All published articles of this journal are available on ScienceDirect.
Revision of Unicondylar to Total Knee Arthroplasty: A Systematic Review
Abstract
Isolated unicompartmental osteoarthritis in the young patient is a difficult problem to treat; they may be too young to consider total knee arthroplasty due to difficulties with inevitable future revision. Unicompartmental knee arthroplasty is one possible solution as it is perceived by some as being a smaller surgical insult than total knee arthroplasty, with easier revision to total knee arthroplasty than a revision total knee arthroplasty. A total knee arthroplasty performed as a revision unicondylar knee arthroplasty is thought by some authors to have equivalent functional outcomes to a primary total knee replacement.
However, there have been several studies suggesting that revision is not as simple as suggested, and that function is not as good as primary total knee arthroplasty.
We performed a systematic review of the literature regarding outcomes after revision of a unicondylar knee arthroplasty.
Although there are many studies proposing selective use of the unicondylar knee arthroplasty, there are a number of studies highlighting difficulties with revision and poorer outcomes, and, therefore, the unicondylar knee arthroplasty cannot be considered a small procedure that will 'buy time' for the patient, and have results equal to a primary knee arthroplasty when revised. Further controlled studies, ideally randomised, are required before final conclusions can be drawn.
INTRODUCTION
The origins of unicondylar knee replacement date back to the 1950s with the work of McKeever [1]. There has been increasing interest since the 1970s, with large numbers of such implants in use today. However, there has always been an air of controversy around this subject, and there still remains no clear consensus on whether a unicondylar knee replacement is a valid operation to perform for a sub-group of patients with knee arthrosis.
Several advantages of unicondylar knee replacements (UKRs) have been cited. By resecting only the degenerate part of the joint, the rest of the joint is spared, often needing a smaller surgical incision. The Anterior Cruciate Ligament is retained, leading to natural kinematics. Total hospital stay is shorter [2], with less post-operative pain and less intra-operative blood loss [3] than total knee replacements (TKRs).
Patients have a quicker return to function following UKR, with better range of motion [4] and patients with a UKR on one side and a TKR on the other report a preference for the knee with a UKR [4, 5].
However, these potential advantages are to be balanced with the counter-arguments that performing a UKR is not necessarily a smaller procedure [6], with results in published series varying considerably. Revision of a UKR to a TKR is reported by some surgeons as being a relatively straight-forward procedure, while others report poorer outcomes and significant surgical difficulties.
If revision of UKR to TKR gives poorer results than a primary TKR then the decision to perform only unicondylar replacement as a primary procedure may be questioned. Our aim in this paper is to report on the published data regarding revision of UKR to TKR. Due to the wide variation in outcome measures following revision UKR it was not possible to perform a meta-analysis, and this data is instead presented as a systematic review.
METHODOLOGY
We performed a literature search to identify articles reporting on the revision of unicondylar to total knee replacement.
We performed a search using Pubmed and Ovid-Medline and Embase using a combination of the search terms “Unicompartmental”, “Revision Knee”, “Unicondylar”, “Knee Arthroplasty”, and “Total Knee Arthroplasty”. A simplified flow-chart depicting this process is seen in Fig. (1).
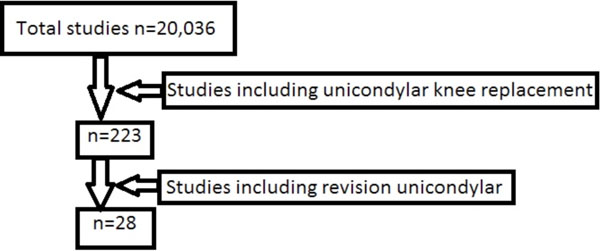
Diagram depicting how relevant studies were identified.
The aim of this paper is not to report on the overall outcome of unicondylar replacement, so studies that did not involve revision of the UKR were excluded. Papers were limited to those published in English.
A total of 223 papers were identified that included the above search terms. After excluding those not in English, those that were review articles and letters/comments we identified 28 papers that were relevant. Details of these studies are in Table 1.
