All published articles of this journal are available on ScienceDirect.
Keeping the Swing on Par: Golfers and Upper Extremity Injuries they Face
Abstract
Golf is a sport enjoyed by a rapidly growing population. While it is perceived as a low-demand activity, golf and its thousands of high-energy rotational swings can result in a plethora of upper extremity injuries. We examine the biomechanics of the golf swing and carry out a review, divided by anatomical region of the upper extremity (shoulder, elbow, forearm, wrist, and hand), of common injuries associated with golf. Part I of this review details the shoulder and elbow pathology seen in golfers, while Part II covers the forearm, wrist, and hand injuries associated with the sport. PubMed was searched for articles using terms that corresponded to the specific injury and golf. Additional data was obtained via outside journal searches that did not appear in PubMed. This is a clinical review. Specific phases of the golf swing place golfers at risk for unique injuries that may affect either the leading (left side in a right-handed golfer) or trailing (right side in a left-handed golfer) extremity. Amateur and professional golfers are at higher risk for different injuries, as pros are more likely to suffer overuse injuries, while amateurs may have injuries secondary to improper grip or swing form. We identify and comment on six shoulders, two elbow, eight forearm and wrist, and three hand injuries associated with golf. Current trends in management, as well as golf-specific rehabilitation and return to sport timelines, are discussed for each injury. Growing participation and an aging population make golf a common source of upper extremity injury. We delineate 19 of the most common upper extremity injuries that golfers face and equip providers with up-to-date information to appropriately diagnose, manage, and rehabilitate these injuries.
1. PART I: SHOULDER AND ELBOW
1.1. Introduction
With its roots in Scotland, golf has become a game played amongst those of all ages and backgrounds. In the United States, twenty-five million Americans play over five hundred million rounds of golf per year [1]. These numbers have surged since the induction of golf in the 2016 Rio de Janeiro Olympic Games [2]. As such, golf has become a popular recreational and tourist activity while inspiring many to play the game at a high level [3].
To most, golf is perceived as a deceivingly low-demand activity. However, the average swing speed is 80 miles per hour, while the average ball speed is 60 miles per hour [4]. One can imagine doing this over 100 times per round can be physically taxing on the golfer’s body. In addition, those who walk the course also have to bear the load of carrying their 40 pound bag while walking approximately 3.75 miles during an 18-hole round. Interestingly, golfers who are unable to achieve 8 metabolic equivalents (METs) safely are advised to use a golf cart and cautiously monitor their ability to complete the round [5]. Given the strenuous circumstances mentioned above, golfers of all ages and skill levels are predisposed to some form of injury. Potential etiologies can be bony, ligamentous, tendinous, or vascular in nature.
In this two-part review article, we delineate various types of upper extremity injuries encountered by amateur and professional-level golfers. We also differentiate between injuries that occur in the leading extremity (left extremity for a right-handed golfer) versus the trailing extremity (right extremity for a right-handed golfer). We highlight the most recent trends in treatment for these injuries and methods for preventing re-injury. We hope that with our findings, medical providers can employ the broad differential needed to facilitate informed decisions on behalf of their golfing patients.
Part I of the review focuses on shoulder and elbow pathology seen in golfers. Golf-related ailments of the shoulder covered include acromioclavicular (AC) joint arthritis, glenohumeral instability, glenohumeral arthritis, rotator cuff injury, superior labral anterior to posterior (SLAP) lesions, and adhesive capsulitis. Lateral and medial epicondylitis of the elbow are also discussed in this part of the review. Part 2 of the review covers hand and wrist pathology.
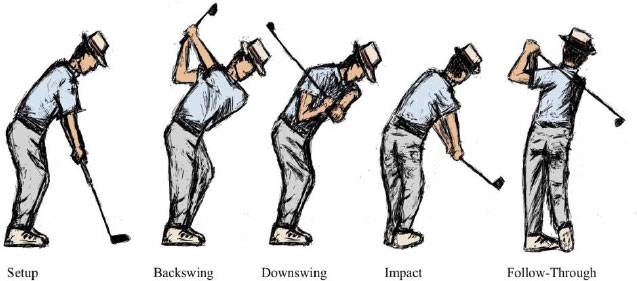
1.1.1. The Golf Swing
It is important to examine the role of the upper extremity during each phase of the golf swing to better understand the predisposing factors to injury. The five phases of the golf swing include setup, backswing, downswing, impact, and follow-through (Fig. 1). The most important part of the setup is the grip, where grip size is an important factor to consider. Grips that are too small can predispose the golfer to tendinopathy; however, grips that are too big may compromise clubhead speed [6]. The backswing is characterized by moving the club away from the ball with the wrists in radial deviation [7]. The backswing also places the trailing upper extremity in extremes of abduction and external rotation of the shoulder. Improper backswing mechanics can lead to injury in the glenohumeral and acromioclavicular joints. During the downswing, both wrists move from radial to ulnar deviation. In addition, the leading upper extremity moves from the extension of the left elbow to the extension of both elbows. As a result, golfers may experience injury to their lead shoulder and elbow [8]. At impact, the golfer’s club makes contact with the ball. A golf swing taken with the club hitting the ground before the ball may lead to fracture or tendinopathy to various upper extremity anatomical areas [9, 10]. During the follow-through, both wrists are in radial deviation. In addition, this phase involves marked abduction and external rotation of the leading shoulder, producing increased anterior force along the shoulder capsule. Golfers may experience lead shoulder pain during this phase [11].
