 14.05 years (2 out of 27 hips) versus 42.4 % after 10.92 years (9/25 hips) (Fig. 3).
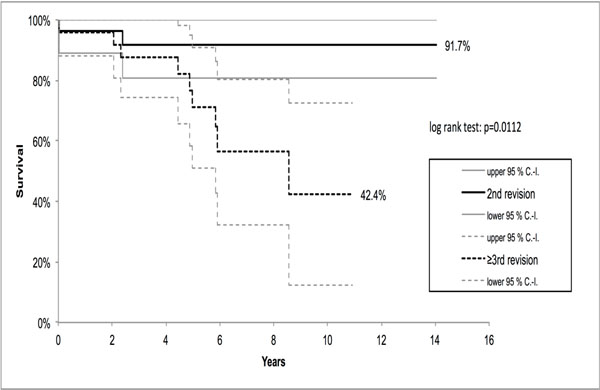 |
Fig. (3). Survivorship analysis (aseptic loosening): 2nd vs. at least 3rd revision at index operation. |
Interpretation
To our knowledge there is no data about a consecutive series of patients after repeated acetabular reconstruction in THA. There are two publications after cemented re-revisions without detailed information with respect to the acetabular site [13, 14].
Final functional result of the patients in this study has to be considered as poor, though improvement of function between preoperative status and level at latest follow-up examination in this series using the Merle d’Aubignée-score was comparable to other series [15, 16].
The only factor in this series showing significant influence on survival rate was the number of previous revisions. Cumulative survival in this series with removal of the implant due to mechanical failure as the endpoint was significantly lower in patients with only one former revision compared to those with two or more revisions.
Although this study showed no influence of quantitative bone defect on survival of the acetabular component, estimating bone deficiency and bone quality is mandatory for preoperative assessment of surgical procedure and choice of implant in revision THA [20]. Classification should not be descriptive but only relay on biomechanical aspects for individual assessment of the proceeding.
There are frequently used classifications for determination of acetabular bone loss [10, 12]. The systems described by Paprosky and Magnus and the one of Saleh et al., are based on x-ray evaluation of standard anteroposterior (pelvic) and lateral views of the hip. Although Saleh reports a high preoperative interobserver reliability and intraoperative validity of his graduation, underestimation of the defect may occur. Additional x-ray magnetic resonance or computer tomography revealed greater bone loss especially at the posterior wall and ischium compared to the estimation according to Paprosky and Magnus based on standard two plain radiographs [21-24]. Underestimation of a defect may lead to treatment by not suitable implants and consecutively to a high failure rate. Cementless cups, roof reinforcement rings or impaction grafting in combined medial deficiencies and/or uncontained defects at the posterior wall or even pelvic discontinuities revealed higher failure rates compared to the use of antiprotrusio cages in these cases [6, 9, 25]. Therefore, preoperative assessment of the quantity of bone loss using only plane radiographs may be too imprecise and consecutively, not sufficient for a suitable preoperative planning.
Not only the amount of bone loss may increase with the number of previous replacements but also quality and vitality of the remaining host bone stock is decreasing due to sclerosis (Figs. 4-8). High contact area to vital cancellous bone is necessary for ingrowth of cementless implants and/or bone transplants as well as for primary stability in cement fixation [26]. Breaking the sclerosis of the thin floor to get this presupposition is limited or impossible as acetabular or pelvic stability is weakened additionally. Although contact area between host bone and implant can be improved with custom made implants, influence of bone vitality may be one of the reasons for the great variety of survival rates of same implants in different studies [27-30].
