All published articles of this journal are available on ScienceDirect.
Post-Traumatic Malunion of the Proximal Phalanx of the Finger. Medium-Term Results in 24 Cases Treated by “In Situ” Osteotomy
Abstract
We report the clinical and radiographic medium-term results obtained for 20 patients (24 fingers) treated surgically for post-traumatic malunion of the proximal phalanx of the finger. In all cases we performed a corrective osteoclasia or osteotomy at the site of malunion, followed by miniplate and screw fixation or by screw fixation only. The corrective osteoclasia was performed when malalignment was addressed within six weeks after injury. Two patients who had two fractures underwent additional surgery (tenolysis and/or capsulolysis) to improve function and ROM. At the final follow-up, at a mean of 24 months after corrective surgery, good or excellent clinical and radiographic results were obtained in all the patients. The pseudoclaw deformity disappeared in all cases in which a volar angulation deformity was present. An average improvement of about 30% in the range of motion of the MP and PIP joints was observed; only 4 patients complained of mild pain at the maximum degrees of articular excursion of the MP and PIP joints. All the patients presented an improvement in grip strength. The mean DASH score in our series was 5 points. In two of the four cases treated by an intra-articular corrective osteotomy, mild radiographic signs of osteoarthritis at the MP joint were present. The data for this study confirm that “in situ” osteotomy stabilized by miniplates and/or screws is an effective procedure to correct post-traumatic malunions of the proximal phalanges of the fingers.
INTRODUCTION
Post-traumatic malunion of the proximal phalanx of the fingers can cause cosmetic deformity and impairment of hand function. When functional disability is severe, surgical correction is mandatory. Reports of corrective osteotomy are quite rare and often limited to a very small number of cases with a short follow-up [1-6]. Only Buchler et al. [7] reported an historical cohort study of 59 procedures in 57 patients who had corrective phalangeal osteotomies for post-traumatic malunion of the phalanges in the hand.
In this retrospective study, we report the medium-term results of 24 procedures in 20 patients operated on for malunion of the proximal phalanx of the finger by a corrective osteoclasia or osteotomy with stable internal fixation. The corrective osteoclasia was performed in the10 cases in which malalignment was addressed within six weeks after injury. In the other 14 cases, a corrective osteotomy at the site of the malunion was performed.
MATERIALS AND METHODS
Between January 2003 and January 2008, 20 patients (24 fingers) with a malunion of the proximal phalanx of the hand underwent surgical correction at our Department. The original treatment, performed in all patients in another hospital, was conservative in 16 fingers and operative in 8, by percutaneous osteosynthesis. In all the patients, only one hand was involved. There were 16 males and 4 females, and the average age of the patients at the time of the fracture was 34 years (range 20-41). Sixteen patients (18 fingers) were treated on the right side while 4 patients (6 fingers), on the left (Table 1). The fifth finger was involved in 8 cases, the fourth in 7, the third in 5 and the second in 4. In 14 cases, the fracture line presented a transversal course near the base of the phalanx, in 6 cases an oblique diaphyseal fracture was present, while in 4 fractures, the articular surface of the base of the phalanx was affected. An average of 120 days (range 10 days-6 months) had elapsed between the initial treatment performed in another hospital and our treatment. In 14 cases in which an extra-articular fracture of the base of the proximal phalanx was present at diagnosis, we observed only a volar angulation deformity in 10 cases, in 2 cases a volar angulation deformity associated with rotation and in 2 other cases a volar angulation deformity associated with deviation. In all of these 14 cases, a pseudoclaw deformity was present. Of the 6 cases with a diaphyseal fracture, 2 showed only a rotation deformity, 2 cases rotation and volar angulation and 2 cases only a shortening deformity, with a bony spike that limited PIP joint flexion. All of the remaining 4 cases, with an intra-articular fracture of the base of the phalanx, showed an articular surface incongruency.