Golfers apply power-generating maneuvers during these phases, predisposing them to various forms of injury. In amateur players, the injury typically results from a “strong” grip (gripping the club too tightly), poor swing biomechanics, improperly fit equipment, and overuse. Seasoned golfers typically experience injuries related to long hours spent at the course perfecting their craft, thus resulting in a myriad of overuse injuries. Understanding the phases of the golf swing can help better predict where injury will occur (i.e., leading versus trailing extremity) and under which circumstances.
1.2. Shoulder
Shoulder injuries account for 12% of golfing injuries in both amateurs and professionals [12, 13]. Shoulder injury rates increase in golfers who play 4 or more rounds and hit over 200 balls per week [12]. Younger golfers are more susceptible to overuse and instability injuries, while golfers over the age of 35 are more likely to experience injury due to arthritic and degenerative changes [14]. Careful diagnosis, management, and rehabilitation are required in order to produce the most successful outcome in the golfer who has sustained a shoulder injury.
1.2.1. AC Joint Impingement and Arthritis
The acromioclavicular (AC) joint is a plane synovial joint connecting the distal end of the clavicle and the medial aspect of the acromion. The AC joint consists of a weak capsule relying on ligamentous stability that is strengthened by the acromioclavicular, conoid, and trapezoid ligaments. Injury to the AC joint is known to be the culprit of many golf-related lead AC joints as the source of injury in 53% of cases of lead shoulder pain [15]. Golf-related AC joint pain is due to either impingement or arthritis.
Golfers with AC joint injuries present with anterior shoulder pain localized to the AC joint at the top of the backswing [14, 16]. This motion places increased stress on the lead shoulder by compressing the AC joint and stressing the posterior capsule [17]. On physical examination, hyperadduction of the shoulder during the backswing elicits similar pain as found in the cross-body test [18].
For patients with signs of impingement, a course of rehabilitation (physical therapy or occupational therapy) is recommended to improve strength and alleviate symptoms. Length of rehabilitation can range between patients; though after 3-6 months of failed conservative treatment, operative measures may be considered [19]. This syndrome is typically associated with AC joint bursitis; thus, bursectomy is the first offered operative treatment [20]. Bursectomy could lead to significant improvement in AC joint pain. Refractory cases can be treated with distal clavicular resection or beveling of the AC joint [20]. Both non-operative and operative interventions are effective in alleviating pain [21].
AC joint arthritis can be diagnosed with plain film imaging [17, 18]. If the cause is determined to be osteoarthritic, first-line non-operative treatment should be pursued. Rest with activity modification can be used to decrease the load placed in the backswing. AC joint corticosterone injections have also been shown to decrease pain in cases of osteoarthritis [22]. Rehabilitation in the context of AC osteoarthritis without impingement is not recommended [18, 22].
If AC joint arthritis non-operative management fails, surgical intervention can be pursued via distal clavicle excision. This procedure resects the distal end of the clavicle to decompress the AC joint and alleviate pain. Rehabilitation consists of early passive and active range of motion 2 days post-surgery, with gradual strengthening and return to sport as tolerated [23]. Both open and arthroscopic distal clavicle excision have been shown to produce effective long-term outcomes, while arthroscopy can facilitate a more rapid return to play, 100% versus 75% return to sport at 1 year post-operative from arthroscopic versus open distal clavicle excision, respectively [18].
1.2.2. Glenohumeral Instability
The glenohumeral (GH) joint is a ball-and-socket joint formed by the articulation of the humeral head and the glenoid fossa of the scapula. The joint has multiple stabilizing ligaments, including the capsular, glenohumeral, and transverse humeral ligaments. The GH joint is predisposed to instability due to a weak overlying shoulder capsule. The backswing, downswing, and follow-through phases of a golf swing place increased stress on the golfer’s lead shoulder. Overuse may eventually lead to instability of the GH joint. This condition usually arises in younger golfers with predisposing joint laxity (i.e., found in Marfan syndrome or Ehlers-Danlos Syndrome) [14, 24, 25].
Golfers may present with either posterior or anterior instability. Posterior instability causes pain and a sensation of instability at the top of the backswing or during the backswing-to-downswing transition when the posterior capsule of the lead shoulder is most stressed. A “pop” or “clunk” sound may also be appreciated with subluxation of the humeral head [25, 26]. On physical exam, patients may have a normal active and passive range of motion. However, signs of instability can be appreciated during a load-and-shift and posterior apprehension test [26, 27]. Imaging work-up should include anterior-posterior (AP) and axillary view radiography with intra-articular contrast magnetic resonance imaging (MRI) in chronic conditions [27].
Anterior instability presents with apprehension in the lead shoulder during the follow-through. Positions inducing anterior pressure will be uncomfortable for the patient; thus, the apprehension-relocation and load-and-shift tests can be diagnostic during physical examination. Imaging consists of initial AP and axillary radiographs. MRI may be used to view soft tissue injury and assess for Hill-Sachs lesions, while CT can allow for evaluation of Bankart lesions and glenoid geometry [28, 29].