Relevant Published Studies
| Author | Year | Journal | No of knees (Patients) | Age at Surgery | Ave Time at Follow Up |
|---|---|---|---|---|---|
| Chou [8] | 2011 | The Knee | 33 (32) | 60 | 3 years |
| Miller [9] | 2002 | Orthopaedics | 35 (31) UKR/ 100 TKR | 71 | 6 months |
| Oduwole [14] | 2010 | Ir J Med Sci | 14 | 61.9 | 15 months |
| Chakrabarty [15] | 1998 | J Arthroplasty | 73 | 56 months | |
| Knight [16] | 1997 | J Arthroplasty | 12 | 69 | 27 months |
| Aleto [17] | 2008 | J Arthroplasty | 32(29) | 66 | 26 months |
| Saragaglia [18] | 2009 | Int Orthop | 33 | 71.76 | 73 months |
| Springer [19] | 2006 | CORR | 22(18) | 71 | 64.5 months |
| Lai [20] | 1993 | CORR | 48(45) | 64 | 5.4 years |
| Jarvenpaa [10] | 2010 | Int Orthop | 21 UKR/ 28 TKR | 75 | 10.5 years |
| Johnson [21] | 2007 | The Knee | 77 | 66.1 | 6.9 years |
| Otte [22] | 1997 | J Arthroplasty | 29(28) | 69 at follow up | 38 months |
| Wynn Jones [23] | 2011 | The Knee | 89(87) | 68 | 28 months |
| Saldanha [24] | 2007 | The Knee | 36 | 71 | 2 years |
| McAuley [25] | 2001 | CORR | 32(30) | 59 | 53 months |
| Levine [26] | 1996 | J Arthroplasty | 31(29) | 72 | 45 months |
| Barrett [13] | 1987 | JBJS | 29 | 62.5 | 4.6 years |
| Pearse [11] | 2010 | JBJS Br | 31 UKR/ 205 TKR | 64.2 U2U, 66.4 U2K, 68.4 TKR* | |
| Dudley [27] | 2008 | CORR | 68 UKR /112 TKR | 53% UKR/ 63%TKR <65yrs** | |
| Hang [28] | 2010 | Acta Ortho | 1948 UKR/ 896 Rev TKR | 65 UKR/ 67 TKR | |
| Martin [29] | 1995 | The Knee | 18 | 71 | |
| Willis-Owen [12] | 2009 | The Knee | 80 | ||
| Berend [36] | 2009 | Orthopaedics | 50 | ||
| Mercier [30] | 2009 | Int Orthop | 13(11) | 68.8 | |
| Bohm [31] | 2000 | J Arthroplasty | 35(34) | 71 | |
| Lewold [32] | 1998 | Acta Ortho | 1135 | ||
| Padgett [6] | 1991 | JBJS | 21(19) | 52-80 | 2-10 years |
* U2U = Unicondylar knee revised to another Unicondylar knee; U2K = Unicondylar knee revised to total knee replacement; TKR = primary total knee replacement.
** Only range of ages quoted in the study: 53% of revision unicondylar knees and 63% of primary total knee replacements were under 65 years of age, the remainder were over 65.
Data from these studies were analysed. There was a wide variation in methods of reporting outcome, including functional/ pain scores, re-revision rate, survival of prosthesis, difficulty of converting UKR to TKR, bone loss and type of revision prosthesis. As a result, there is no way of accurately combining data from these studies in order to produce a cumulative result from revision UKR.
RESULTS
Only 9 studies performed outcome scores on patients both before and after revision of UKR. Further 8 studies provided outcome scores taken only following revision UKR.
There was variation in the way in which surgery was deemed to be successful or unsatisfactory. This included time to revision of UKR, time to re-revision of a unicondylar that had been revised to a total knee replacement, survival of the revised UKR, survival of a UKR revised to a further UKR, pain relief, bone defects, range of movement, requirements for metal augments/stemmed implants, as well as the different outcome scores mentioned above.
