All published articles of this journal are available on ScienceDirect.
Unilateral Lumbosacral Dislocation: Case Report and a Comprehensive Review
Abstract
Lumbosacral fracture-dislocation is a rare occurrence. There are more than 73 cases reported in the English literature. We report on the imaging findings and surgical treatment in a patient suffered of unilateral traumatic L5-S1 dislocation associated with severe disruption of the posterior ligamentous complex. The patient underwent open reduction and stabilization of L4-S1 vertebrae with posterior instrumentation system. Open reduction and internal fixation was mandatory as post-traumatic ligamentous insufficiency would lead to abnormal motion. Operative treatment managed to produce a solid arthrodesis and restore stability of the lumbosacral junction. Follow-up revealed excellent results. This study reports a rare injury of the lumbosacral junction, and the literature concerning this unusual condition is extensively reviewed.
INTRODUCTION
Unilateral facet dislocation is an injury classically localized to the mobile cervical spine [1]. However, its rarity in the lumbosacral spine is attributed to the orientation of the lumbar facet joints and the presence of robust muscular and capsuloligamentous structures that provide substantial stability in the lower lumbar region [2, 3].
Diagnosis of lumbosacral dislocation depends on an initial imaging study of good quality that demonstrates the abnormal relation of the lumbosacral facets [1]. Radiographs performed in the emergency room may hardly demonstrate subtle findings. The anteroposterior projection might show fractures of the ipsilateral lumbar transverse processes, lower lumbar scoliosis or signs of rotational malalignment at the lumbosacral junction including, widening of the interpedicular distance, rotational deformity of the spinous processes or increased interspinous distance. The lateral view may show an increased interspinous distance, a sharp kyphosis of L5 on S1, with anterior narrowing of the height of the disc space, malalignment of the facet joints or minimal anterior or posterior subluxation of L5 on S1 [4]. Computed tomography shows easily associated fractures [5-7]. The “naked facet” sign on the axial plane is indicative of facet dislocation. MRI examination allows identification of the herniated disc and degree of ligamentous disruption [8].
We report a case of unilateral traumatic L5-S1 dislocation, and the literature concerning this unusual condition is comprehensively reviewed.
CASE REPORT
An 18-year-old male was involved in a motorcycle accident, suffering an injury of the lumbar spine and a fracture of his left humerus. On admission the patient was confused, but awake and without history of loss of consciousness. Physical examination revealed abrasions to the patient’s left upper extremity. He complained of mild lumbosacral pain. Palpation of the spine revealed low lumbar tenderness with an echymosis in the lumbosacral region. There were no open wounds.
Neurological examination showed a 4+/5 muscular weakness in the left L5 root distribution. Rectal examination and perianal sensation were normal. Sensory examination revealed a decreased sensation in the lateral and plantar aspects of the left lower extremity. Hemodynamic and respiratory functions were normal.
Radiographic study:
Initial lumbosacral anteroposterior radiograph showed avulsion of the L5 left transverse process and obliquity of the lumbar spine on the sacrum, manifest as increase of the L5-S1 interspinous distance and as rotational deformity of the L5 spinous process (Fig. 1). Helical CT scan of the lumbosacral junction was performed using 3 mm axial slices from L4 to S1 level with reconstruction in the coronal and sagittal planes. This revealed unilateral left L5-S1 facet joint dislocation with perch of the articular facets and fracture of the L5 inferior process (the inferior part of it). On the right, fracture of the S1 superior articular facet was demonstrated with normal alignment of the facet joint (Figs. 2, 3a, b). Magnetic resonance imaging (MRI) of the lumbosacral spine confirmed the bone injuries and showed mild posterior subluxation of L5 on S1. Furthermore, it demonstrated disruption of the posterior ligamentous complex including the ligamentum flavum bilaterally, the interspinous and supraspinous ligaments and extensive high-signal intensity traumatic changes of the paraspinous musculature (Fig. 4). Epidural hematomas were noted causing compression of the dural sac. There was no evidence of disc disruption.

Preoperative anteroposterior radiograph. The L5-S1interspinous distance is increased and the interspinous line shows a stepoff at this level. Avulsion of the L5 left transverse process is identified (arrow). The left facet joint is not well delineated.

Axial CT image shows avulsion of the L5 left transverse process and the lateral half of the pedicle.