First-line management consists of a 12-week course of rehabilitation (physical/occupational therapy) to strengthen the surrounding rotator cuff musculature [30]. If patients are still symptomatic after 3-6 months of conservative therapy, arthroscopic repair of underlying injury may be indicated [27]. Operative measures include capsulolabral repair, capsular plication, and re-tensioning of the inferior glenohumeral ligament [27]. Electrothermal capsulorrhaphy may performed, though isolated capsulorrhaphy may not be adequate for overhead athletes to return to play [26, 31]. With successful surgical intervention, golfers can begin a rehabilitation program consisting of an initial range of motion and strengthening of scapular stabilizing muscles, resumption of chipping and putting at 3 months, and return to full play within 4-5 months post-surgery [26].
1.2.3. Glenohumeral Arthritis
A lifetime of golf swings can cause wear and tear of the glenohumeral (GH) articular cartilage. GH arthritis can affect either the lead or trailing shoulder and has been seen in older golfers [15, 16, 24]. Patients with GH arthritis will frequently note a history of deep pain in the shoulder that may cause trouble falling and staying asleep [32]. Limited active and passive range of motion, along with compensatory scapular dyskinesia, are physical exam findings that point towards GH arthritis [24]. Diagnostic imaging consists of orthogonal view radiography, allowing for a tangential view of the GH joint. Axillary and AP views may also be obtained to search for secondary arthritic findings, including cartilage thickening, humeral deformity, glenoid erosion, and humeral subluxation (Fig. 2) [32]. Negative radiographic findings can suggest a diagnosis of adhesive capsulitis.

In addition to initial anti-inflammatory medication and activity modification, rehabilitation protocols are effective in balancing the scapula in cases of mild to moderate arthritis [24, 32]. Severe arthritis requiring operative intervention can be treated with hemiarthroplasty, total shoulder arthroplasty, or reverse total shoulder arthroplasty. Indications for each of these surgeries depend on the patient’s age, glenoid involvement, rotator cuff function, and prior surgical history.
Golfers are likely to be worried about return to play and performance after arthroplasty; however, they should be assured that return to golf is highly likely, with rates of return ranging from 88.5% to 95.8% post-surgery [16, 33-35]. Patients can expect to return to golf within 4-6 months post-surgery [17, 24, 33]. Generally, putting can begin within 2-6 weeks, chipping at 4-10 weeks, swinging irons at 1.5-3 months, and full return to play at 4-6 months [16, 33]. Interestingly, golf performance may increase after surgery. Improvements in both driving distance and overall skill level have been noted in two reviews evaluating performance post-arthroplasty, potentially due to pain improvement and post-operative strengthening [33, 34]. These improvements were most dramatic in those undergoing arthroplasty in the trailing shoulder [34]. Of note, golfing does not increase one’s risk for post-operative complications; component loosening and osteolysis in golfers are similar to the general population after surgery [16, 33].
1.2.4. Rotator Cuff Injury
The rotator cuff is a group of four muscles (supraspinatus, infraspinatus, subscapularis, and teres minor) that work in concert to stabilize and allow for motion of the ball-and-socket shoulder joint. Electromyography (EMG) recordings of professional golfers demonstrate that the subscapularis is the most active during the acceleration phases of the swing, while the infraspinatus and supraspinatus stabilize the shoulder at the ends of the swing. The overlying deltoid muscle is relatively silent [11], [36]. The highest risk factor for rotator cuff injury is increased age. As there is increased play with increased age in golfers, it follows that rotator cuff injuries are found to be one of the most common injuries among golfers [11, 37, 38].
Patients with rotator cuff injury may present with complaints of persistent shoulder pain, decreased strength, limited range of motion, and/or signs of impingement. Often, symptoms are so severe that patients are unable to play golf. If they are able to play, pain may be noted during all phases of the swing [37]. Tenderness at points of insertion of the rotator cuff muscles and atrophy of the supraspinatus and infraspinatus may also be present [37-39]. MRI is considered to be the imaging gold standard for a rotator cuff injury and may allow for pre-operative planning if surgery is required [38, 39].
Generally, non-operative management consisting of rehabilitation and anti-inflammatory medications is the first line of treatment [8, 40]. It is important for rehabilitation protocols to focus on progressive strengthening and loading of the rotator cuff muscles [41]. Subacromial corticosteroid injections are often used in the setting of rotator cuff tears and may alleviate pain but have not been shown to improve long-term outcomes [40, 42, 43]. In cases refractory to non-operative management, surgical intervention consisting of open or arthroscopic rotator cuff repair may be indicated. Acromioplasty can also be performed as a concomitant procedure. There is controversy as to whether acromioplasty should be performed as some authors fail to show clinical differences in patients undergoing arthroscopic rotator cuff repair with or without acromioplasty; however, golfers who wish to obtain their pre-injury level of play may benefit from the additional procedure [44]. A series of 30 golfers who underwent rotator cuff repair with acromioplasty revealed all but three returned to their pre-injury competition level, with driving, the initial long-distance tee shot, being the most noted affected aspect of golf post-surgery [37]. Patients underwent a rehab regimen consisting of 3 months of therapy and gradual golf progression with chipping and putting at 3 months and driving at 4-5 months post-operation.