The design of implants also differed significantly. Older papers studied implants such as the PCA (Porous Coated Anatomic), Brigham, St Georg, and Marmor. Newer studies tend to study the Oxford, Brigham, Search Uni and Miller-Galante implants. Implant design has changed considerably over the years and, therefore, earlier studies cannot be directly compared with more recent studies, despite having similar methodology.
Outcome scores were mostly Oxford (three studies), Hospital for Special Surgery (HSS - seven studies), Knee Society Score (KSS - ten studies). One paper used the Total Knee Questionnaire, one study SF-12, one SF-36, two used WOMAC, and two used the Bristol score. A summary of the findings is shown in Tables 2 and 3.
Comparison of Series with Control Subjects
* P = Pain, S = Stiffness, Fn = Function.
Functional Scores in Non-Controlled Studies
| Author | Time at Follow Up (Months) | Score Used | Pre-Revision to TKR | Post-Revision to TKR | Change | Pre-Primary TKR | Post-Primary TKR |
|---|---|---|---|---|---|---|---|
| Oduwole | 15 | WOMAC SF-36 | 40 (W) 57.86 SF | 36.22 (W) 60.4 SF | 3.78 (W), 2.34 SF | ||
| Wynn Jones | 28 | Oxford, SF-12 | 32 (O) 31 SF | ||||
| Pearse | 6 | Oxford | 30.02 | 37.16 | |||
| Chakrabarty | 56 | Bristol | 51 | 79 | 28 | ||
| Johnson | 82.8 | Bristol | 78.2 | ||||
| Barrett | 55.2 | HSS | 45%exc, 21%good, 27%fair, 7% poor | ||||
| Otte | 38 | HSS | 77 | ||||
| Knight | 27 | HSS | 56 | 86 | 30 | ||
| McAuley | 53 | Knee Society* or HSS | 89(81)/76 (HSS) one pt** | ||||
| Lai | 64.8 | Knee Society and HSS | 41(47), 57 (HSS) | 80(74), 82 (HSS) | 39(27), 25 (HSS) | ||
| Aleto | 26 | Knee Society | 48.9 (50.9) | 87.9 (72) | 39 (21.1) | ||
| Saragaglia | 73 | Knee Society | 57(43) | 86(80) | 29(37) | ||
| Springer | 64.5 | Knee Society | 75(66) | 93(78) | 18(12) | ||
| Saldanha | 24 | Knee Society | 86.3(78.5) | ||||
| Levine | 45 | Knee Society | 91(81) |
* Knee Society scores are given as separate components: Pain(Function).
** The scoring system was changed during the study from Knee Society to HSS (Hospital for Special Surgery).
Differences in prosthesis design include metal-backed or polyethylene load transmission to the tibia, cemented or uncemented interface, variable amounts of bone needing to be resected, implants with small pegs or large spikes for fixation, and manufacturing processes that led to poorer quality implants. An example is the PCA (Porous Coated Anatomic) knee, which was found to have a disproportionately high revision rate in the Swedish Registry [7]. Following investigation it was found that the femoral component loosened more than expected, and the polyethylene had poor wear resistance due to its manufacturing process (heat-pressed). It is used less frequently now.
CONTROLLED TRIALS
Only three studies [8-10] compared revision of unicompartmental knee replacements directly with primary total knee replacements performed in the same institution. Of these, one did not record pre-operative knee scores [10] and, therefore, the two groups cannot be compared accurately. Details, including scores, are shown in Table 2.
Chou et al. [8] report a series of 33 knees in 32 patients with an average follow up of 3years who had revision of unicondylar to total knee replacement. Most were Oxford (58%) with the rest being Balansys, Brigham, and EIUS implants. They found a 5year survival of the UKR was 69%, and 90% of UKRs revised to TKR were performed within 5 years of index procedure. They report Oxford scores at 1 year after surgery for the revision UKRs and also a comparable group of patients receiving a primary total knee replacement but did not give further details as to how matched the control group was, if at all. They suggest that revision of UKR to TKR is technically challenging and has inferior results to a primary TKR.