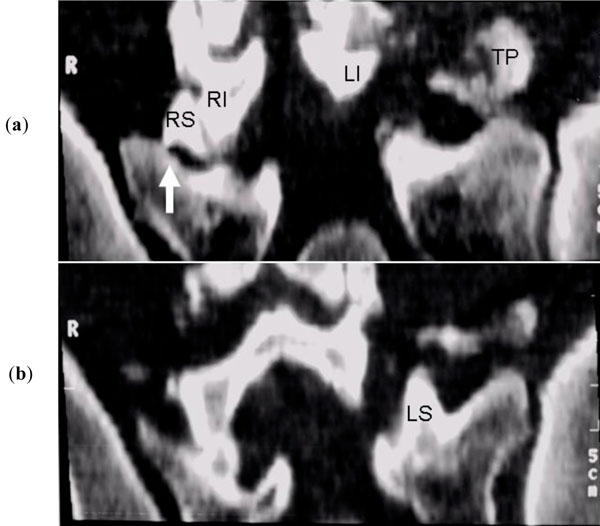
(a, b) CT oblique coronal reformatted sequential images demonstrate the fracture at the root of right superior facet (RS) (arrow), the normal right inferior facet (RI), the normal (not fractured) LS, the fractured left transverse process (TP). The inferior part of LI is not identified (comminuted).
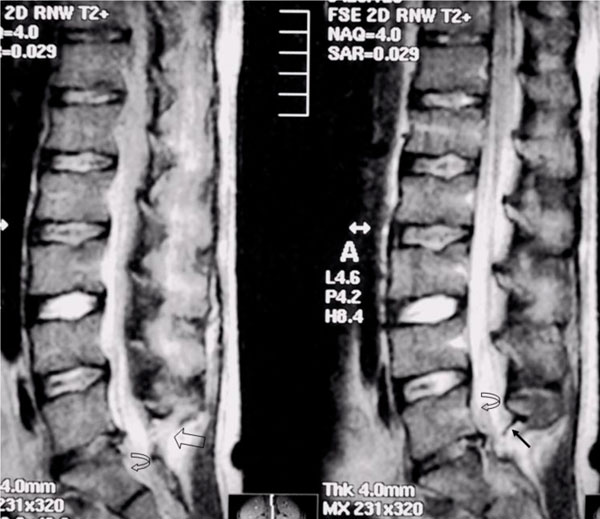
MRI of the lumbosacral spine. Sagittal T2-weighted midline and off-midline images showing epidural haematoma (curved arrow), extensive high-signal intensity changes in the posterior ligamentous complex (empty arrow) and discontinuity of the ligamentum flavum (straight arrow) suggestive of disruption. Notice mild posterior subluxation of L5 on S1.
The patient underwent surgery the next day through a posterior approach. Intra-operative findings of unilateral facet fracture-dislocation were revealed. The left articular capsule of L5-S1 was torn. A rotational deformity of the L5 in relation to the sacrum was noticed. Disruption of the posterior ligamentous complex was evident and confirmed the imaging findings. Vertical traction force on the spinous process of L5 vertebra by using a small periosteal elevator could not managed to restore the reduction, as the inferior process of the L5 vertebra was comminuted and thus, unable to serve as a block against deforming forces. An arthrodesis was performed from L4 to S1 vertebrae using titanium rods and screws. This solution seemed to be appropriate as it could reduce the L5 displacement by applying traction to the right pedicle screw positioned in L5 with bent rods placed between L4 and S1. It was unable to insert a screw at the L5 left pedicle because it was fractured, (Fig. 5a, b).

Anteroposterior (a) and lateral (b) postoperative radiographs.
The patient was upright on the second postoperative day after bracing. Currently, seventy-two months after the injury, the patient is free of symptoms and able to walk without any help.
DISCUSSION
Traumatic fracture-dislocation of L5 is a very uncommon injury. It can be easily missed, especially in multi trauma patients [9]. The lumbosacral joint is a solid and stable junction and that because of its increased inclination in the sagittal plane, the more vertical orientation of the facets and the presence of the powerful musculature and the ligamentum complexes [10]. Rupture of the iliolumbar ligamentum complex increase the flexion at the lumbosacral joint by 77%, as experimentally demonstrated by Leong et al [11].