1.2.5. SLAP Lesion with Biceps Tendonitis
The glenoid labrum lines and deepens the glenoid fossa. This allows for greater surface area articulation with the head of the humerus, stabilizing the shoulder joint. The tendon of the long head of the biceps inserts along the superior edge of the glenoid, becoming continuous with the circumferential labrum. Superior labral anterior to posterior (SLAP) lesions have been noted to affect the lead shoulder in both amateur and professional golfers [8, 14, 16]. This lesion, which often afflicts overhead athletes, consists of a tear along the superior aspect of the glenoid labrum, with frequent involvement of the long head of the biceps. Pain is most often felt at the top of the backswing or the beginning of the forward-moving downswing with the lead arm in a cross-body position [8, 16]. Patients may note a “catching” or “clicking” sound at this position with weakness at ball contact and complain of “dead arm syndrome”, an inability to swing the club with the same pre-injury velocity [16, 45].
Physical exam special tests include the relocation test, Yergason’s test, compression-rotation test, and the newer passive-compression test. These tests have shown promise in the detection of SLAP lesions; however, there is no current physical exam gold-standard [45-47]. Therefore, imaging in conjunction with suspicious exam findings is required for diagnosis. MR arthrography has been shown to be superior to MRI and CT in the detection and classification of SLAP lesions [45, 48].
Rest, rehabilitation, anti-inflammatories, and corticosteroid injections are the first-line conservative treatment options for SLAP tears [8, 16]. Lack of improvement after 3 months of rehabilitation may necessitate arthroscopic surgery consisting of debridement, repair, and tenotomy or tenodesis of the biceps [16, 45, 49]. The latter procedure moves the attachment point of the long head of the bicep from the labrum to the humerus to alleviate pressure from the labrum. Though there is no golf-specific outcome data available, SLAP repair surgery has been shown to have good functional outcomes with successful return to play in baseball, rugby, and recreational athletes [45, 50, 51].
1.2.6. Adhesive Capsulitis
Adhesive capsulitis, known colloquially as “frozen shoulder”, is a clinical condition characterized by a restricted range of motion in all directions [52]. The condition occurs due to excessive fibrotic tissue across the GH joint, leading to shoulder stiffness. Patients present with initial pain followed by loss of motion with no history of shoulder trauma [52, 53]. Golfers will likely report a period of painful swings, followed by complete cessation of golf activity secondary to pain and loss of shoulder motion. Adhesive capsulitis commonly affects older patients > 40 years old who have comorbid diabetes mellitus, thyroid disease, or other autoimmune disease [53, 54].
Treatment is dependent on the stage of the condition. Non-operative management can be effective in 90% of cases [54, 55]. Specifically, anti-inflammatory medications and other oral pharmacologic agents can be used to decrease pain associated with the condition [52, 53]. The early, painful stage of adhesive capsulitis can be treated with corticosteroid injections as this is considered an inflammatory state, while later stages should not be treated with local injection [52, 53]. Rehabilitation is considered a hallmark of treatment. Therapists should work in the early stages to prevent capsular contracture and in later stages to aggressively stretch the capsule [52, 53]. Prolonged, low-load bearing stretching has been noted to be preferred to brief high-load movements for both golfers and non-golfers [53].
Surgical management is considered after 6 months of refractory non-operative management [52]. Options include capsular release and manipulation via arthroscopic capsulotomy and synovectomy if synovitis is found to be present [52, 53]. There is no present data on return to play after surgery; golfers should return to the course gradually as they regain range of motion and strength.
1.3. Elbow
The elbow accounts for 25% of all amateur golf injuries and 10% of professional golf injuries [12]. It is also the most common location for golf injuries in women [12, 56]. Female golfers are thought to be predisposed to elbow injury due to increased carrying angle [57]. Elbow injuries may result in long absences from golf, and it takes an average of 74 days to return to the course [12]. Elbow injuries can have traumatic or overuse etiologies. Overuse injuries commonly affect the lateral epicondyle of the lead arm, while traumatic injuries affect the medial epicondyle of the trailing arm. Lead elbow injuries are common in amateurs, while professionals are more likely to suffer trail elbow injuries [17, 24]. These differences can be attributed to variations in swing mechanics and load transfer.
1.3.1. Lateral Epicondylitis
The lateral epicondyle is the origin of extensors of the wrist and fingers, including the extensor carpi radialis brevis (ECRB), extensor digitorum communis (EDC), and extensor digiti minimi (EDM). The extensor carpi radialis longus (ECRL) originates just above the epicondyle on the lateral supracondylar ridge. Lateral epicondylitis is thought to begin as a microtear of the ECRB, EDC, or ECRL, though the ECRB is most often affected [58]. Injury causes gray, fibrillated tendon fibers that may form a sinus tract in the elbow (Figs. 3a and b) [58].
Lateral epicondylitis is the most common upper extremity injury seen in the amateur golfer and usually affects the lead elbow [56, 59]. This injury is associated with overuse of the forearm extensors [12]. Grip and swing forms are known to be risk factors for the development of lateral epicondylitis. Gripping the club too tightly and keeping the lead arm straight may increase the load to the extensors of the wrist and fingers, thus increasing the risk of lateral epicondylitis [17, 59]. This condition has also been seen in a right-handed golfer who changed his grip to a “strong” grip position with his left hand supinated and right forearm in excessive pronation in order to avoid slicing the ball [60].