Miller et al. [9] reported 35 knees in 31 patients at 6 months review, who had revision of UKR and compared it to a consecutive series of 100 primary TKRs, but the two groups were not specifically matched. Their study was difficult to interpret because their UKR group was heterogeneous in the underlying diagnosis: most had osteoarthritis, but 2 had rheumatoid arthritis, gout/pyrophosphate deposition in 3, and 4 had avascular necrosis. 74% had a Brigham, with the remainder having the AML cruciate-sparing knee. They used the Knee Society scoring system and found that Posterior Cruciate Ligament (PCL) sparing knee replacements, when used as a revision prosthesis for failed UKR had similar scores to the primary TKR group, but poorer than either prostheses with a flat or constrained revision tibial tray when PCL was sacrificed, and, therefore, primary TKR is comparable to revision UKR, despite noting a high degree of bone loss at time of surgery and requiring a large number of constrained implants or augments.
Jarvenpaa et al. [10] report the results, at an average 10.5 years, of 21 patients with unicompartmental knee replacements revised to TKR, and matched these to a control group of 28 primary TKR. Using the WOMAC score they found more revision-UKR patients were dissatisfied with their surgery than those having primary TKR with regards to stiffness, pain, and physical dysfunction. However, pre-operative scores were not available and, therefore, the patients undergoing revision of TKR may have had worse pre-operative scores leading to poorer scores following surgery, and may not be a truly comparable group. Hospital stay was comparable for both groups: 8.3 days for revision UKR and 7.9 days for primary TKR. Overall, they found primary TKR to have superior results to revision of a UKR.
CASE SERIES
The majority of studies are not controlled trials and report the outcome of a cohort of patients. Although the results of their surgery from UKR to TKR are detailed, and some papers quote outcomes for their series of primary total knee replacements as a comparison, details such as patient demographics for the primary TKR group are not given, and, therefore, we cannot interpret these in the same way as the small number of controlled/ matched series studies.
Table 3 shows the published functional scores for these studies. There is variation in the type of scores used, and these are discussed later.
There is useful data available from various local [27] and national [2, 7, 11, 28] joint replacement registries. Although these are retrospective analyses of data, limited by the type and quality of data held by the registry, they are on a very large scale and are able to report on much larger numbers of revision UKRs. However, the useful information from these studies is largely limited to the incidence of revisions and re-revisions, broad modes of failure, and the number of revisions requiring augmented prostheses.
Hang [28] have reported a data set from the Australian Joint Registry comparing patients who had revision of UKR to TKR, to patients having revision TKR, which showed the further revision rate for both groups was similar at 5 years, 15% and 18% respectively.
FUNCTIONAL SCORES
Functional scores are reported using different scoring methods, and so are not directly comparable. Tables 2 and 3 show the functional scores for controlled and non-controlled studies, respectively. Only 9 studies measured pre- and post-operative scores, 9 others measuring only the score at follow-up.
Pearse et al. [11] reviewed data from the New Zealand registry including revision rates and functional scores. They found that, at 6 months, the Oxford score for primary TKR was better than for unicondylar knee replacement, and scores for TKR revised from UKR were equivalent to those for revision TKRs. Their findings suggest that unicondylar knee replacement is not superior to a primary knee replacement, neither from a functional point of view nor from revision surgery outcome.
Willis-Owen et al. [12] used the Total Knee Score Martin et al. reported on 18 patients and found that following revision of UKR to TKR there were 10 excellent, 3 good, 2 fair, and 3 poor (56% excellent, 17% good, 11% fair, 17% poor) results using the Knee Society score, although they did not quote specific scores.
Similarly, Barrett et al. [13] used the HSS (Hospital for Special Surgery) score at an average of 4.6 years follow-up in their series of 29 revisions of UKR and found 45% were excellent, 21% good, 27% fair, and 7% poor results. Again, they did not quote specific scores.
Chou et al. [8] found a similar improvement in score in the revision UKR group and the TKR group. Miller [9] found the Knee Society score to be lower in patients prior to total knee arthroplasty compared to those about to have unicondylar arthroplasty; but post-operative scores in both groups were similar, suggesting TKR potentially gives more improvement in pain and function than knees affected more mildly and having UKR.