Demographic Data and Treatment Performed
| Patients (fingers) | 20 (24) |
| Males/females | 16/4 |
| Side (patients/fingers) | 16/18 right – 4/6 left |
| Mean age at trauma (range) | 34 years (range 20-41). |
| Previous treatment performed in another hospital (conservative/surgical) | 16/8 |
| Treatment (osteoclasia/osteotomy) | 10/14 |
| Surgical devices (only screws/miniplates) | 6/18 |
All the patients were treated surgically. The surgical approach was lateral in 20 cases and dorsal in 4, when a malunited articular fracture was present. A corrective osteoclasia of the phalanx at the level of the fracture was done within 6 weeks after initial treatment in 5 cases that showed only volar angulation, in 3 cases that presented volar angulation and malrotation and in 2 cases that showed volar angulation and deviation. In the other 14 cases, we performed a corrective osteotomy because more than 6 weeks had elapsed after initial treatment. We performed a closing wedge osteotomy in 5 cases of volar angulation deformity and 1 case of volar angulation with rotation deformity. In 2 cases of rotation deformity, a rotational osteotomy was performed. In the 2 cases of shortening of the phalanx, we performed a corrective osteotomy with removal of the bony spike. In 4 cases with articular incongruency, we performed a corrective osteotomy of the articular surface of the base of the phalanx. In 6 cases internal fixation was done with screws, while in 18 cases with miniplates and screws. We used screws only when osteoclasia was performed and the refracture line was oblique or spiroid; whereas we used miniplates in all other cases (Table 1). Active assisted and passive mobilization of the metacarpophalangeal and interphalangeal joints was allowed in all patients immediately after the operation. Two patients underwent additional surgery (tenolysisis and/or capsulolysis) to improve function and ROM, performed at an average of 4 months after osteotomy. In these cases only, the plates and screws were removed during the aforesaid operation.
RESULTS
The clinical evaluation performed pre-operatively revealed in all cases a deformity of the finger, a limitation of the range of motion of the PIP and MP joints, and a reduction in grip strength of the hand, present to a varying extent. Before surgery, all the patients underwent an accurate radiographic study, including standard A-P, lateral and oblique projections.
At follow-up, which took place at a mean of 24 months (range 13-32) after surgery, we evaluated the clinical and radiographic correction of the deformity, the improvement in the range of motion and grip strength of the hand, and the patient’s satisfaction. Functional results were evaluated by the DASH (Disability of the Arm, Shoulder and Hand) questionnaire. Grip strength was measured with a Jamar dynamometer (Lafayette Instrument, Lafayette, IN, USA).
There were no perioperative complications. The osteoclasias and osteotomies were radiographically united an average of 8 weeks after surgery (range 5-9). At the final follow-up, in the 14 cases treated for extra-articular malunion of the base of the proximal phalanx, clinical and radiographic evaluations showed that all the deformities (volar angulation, rotation and deviation) were corrected well (Fig. 1), and the pseudoclaw deformity of the affected finger had disappeared. The final result in the 6 cases treated for a malunited diaphyseal fracture also showed full correction of the pre-operative deformity. In 2 of the 4 cases treated by an intra-articular corrective osteotomy for an articular fracture malalignment, the final x-rays revealed mild signs of osteoarthritis at the MP joint, but the clinical evaluation did not show a significant functional disability of the hand.
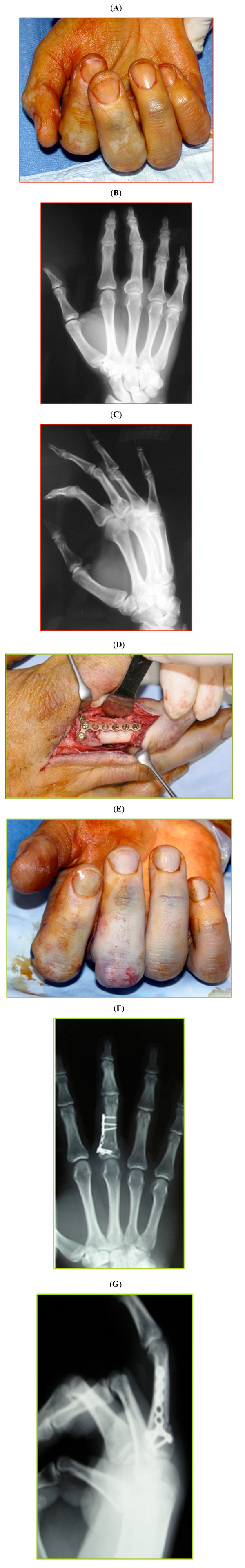
Forty-two year-old patient affected by a malunion of the proximal phalanx of the third finger of the right hand. A volar angulation associated with rotation deformity were present (A, B, C). A corrective in situ osteotomy of the phalanx fixed with plate and screws was performed, using a lateral approach (D). At the postoperative clinical and radiographic examinations, the deformity is corrected well, with a perfect alignment of the third finger (E, F, G).