Patients will complain of insidious onset lateral elbow pain that worsens with activity and may radiate down the forearm [17, 58]. The pain is reproducible with palpation, likely at the ECRB or affected tendon, and may occur with passive flexion or actively resisted extension of the wrist and fingers [17, 58]. Pain may also be noted with forearm supination, and patients may complain of poor grip strength [60]. A physical exam will reveal point tenderness at the lateral epicondyle as well as a positive Thomsen test [61]. If bony tenderness is present, radiographs may be ordered for evaluation; however, these are usually not required [17].
Initial non-operative management consists of anti-inflammatory medications and rest. Wrist orthoses have been shown to provide greater pain relief compared to counterforce forearm braces, i.e., 23% versus 4% reduction in pain at worst scores at 6 weeks [62]. This is likely due to increased immobilization of the extensor muscles. Corticosteroid injections are commonly used, though they may only help with pain relief and not provide increased function or repair [63]. Platelet-rich plasma injections have been shown to reduce pain by 93% in chronic cases that have failed other non-operative treatments [64].
A course of rehabilitation is necessary for patient education to prevent further injury, as well as a systematic approach to resolving pain and increasing motion and upper body strength prior to returning to sport. Golf instruction focusing on proper grip can be useful to reduce tension on the forearm extensors [17, 59]. A progressive return-to-play schedule can be initiated once strengthening exercises can be performed without pain [59, 60].
Surgery is indicated after 6 months of unsuccessful conservative treatment. Multiple surgical options exist, including open excision of pathologic tissue and reattachment of the ECRB, arthroscopic debridement, and denervation in refractory cases [58, 65, 66]. These procedures have been shown to be highly effective, with comparable rates of pain relief, function, and rehabilitation between arthroscopy and open surgery [67, 68]. The complication rate may be slightly higher in open surgeries for all patients [68]. Approximately three months of rehabilitation post-operatively is necessary to restore the motion, strength, and endurance required for returning to golf.
Return to play can vary between players. In non-operative cases, patients have been reported to return to the course within 10 weeks [60]. Players who undergo surgical management can expect to return to chipping and putting in 3-4 months and full play in 4-5 months, with pre-operative levels of play within a year [69].
1.3.2. Medial Epicondylitis
The medial epicondyle is the attachment point of the ulnar collateral ligament and flexor muscles of the forearm, including the flexor carpi radialis, flexor carpi ulnaris, flexor digitorum superficialis, and palmaris longus. The pronator teres originates just superior on the supracondylar ridge. Medial epicondylitis is known as “golfer’s elbow”, though it is less common amongst golfers than lateral epicondylitis [56, 58]. Medial epicondylitis is more likely to be due to a traumatic deceleration that affects the trailing arm [17, 24]. Traumatic deceleration causes sudden trailing arm wrist extension and forearm supination that can cause injury to the flexor carpi radialis and pronator teres muscles [17, 58]. In amateur golfers, this may be due to hitting the ball “fat”, when the club strikes the ground before the ball due to a steep downswing [8, 70]. In professionals, this can be due to an obscured tree root or thick playing fields [70].
Patients will present with pain and tenderness over the affected area, usually distal and lateral to the medial epicondyle [24]. Normal strength and range of motion may be noted, though patients will complain of pain exacerbation with wrist flexion and forearm pronation [24, 58]. A positive Tinel’s sign and elbow flexion test may indicate concomitant ulnar compression, which is present in 20% of cases [58, 69].
Non-operative treatment is similar to that of lateral epicondylitis, including rest, orthoses, anti-inflammatory medication, and rehabilitation. However, corticosteroid injections should proceed with caution as there is potential for injury to the ulnar collateral ligament and ulnar nerve [17, 71]. Surgery may be considered after 6-12 months of unsuccessful non-operative management. Open surgery consists of excision of diseased tissue, neovascularization via medial epicondyle drilling, and re-approximation of the tendon [72, 73]. Ulnar nerve decompression and transfer may be required when subluxation injuries are found [73]. Surgical management is highly effective and allows 95% of athletes to return to previous levels of sports, including golf, after a dedicated 3-month course of rehabilitation [72].
2. PART II: WRIST AND HAND
2.1. Introduction
While generating power in a golf swing largely relies upon the legs and torso, the final links in the body’s kinetic chain are the wrist and hand. The hands and wrists of the golfer are also the first to experience force after the impact of the club with the ball. Wrist and hand injuries are amongst the most frequently injured parts of the body in both amateur and professional golfers. The leading wrist and hand (left side in right-handed golfers) are affected more often than the trailing wrist and hand. An overlapping grip is the most frequently used to grasp the club, with the small finger of the dominant hand locking over the index finger of the nondominant hand. Having a relaxed grip on the club with an appropriate distance between the hands may reduce injury likelihood and improve swing power. Club grips should be regularly replaced to avoid significant wear, as worn-out grips can also lead to over-tensioning of the hands.
Acute and chronic injuries of the wrist and hand can occur from golf play. One possible cause of these acute injuries is the high impact forces during misplaced swings in amateur golfers. In more seasoned players, overuse injuries cause many of the more chronic pathologies seen in the upper extremities. Repetitive swinging and impact of the club can result in tendonitis or nerve compression in these athletes.