Range of movement is quoted in a small number of studies, shown in Table 4. Although it would be expected that range of movement would improve following revision of a failed joint, two studies actually reported a small decrease in the range of movement [2, 19] and changes in the total arc of movement for all studies was small.
Arc of Movement in Degrees Following Revision of Unicondylar to Total Knee Replacement
| Author | Pre-Revision | Post-Revision | Improvement |
|---|---|---|---|
| Oduwole | 17 | ||
| Knight | 108 | 113 | 5 |
| Aleto | 108.2 | 110.1 | 1.9 |
| Springer | 113 | 111 | (-)2 |
| Lai | 110 | 101 | (-)9 |
| Jarvenpaa | 105.7 | 106.8 | 1.1 |
| Otte | 110 | ||
| McAuley | 111 | ||
| Levine | 115 | ||
| Barrett | 110 |
MODES OF FAILURE
Although to review the mechanism of failure of unicompartmental knee replacements in the published literature is beyond the scope of this paper, we report the main reasons for failure of the UKRs that were revised in this study. A summary of the published data from these studies is in Table 5.
Cause of Failure of Unicondylar Knee Replacements Revised to Total Knee Replacements
| Study | OA | Loose | Prosth # | Peri-Prosth # | Insert Disloc | Poly | Implant Subsided | Alignment or Instability | Pain | Infect |
|---|---|---|---|---|---|---|---|---|---|---|
| Chou | 4% | 50% | 18% | 7% | 21% | |||||
| Miller | 37% | 26% | 5% | 8% | 24% | |||||
| Oduwole | 15% | 29% | 7% | 21% | 15% | 15% | ||||
| Chakrabarty | 37% | 22% | 11% | 1% | 22% | |||||
| Knight | 42% | 50% | ||||||||
| Aleto | 19% | 19% | 13% | 3% | 47% | |||||
| Saragaglia | 12% | 64% | 18% | 3% | ||||||
| Springer | 13% | 32% | 55%* | |||||||
| Lai | 21% | 65% | 4% | 2% | 8% | |||||
| Jarvenpaa | 5% | 19% | 71% | 5% | ||||||
| Otte | 34% | 31% | 3% | 24% | 3% | |||||
| Wynn Jones | 11% | 55% | 9% | 16% | 11% | 6% | ||||
| Saldanha | 36% | 39% | ||||||||
| McAuley | 28% | 66% | ||||||||
| Levine | 32% | 68% | ||||||||
| Barrett | 38% | 55% | 6% | |||||||
| Pearse | 6 /8% | 45 /37% | 29 /4% | 29 /49% | 6 /5% | |||||
| Dudley | 48% | 24% | 21% | 2 | ||||||
| Hang | 18% | 50% | 12% | 5 | ||||||
| Martin | 70% | 17% | 13 | |||||||
| Berend | 20% | 44% | 10% | 16% | 10% | |||||
| Mercier | 23% | 38% | 31% | |||||||
| Bohm | 11% | 49% | ||||||||
| Lewold | 26% | 43% | 5% | 4% | ||||||
| Padgett | 33% | 14% | 33% | 5% |
OA = Osteo-arthritic progression into other compartments; Loose = Aseptic loosening; Prosth = Prosthesis; Insert Disloc = Bearing insert dislocation; Poly = Significant wear of polyethylene bearing; Pain = Pain of unidentified origin; Infect = Infection
* All the knees with failure due to polyethylene wear were Brigham knees in this series by Springer et al. [19].
Older prostheses differ to modern prostheses in the way they failed, and designs are different enough to make direct comparison impossible. We have already discussed the PCA knee with its unusually high rates of polyethylene bearing surface wear and large femoral bone defects leading to loosening. The Brigham knee was found to have a significant amount of polyethylene wear [7] making it the cause for 55% of the revisions in one series. The failure rate for resurfacing and non-modular implants was found to be higher in Berend's series of 50 cases [36].
Bone defects are found in all revision procedures to some extent, but not all are significant. Table 6 shows the occurrence of significant bony defects and the techniques used to overcome the defects.