 |
Fig. (4). Compared to standard views (Fig. 2) additional information with respect to the bony defect situation can be obtained with further radiological diagnostics. In this case, simple oblique iliac radiograph shows a highly deficient posterior wall, massive sclerosis of the host bone and defects at the bottom due to loosening and dislocation of screws. |
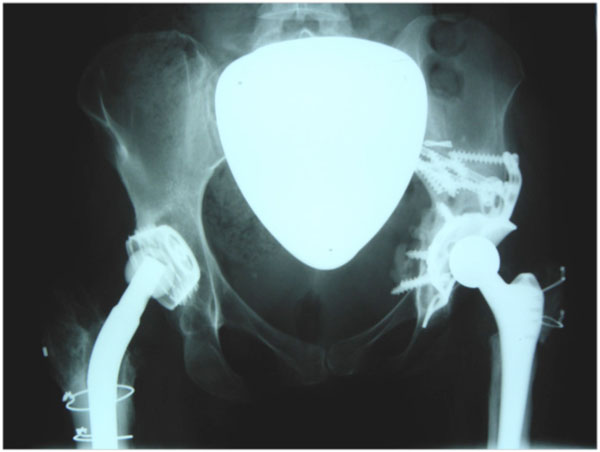 |
Fig. (6). 14 days postoperatively after a standard reconstruction by allogenous, morselized bone graft and reconstruction ring (antiprotrusio cage). |
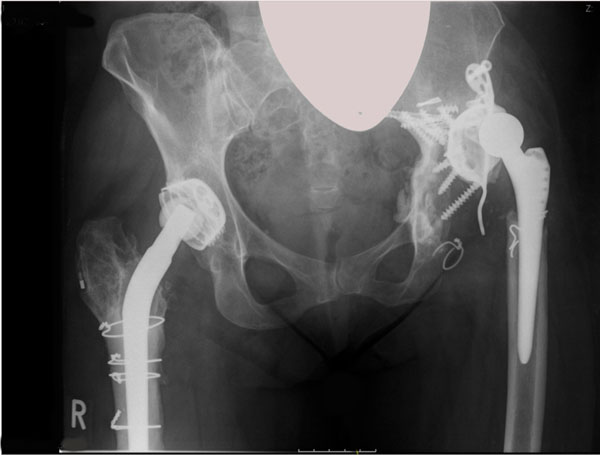 |
Fig. (8). Sudden dislocation occurred less than six years after the index operation leading to the 6th revision procedure due to immobility and pain. |
Overall survival rate after 14.05 years with the worst-case criterion (any cause and/or lost to follow up) or aseptic loosening as the end point was 58.42 % or 66.38 %. The revision rates due to aseptic loosening with regard to RR’s and AR’s were 58.77 % after 11.30 years and 69.14 % after 14.05 years and worse to comparable series published yet [3, 4, 9, 17-19]. The revision rate due to infection or instability was comparable to these series.
Neither the defect classification systems nor intraoperative defect description correlated with a mechanical failure of the reconstruction. In addition, general patients or specific intraoperative data showed no significant influence on survival of the reconstruction. Both findings were similar to those of Sembrano et al., [4].
Fig. (4). Compared to standard views (Fig. 2) additional information with respect to the bony defect situation can be obtained with further radiological diagnostics. In this case, simple oblique iliac radiograph shows a highly deficient posterior wall, massive sclerosis of the host bone and defects at the bottom due to loosening and dislocation of screws.
Even with use of more porous metal implants or augments instead of bone grafts with a proven high osteoinductivity, integration of these implants into thinned and sclerotic bone may be also limited although encouraging short to mid-term results in some studies has been already reported [16, 31-36]. Fragility of this material may cause wear debris and the high surface may be related with higher infection rates in the long run.
In general, biological reconstruction by use of autologous grafts for defect augmentation is favourable to allograft bone but host bone is limited. The rate of ingrowths of morselized allograft is higher compared to massive allografts but the latter are often necessary to get primary stability in non-contained defects [37-40]. One of the golden standards of acetabular revision in case of non-contained bone defects is the use of allogenous bone graft and specific revision devices like roof reinforcement rings or antiprotrusio cages [3, 4, 9, 17, 18, 25, 41]. Limited survival of these reconstructions also is related to none integration of allograft into host bone. Bone ingrowth can be enhanced by osteoinduction. The use of stem cells in combination with allograft bone may improve incorporation and therefore survival of the implant [42]. In-vitro and animal studies with biogenetic agents like osteogenetic proteins or bone morphogenetic protein have shown advanced integration but clinical data is missing [43].
CONCLUSION
Patients presenting with repeated implant failure in THA are demanding not only with respect to the rising number. Although this study has some limitations, it is the first investigation dealing with a consecutive series of patients undergoing acetabular revision for at least the second time within a mid- to long-term follow-up period.
Functional outcome in this series is poor. Survival of acetabular reconstruction with contemporary techniques and implants is very limited and decreasing with the number of previous revisions. There was a significantly lower survival of acetabular reconstruction in patients with two or more former revisions compared to patients with only one previous acetabular replacement procedure.
Although very promising short term data with more porous metal devices exist, future examination and long term follow-up studies in a large number of patients may give definitive answer whether these implant generation will give better results especially in these most challenging patients.
CONTRIBUTIONS OF AUTHORS
Each of the authors hereby transfers, assigns and otherwise conveys to the journal all right, title and interest in the work, including but not limited to any and all copyrights therein held by each undersigned author.
Each of the authors hereby warrants, represents and covenants that each of the authors has read and approved the final manuscript or version of the work; the work is original.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.