In this second part of the review, we focus on common wrist pathology seen in golfers, such as DeQuervain’s disease, intersection syndrome, extensor carpi ulnaris disorders, flexor carpi radialis tendinitis, flexor carpi ulnaris tendinitis, carpal tunnel syndrome, triangular fibrocartilage complex injury, and pisotriquetral arthritis. We also cover hand pathology seen in golfers, including trigger finger, hook of hamate fracture, and hypothenar hammer syndrome.
2.2. Forearm and Wrist
Injuries to the wrist are the most common injury sustained by both amateur and professional golfers [56, 74]. Injury rates for both groups of players have been reported to be around 20-30% [57, 75]. For the recreational player, the etiology of these injuries is thought to be related to overuse, unfavorable swing mechanics, unfavorable equipment quality, and transmitting forces from ground impact [7]. The mechanism of wrist injuries in professional golfers is related to greater time spent in practice and greater impact power [7]. Professional golfers report an increased incidence of injury to the leading wrist [7, 74].
The nature of injuries reported to the wrist arises from various tendinopathies, arthritis, and ligamentous injuries. Injuries can occur either in an acute or chronic fashion. If not identified and treated appropriately, these injuries have the potential to keep the golfer out of play for a prolonged period of time.
2.2.1. De Quervain’s Disease
First described in 1897, De Quervain’s disease involves the thickening of the first dorsal compartment tendon sheath due to inflammation from mechanical irritation [76]. This fibro-osseous tunnel contains the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons. Wrist positioning can influence the relationship of these two tendons: the tendon sheath and radial styloid process.
Increased radial deviation can cause increased friction of the two tendons within the tendon sheath and lead to the development of De Quervain’s disease. For the amateur golfer, this mechanical irritation can originate from over-cocking the wrist during the backswing and failure to maintain this position during the downswing. This is interestingly the same maneuver used to diagnose De Quervain’s disease (Finkelstein Test); the thumb is placed in the palm of the hand with a clenched fist, and the wrist is taken from radial to ulnar deviation.
The highest incidence of De Quervain’s disease occurs in female professional golfers [7]. The etiology of De Quervain’s in the professional player is overuse in nature, thought to be related to repetitive microtrauma to the first dorsal extensor compartment from prolonged periods of practice.
Treatment options range from non-operative to operative. The golfer should consider resting with a custom orthosis until symptoms are improved. Swing modifications can also be considered. A potentially more favorable swing pattern would involve delayed wrist uncocking until impact and a less aggressive transition from radial to ulnar deviation typically seen in amateur golfers [10]. Anti-inflammatory medications, physical/occupational therapy, and corticosteroid injections can also be considered. Studies have shown resolution of symptoms in up to 80% of patients following 1-2 corticosteroid injections [77].
Surgical intervention is indicated in refractory cases. The thickened tendon sheath is released dorsally in order to prevent volar tendon subluxation. Underlying intercompartmental septae are also released. Care is taken to protect the superficial radial nerve, which provides sensation to the dorsum between the first and second digits. Golfers are allowed to begin gentle swings with chipping and short irons at about 4-6 weeks postoperative and gradually advance to full return to play [7].
2.2.2. Intersection Syndrome
The abductor policis longus (APL) and extensor policis brevis (EPB) tendons cross over the ECRL and ECRB tendons just proximal to the dorsal retinaculum of the wrist [78]. This “intersection” of tendons can become an area of irritation with overuse, termed intersection syndrome. This has been reported in the leading upper extremity of elite golfers [79].
Commonly reported symptoms include pain, swelling, and crepitus on the dorsum of the wrist, approximately 6cm proximal to Lister’s tubercle [80]. On physical examination, this pain will be aggravated with resisted extension or passive flexion of the wrist.
Providers suspecting this injury may not appreciate any radiographic findings. However, on MRI, edema noted around the APL and EPB tendons would be seen at the point of intersection. Treatment consists of conservative measures, including immobilization and anti-inflammatory medications. Rehabilitation is a conservative option for 8-10 weeks in order to ensure all symptoms have subsided, and motion and strength have recovered. Furthermore, comprehensive education is provided. A corticosteroid injection may be performed into the APL bursa [7]. In rare cases, release of the second dorsal compartment is performed proximal to the radial styloid [78]. A post-operative rehabilitation course includes stretching and progressive strengthening over a 4-6 week span [81].
2.2.3. Extensor Carpi Ulnaris Disorders
Golfers of all skill levels may be afflicted with extensor carpi ulnaris (ECU) tendon disorders. The ECU tendon passes through the sixth extensor compartment of the wrist and inserts at the fifth metacarpal base. Interestingly, the muscles' action depends largely on forearm rotation. It contributes to extension when the forearm is supinated and more towards ulnar deviation when the forearm is pronated [82]. When the forearm is in supination, and the wrist is in flexion in a downswing, the ECU tendon can be predisposed to traumatic injury. This occurs in the form of tenosynovitis, tendinopathy, and tendon instability.
ECU tenosynovitis can occur from repetitive use. On physical examination, patients will have pain to palpation of the ECU tendon. Pain will also increase with resisted extension and ulnar deviation of the wrist. The diagnosis can also be made on ultrasound, which demonstrates anechoic fluid around the ECU tendon [7]. Patients with this injury should avoid golf for 2 weeks, be custom splinted in 30 degrees of extension, and take anti-inflammatory medications. Corticosteroid injections can also be performed [7]. A short course of rehabilitation is beneficial after the immobilization period to restore motion and strength.