Bone Defects Found at Time of Revision UKR to TKR
| Author | Bone Defects | Augments | Autologous Bone Graft | Structural Bone Graft | Stemmed Implants | Metal Wedges |
|---|---|---|---|---|---|---|
| Chou | 67% | 18% | 36% | 33% | ||
| Miller | 24% | 17% | 6% | 3% | ||
| Oduwole | 43% | |||||
| Chakrabarty | 58% | 22% | 11% | 11% | 10% | |
| Knight | 58% | |||||
| Aleto | 78 | 75% | 47% | 25% | ||
| Saragaglia | 66% | 24% | 55% | 36% | ||
| Springer | 68% | 68% | 9% | 23% | ||
| Lai | 50% | Only cement | ||||
| Jarvenpaa | 29% | 19% | 5% | |||
| Otte | 69% | 69% | 14% | |||
| Wynn Jones | 30% | 34% | 17% | |||
| Saldanha | 33.30% | 17% | 6% | 17% | 6% | |
| McAuley | 31% | 44% | 25% | |||
| Levine | 23% | 9% | 19% | |||
| Barrett | 17% screw +cement | 10% | 34% | 3% | ||
| Pearse | 28.30% | 22% | 14.10% | |||
| Dudley | 43% Rev-UKR | 26% Rev-UKR 70% Rev-TKR | 24% Rev-UKR 50% Rev TKR | |||
| Martin | 39% | 13% | 28% | 0 | 11% | |
| Berend | 23% | |||||
| Bohm | 34% | |||||
| Padgett | 76% | 5% | 14% | 5% |
Most studies show at least half of knees had a significant bony defect, often requiring the new implant to have metal wedges or stems, as well as frequent use of bone graft. One advantage of revising UKR to TKR is that there is still bone in the previously unaffected compartment that can be used as autologous graft. Dudley compared revision UKR to revision TKR and found the requirement for metal wedges to be almost twice as likely in revision TKR, and stems almost three times as likely.
Some studies have used mainly cement to fill defects, whereas most tend to use either stemmed implants or wedges to build up defects. Barrett et al. [13] suggest having stemmed implants available for all revision UKRs.
In a series of 89 knees Wynn Jones et al. [23] found a poorer SF-12 score if revision components were used due to excessive bone loss, compared to knees where standard TKR implants were used. A similar outcome was found by Saragaglia et al. [18], however their two groups were not entirely comparable.
Modern knee arthroplasty systems have more modularity and have the flexibility to use augments. Older studies have used cement to fill all bone defects [20], whereas current thinking is to use metal wedges/ stems in preference to filling defects with cement [17, 18, 25].
DISCUSSION
The measures used to report success or failure in the studies we analysed were very different. There is no general consensus on whether it is better to perform a UKR in a select group of patients with isolated unicompartmental degeneration and then revise to a TKR, or whether to proceed directly to TKR and replace compartments that are not degenerate in the belief that there is greater longevity of the TKR compared to a UKR.
Proponents of the UKR feel they can 'buy time' for the patient by performing a seemingly smaller operation, which is easier to revise than a TKR. Proponents of primary TKR would argue that revision of UKR to TKR is more difficult than a primary TKR and with poorer results in some studies.
The time to failure of a UKR has been debated in the literature for some time. The UK National Joint Registry [2] reported on 238,731 revision TKRs, of which 16,393 were revisions of UKR. The revision rate at 5 yrs was 9.4% for UKR and 3% for cemented TKR.
The rate of satisfaction following knee arthroplasty has been investigated by Baker et al. [33], who analysed the results of 7,230 returned questionnaires and Oxford scores from a postal survey sent to 10,000 patients on the UK National joint Registry. 9% of respondents had UKR and 92% TKR. They found that pain was a more reliable indicator of overall satisfaction than function, and UKR patients were less satisfied than those with a primary TKR.
Registry data needs to be interpreted with some caution, as the end point to determine failure is often revision. However, revision may be deemed more difficult if there is a TKR in situ than a UKR, so revision surgery may be offered by the surgeon more readily to patients with a failing UKR.