Sixteen patients stated that they were very satisfied with the result obtained while 4, who reported mild pain, were moderately satisfied. Sixteen patients were asymptomatic, while 4 complained of mild pain during articular excursion of the MP and PIP joints (maximum excursion). In all cases, we observed an average improvement of 30% in the range of motion of the PIP and MP joints (range 25% to 45%). The mean DASH score in our series improved from 30 to 5 points. All the patients presented an improvement in grip strength of the hand, from an average of 40.5 to 56.5 in males and from an average of 20 to 31.5 in females (Table 2).
Results of the Treatment
| Pain | No Pain: 16 ; Mild Pain: 4 |
|---|---|
| Improvement in range of motion of PIP and MP joints at follow- up | Range 25%-45% (average 30%) |
| Improvement of DASH score at follow-up | From 30 to 5 points |
| Osteoarthritis | Mild in 2 cases |
| Mean improvement of grip strength at follow-up in males and females | From 40.5 to 56.5 (males) From 20 to 31.5 (females) |
DISCUSSION
Malunion is a frequent complication of fractures of the phalanges of the hand, especially when the proximal phalanx is involved [5, 8-10]. Malunion of the phalanx can cause functional and aesthetic problems such as crossing or scissoring of the fingers, disturbance of tendon balance such as extensor lag, and reduction of grip strength. Vahey et al. [11] performed a cadaver study on the effect of shortening and angulation of the proximal phalanx that cause extensor lag at the proximal interphalangeal joint. The authors noted the importance of reestablishing a correct bone-tendon relationship for proximal phalangeal fractures. Intra-articular malunion may cause capsular loosening or stiffness of the finger and osteoarthritis.
The surgical correction of post-traumatic malunion of the phalanges of the hand is often very complex. Reports of corrective osteotomy for malunited fractures of the phalanges of the hand are infrequent and often limited to small series with a short follow-up [2, 3, 5, 12]. Malunited fractures of the phalanges can be corrected at the site of malunion or at the base of the metacarpal. Surgeons still debate about these two methods. A rotational phalangeal malunion can be treated by a rotational osteotomy of the metacarpal bone [1]. A cadaver study demonstrated that one degree of metacarpal rotation provides about 0.7 degrees of phalangeal correction [13]. Botelheiro [3] and Menon [9] reported good results in a small series of patients treated with metacarpal osteotomy for phalangeal malunion. Metacarpal rotational osteotomy is technically easy and avoids adhesions of the tendons that surround the proximal phalanx, which can increase stiffness. However, a metacarpal rotational osteotomy may produce a “Z-deformity" if the angulation is associated with malrotation of the fracture. For this reason, we think, in agreement with other authors [7, 10, 14], that a corrective osteotomy of malunited fractures of the phalanges at the site of the original fractures better corrects a combined deformity, enabling the surgeon to simultaneously perform tenolysis and capsulolysis. In all our cases, we corrected the deformity at the site of the malunion and got good results without perioperative complications. The corrective osteoclasia or osteotomy was fixed by miniplates and screws or by screws only, obtaining in all cases a stable fixation, so as to allow active exercises of the hand immediately after surgery.
The timing of the corrective surgical procedure is very important. According to some authors [7, 15], if post-traumatic malunion is addressed within 10 weeks after injury, it is possible to perform a corrective osteoclasia, by mobilizing the fracture’s callus. We performed an osteoclasia in all cases in which malalignment was addressed nolater than 6 weeks after injury. Good clinical and radiographic results were obtained in all patients.
At follow-up, in 2 of the 4 articular fracture malunions treated by an intra-articular corrective osteotomy, mild radiographic signs of osteoarthritis at the MP joint were present, although the patients did not report impairment of their hand function. However, when a severe articular malunion is associated with early osteoarthritis of the MP joint, the treatment of choice is an arthrodesis or an arthroplasty [14].
The limitations of our study are that it is a retrospective study on a case series with a mixed population of fracture types.
CONCLUSION
We believe that fracture malunion of the phalanx, predictive of functional loss of the hand, should be corrected surgically as soon as possible. The deformity may be corrected well by an osteoclasia or osteotomy, performed at the malunion site. We agree with other authors [10] that “in situ” phalangeal osteotomy is a natural development with the possibility to use miniplates and screws, thereby permitting a stable fixation of the corrective osteotomy.
CONFLICT OF INTEREST
The author confirms that this article content has no conflict of interest.
PATIENT CONSENT
Declared none.
ACKNOWLEDGEMENTS
Declared none.