ECU tendinosis occurs due to changes in tendon structure due to a sudden distraction force placed on the ECU muscle [74]. Hitting a “fat” shot (the ground before the ball) or hitting off of a harder surface can predispose the ECU to tendinosis. This can manifest as a partial or complete rupture. Disruption of the ECU tendon can lead to secondary changes, including thickening of the tendon or bony spur formation at the ulnar groove [74, 82]. If conservative measures do not alleviate the golfer’s symptoms, surgical intervention can be considered. The septum between the fifth and sixth extensor compartments can be divided into any other tendon defects trimmed or repaired [7].
However, the results of this procedure are not promising, with a reported success of 50% with potential risk of causing iatrogenic instability [83, 84].
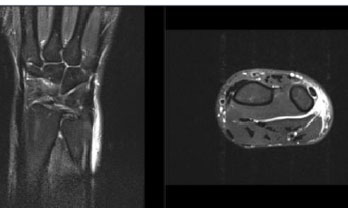
ECU tendon instability is commonly the result of a single traumatic event. Patients note a sensation of “snapping” or “locking” while attempting to engage the ECU muscle. This leads to significant discomfort. To supplement the physical examination, ultrasound or MRI can confirm the diagnosis (Fig. 4) [7]. Non-operative management includes cast immobilization in wrist extension, ulnar deviation, and forearm pronation for 4-6 weeks [85]. Surgical measures may include reconstruction of the tendon sheath with suture anchors [86]. Operative intervention is over 90% effective in treating ECU instability [82]. Rehabilitation protocols emphasize early range of motion and strengthening, permitting return to sport when 80% strength of the contralateral side is reached [82, 86].
2.2.4. Flexor Carpi Radialis Tendinitis
The flexor carpi radialis (FCR) tendon travels within a fibro-osseous tunnel at the proximal border of the trapezium. Within this tunnel, the FCR tendon occupies most of the space within the tunnel directly in contact with the palmar aspect of the trapezium [87]. Thus, inflammation within this tunnel can lead to FCR tendinitis. This is reported to occur in the trailing hand of golfers, likely due to repetitive wrist flexion against resistance at impact [7]. Thus, this can be a source of radial-sided pain for professionals and amateur golfers alike.
Diagnosis is made through a series of maneuvers, including tenderness along the FCR tendon sheath distally and pain with resisted wrist flexion and radial deviation [87, 88]. Radiographic imaging in golfers is largely unremarkable unless the underlying etiology is a prior traumatic injury or arthritis. However, one may see an increased T2 signal around the FCR tendon sheath on MRI imaging [87]. The diagnosis can also be made with the resolution of symptoms with a lidocaine injection.
A majority of patients with FCR tendinitis can be managed non-operatively [7]. Non-operative modalities range from orthosis immobilization and avoidance of play for 4-6 weeks. Patients should consider a course of formal rehabilitative therapy and anti-inflammatory medications to alleviate pain. For refractory cases, a corticosteroid injection or surgical decompression of the FCR tendon sheath may be considered. During surgical intervention, care should be taken to avoid damage to surrounding cutaneous nerves or the FCR tendon itself [88]. Success rates of operative intervention can be as high as 90%, which can be predicted by the improvement in symptoms with corticosteroid injection [88]. Patients managed operatively are typically immobilized for 2 days, with subsequent initiation of range of motion and strengthening until return to play at roughly 6 weeks [89].
2.2.5. Flexor Carpi Ulnaris Tendinitis
The flexor carpi ulnaris (FCU) tendon inserts into the palmar aspect of the pisiform, hook of hamate, and base of the fifth metacarpal. FCU tendinitis is an overuse syndrome and is commonly reported in golf and racket sports [90]. The point of irritation is thought to be along the tendon’s insertion point [56]. Of note, the FCU tendon does not run through a tendon sheath; however, it can get irritated through microtrauma during impact. This commonly occurs in the golfer’s trailing hand [7].
On examination, patients will demonstrate tenderness to palpation of the FCU tendon. Radiographic imaging may show a calcified tendon distal to the ulnar styloid [7]. T2 weighted MRI will also show increased signals or calcifications. For treatment, golfers may consider resting, trialing an orthosis, reducing grip strength, and taking anti-inflammatory medications. Non-operative rehabilitation typically consists of 3-6 weeks of immobilization, followed by a gradual range of motion and strengthening [89]. Surgical management may include performing a z-plasty for tendon lengthening, tendon debridement, or excision of calcifications [91].
2.2.6. Carpal Tunnel Syndrome
Within the wrist lies the carpal tunnel, the space between the palmar flexor retinaculum and dorsal carpal bones. The tunnel contains nine flexor tendons and the median nerve. Carpal tunnel syndrome develops from inflammation and swelling of the tendons that travel within the carpal tunnel [7]. Professional and amateur golfers may begin to notice paresthesias in the median nerve distribution concerning carpal tunnel syndrome. To our knowledge, there have been no reported cases of carpal tunnel related to an acute golfing injury.
Diagnosis can be made with a positive Tinel’s or Phalen’s sign at the wrist [92]. Additionally, the Durkan carpal compression test has been found to be the most sensitive test [93, 94]. Electromyography and nerve conduction studies can be considered; however, these tests appear to have more value in documenting the severity of median nerve neuropathy [95].