The New Zealand registry holds data including Oxford scores, and shows that UKR patients tend to have higher scores at the time of revision than TKR patients, suggesting that their knees are functioning better, and have been revised earlier than if they already had a TKR [34].
While UKR undoubtedly has some benefits, a failed UKR should not be revised to another UKR. When analysing results from the New Zealand joint registry Pearse et al. [11] found that UKR that were revised to another UKR had a 6.67 per 100 component-year revision rate, compared to a primary TKR (0.484), and even a revision UKR (1.97).
Hang et al. [28] report results from 1,947 revision UKRs from the Australian registry that were revised to either further UKR or to TKR, and found the revision rate in the UKR to UKR group to be 30% at 3 years, compared to 15% at 5 years for the UKR to TKR group. This is supported by the work of Lai et al. [20] in their series of 48 knees.
Dudley et al. [27] compared revision of UKR to TKR to revision TKR and found that, although the period of hospitalisation was not much shorter, the implant cost and overall cost of surgery was significantly higher in the revision TKR group, suggesting that revision of UKR offers a considerable cost saving over revising a primary TKR.
Willis-Owen et al. [12] calculated several parameters relating to the cost of surgery and found unicondylar knee replacements to be £1761 cheaper than a primary total knee replacement. Hospital stay for UKR averaged 4.2 days vs 6.8 days for TKR according to one registry [2].
Surgical difficulty in revision of a UKR varies in the literature. Some studies [13,15] suggest that revision of a UKR to TKR has few technical difficulties, whereas others report significant surgical difficulties including the use of a large number of augments or stems, as well as autologous or autogenous bone grafts for large bone defects [6, 17, 22].
Rolston et al. [35] present a case report of a patient with a well fixed lateral compartment UKR who developed degeneration in the rest of the knee and had a medial and patello-femoral resurfacing implant (Journey Deuce) inserted while leaving the original UKR in situ and had a good result. However, there are no large series where this strategy has been used, and therefore cannot be routinely recommended where there is progression of OA in previously unaffected compartments.
In young patients it may be difficult to suggest total knee arthroplasty where only one compartment is involved, and few alternatives exist. The UKR is one option, and High Tibial Osteotomy (HTO) is another.
Levine et al. [26] found that revision of UKR to TKR gives equivalent functional scores to primary TKR from their previous series, and that it is preferable to revision TKR or revision High Tibial Osteotomy. Gill et al. [34] report significant intra-operative difficulties when revising HTO, with similar time to revision of HTO or UKR; the HTO group had better Knee Society pain scores (87.3 vs 78.3).
What appears to be clear is that revision of a UKR to another UKR has very poor longevity and should be revised to a TKR. Revision of a TKR is also more difficult than revision of a UKR. Results of revision of UKR appear to be slightly poorer than a primary TKR, but better than revision TKR.
No randomised controlled trials exist, and there are very few comparative studies where outcome measures for revision UKR and primary TKR are standardised. There is also significant variation in the way studies report their outcome as either difficulties with revision, functional scores, range of movement, bone defects, etc. Significant surgeon preference makes it difficult to expect large randomised controlled trials comparing the two groups, but further controlled studies would go some way towards clarifying whether revision of UKR is equivalent to primary TKR, in which case it may be worth giving the patient a few more years of function and pain relief before a primary TKR is performed.
In conclusion, it is likely that UKR gives patients improved function and pain relief, but its advantages over TKR are unclear. UKR is likely to need revision sooner, and, once revised, function of the revised UKR is probably not as good as having a primary total knee arthroplasty, with a high likelihood of requiring an augmented prosthesis; however, a revision UKR will be better than having a revision TKR. Due to the variation in the literature of revision rates for UKR it is unclear if it will be of benefit by prolonging the need for TKR for any significant length of time.
ACKNOWLEDGEMENTS
Mr Z. Ahmad gratefully acknowledges the support of the Technology Strategy Board and of the National Institute for Health Research.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.