An in depth review of the literature revealed that 57 of patients were men (78%) and 16 were women (22%) [12-52]. The average age was 27 years and this injury pattern has been described in patients as young as 5 years [13] to as old as 52 years [5, 23]. The causes of the injury were motor vehicle accidents in 34 cases (46.5%), falls from a height in 17 cases (23.3%), occupational injuries in 13 cases (17.8%), motor versus pedestrian in 3 cases (4.1%), sports related injuries in 3 cases (4.1%), 2 cases after an airplane (1.4%) and a helicopter crash (1.4%), respectively, and one case was a war related injury (1.4%). Fractures of the transverse processes were seen in 34 cases (46.5%) [1, 2, 4-6, 8, 10, 12, 13, 15, 17, 18, 21, 23, 24, 28, 31, 37, 38-43, 47, 49, 50, 52], and disk involvement at L5-S1 level was present in 12 cases (16.4%) [1, 4, 10, 19, 28, 30, 32, 35, 45, 49]. The ratio bilateral/unilateral fracture-dislocations were 1.1:1. Additional injuries in the other parts of the body included head injuries, abdominal injuries, femur fractures, clavicular fractures, and rib fractures.
Thirty-six patients (58%) had a neurological deficit at time of their admission. Twenty-six patients were presented with no neurological compromise [1-5, 15, 20, 21, 23, 31, 33, 36-38, 43, 44, 47-50] and no data has been given for the rest 11 patients [8, 17, 20, 23, 27], regarding neurological involvement. The occurrence of neuropathological complications is broadly similar. They include paraplegia (or paraparesis) [29, 43, 43], lumbar plexus lesions, hyposthesia or anesthesia in the lower extremities, and urine retention. The vast majority of the patients are complaining of severe low back pain. However, severe disability is unusual.
Forced hyperextension was the first proposed responsible mechanism for this type of injury [53]. However, most authors recently agree that these types of injuries are provoked from severe forces applied to the lumbar spine, shifting it forward on the immovable sacrum, while the lumbar spine and hips are flexed [13, 23, 24, 26, 48, 52]. The presence of a presumed rotary component in the above mentioned mechanism leads to a dislocation as demonstrated in a cadaveric experimental study by Roaf [54].
Good quality initial radiographs are important for the diagnosis, as emergency room radiographs are frequently inadequate. Transverse processes fractures are a frequent radiologic sign [4, 10]. CT scan and MRI imaging studies are of great help and easily reveal associated fractures, soft tissue and disc disruptions as well as secondary spondylolysthesis.
Aihara et al, proposed a classification system by reviewing 57 cases [9]. They classified the injury into five types: type 1, unilateral lumbosacral facet-dislocation with or without facet fracture; type 2, bilateral lumbosacral facet-dislocation with or without facet fracture; type 3, unilateral lumbosacral facet-dislocation and contralateral lumbosacral facet fracture; type 4, dislocation of the body of L5 with bilateral fracture of the pars interarticularis; and type 5, dislocation of the body of L5 with fracture of the body and/or pedicle, with or without injury of the lamina and/or facet. The presented injury was judged to be type 3 as unilateral lumbosacral facet dislocation and contralateral lumbosacral facet fracture were present.
Despite the type of injury, fracture-dislocation of the lumbosacral junction is a three-column injury. Thus, the choice of the type of treatment is essential. Although reported success with conservative treatment has been published [2, 3, 14, 16, 21, 23, 26, 38, 40, 50], currently, this choice of treatment is not accepted. Open reduction internal fixation and bone grafting is postulated by many authors [18, 34, 37, 49] and pedicle screw instrumentation is the preferred method of choice [8, 17, 20]. Surgical intervention will ensure normal anatomical relationships, and late detoriation prevention. Aihara et al. [9], recommended anterior lumbar interbody fusion after posterior reduction of the dislocation with pedicle screw instrumentation. The prognosis varies from complete recovery to unchanged neurological involvement depending on the initial injury pattern presentation, as this comprehensive review revealed. Only one case has been reported that resulted to death due to extensive fat embolism after the operation [26].
In conclusion, this study reports a rare injury of the lumbosacral junction. Open reduction and internal fixation was mandatory, as post-traumatic ligamentous insufficiency would lead to abnormal motion. Operative treatment managed to restore the stability of the lumbosacral junction and to produce a solid arthrodesis and a good outcome after two years follow-up.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