Treatment options range from non-operative to operative modalities. Non-operative options include rehabilitation for symptom management, patient education, and ergonomic improvement. A prior report demonstrates that larger diameter and softer grips may facilitate reduced grip pressure [96]. In addition to equipment and swing changes, conventional treatments of carpal tunnel syndrome can also be considered, including anti-inflammatory medications, night-time wrist orthosis, and open versus endoscopic carpal tunnel release for refractory cases [97]. Post-operatively, patients are immo- bilized until stitches are removed at 10-14 days, at which point a gentle range of motion and strengthening are initiated [98]. A short course of rehabilitation is recommended to ensure that the patient has regained the motion and strength required to successfully return to golf. Short iron and chip shots are initiated at 1 month post-operative, where slow advancement to long irons and driver are reached at 12 weeks post-operative [7]. Success rates of treatment are higher than 80% [99].
2.2.7. Triangular Fibrocartilage Complex Injury
The triangular fibrocartilage complex (TFCC) is an important component of static stability at the distal radioulnar and ulnocarpal joints. The TFCC comprises of the articular disc, volar and dorsal radioulnar ligaments, volar ulnotriquetral and ulnolunate ligaments, ulnar collateral ligament, ECU tendon sheath, and the meniscus homologue [100]. The etiology of TFCC injury in golfers appears to be chronic in nature and related to repetitive rotational motion during the golf swing [84]. Acute sprains have been reported during instances of hitting the ball out of the rough.
Golfers facing TFCC injury typically present with ulnar-sided wrist pain, pain with gripping the club, or DRUJ instability [7]. Many physical exam maneuvers have been reported in the literature, including the TFCC compression test, stress test, press test, supination test, piano key test, and grind test [101]. On imaging, plain radiographs can provide insight into ulnar variance. MRI can differentiate between a central versus peripheral TFCC injury [101]. The most accurate method of diagnosis, however, is direct visualization through arthroscopy [101].
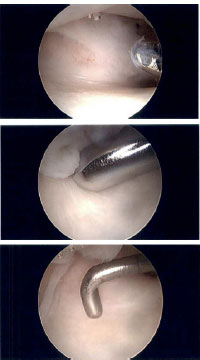
Most golf-related TFCC injuries respond well to non-operative treatment. This includes immobilization in an orthosis, icing, and anti-inflammatory medications [7]. Corticosteroid injections can also be considered. Rehabilitation is beneficial for symptom management, patient education, and progressive restoration of motion and strength once the acute pain has subsided. For more chronic degenerative TFCC injuries, treatment may consist of debridement, restoration of proper joint alignment (to correct mechanical load across the joint), or TFCC reconstruction (Figs. 5a-c). Post-surgical protocols typically call for immobilization for 4 to 6 weeks [7, 101]. This may be extended by an additional 4 weeks if an osteotomy is performed [101]. Post-operative patients are routinely managed in formal rehabilitation for a period of approximately 3 months prior to returning to sport. These procedures are associated with favorable outcomes in high-level athletes [101].
2.2.8. Pisotriquetral Arthritis
Pisotriquetral (PT) arthritis is a common cause of hypothenar wrist pain. As with other arthridies, potential etiologies include genetic, degenerative, and traumatic causes. Golfers with this condition typically experience ulnar-sided palmar wrist pain. Patients typically note pain with grinding of the pisiform along and against the triquetrum. This is known as the pisotriquetral shear test [102]. Narrowing or widening of the PT joint space with flexion and extension, respectively, may indicate instability of the pisiform ligament complex (PLC) [84, 103].
X-ray imaging with dedicated views (centered through the PT joint), CT, and MRI are useful imaging modalities for diagnosis. The PT joint has also been advocated for incorporation into routine ultrasound imaging of the wrist [104]. Corticosteroid injection can be used as a diagnostic and therapeutic modality [103-105]. Golfers with refractory pain may require pisiform excision [103]. This is now being performed with a minimally invasive arthroscopic approach [106]. To our knowledge, rehabilitation following pisiform excision has not been well-defined.
2.3. Hand
In addition to the wrist, injury to the hand is quite high among golfers [56, 75]. The hand most commonly injured is the lower leading hand (i.e., the left hand for a right-handed golfer) [107]. Hand injuries can be either acute or chronic, ranging from tenosynovitis and vascular injury to acute fracture.
2.3.1. Trigger Finger
Annular (A) pulleys form fibro-osseous tunnels, through which the flexor tendons travel along the palmar aspect of the digits. After long hours of practice or a significant number of holes played, many golfers of all skill levels begin to feel clicking, locking, or pain in one or more of their digits. This is concerning for trigger finger (stenosing tenosynovitis), which at baseline has a prevalence of 2-3% in the general population [9]. The etiology of the trigger finger is multifactorial in nature, including genetics, trauma, and degenerative changes [108]. Of note, there have been implications with repetitive power grip and maintained flexion as contributing factors [108-110]. These disturbances lead to hypertrophy of the A1 pulley and subsequent impingement of the flexor digitorum superificialis and profundus tendons [108].
Symptoms can range from vague pain to being unable to extend the affected digit at the proximal interphalangeal (PIP) joint. Golfers may notice an inability to swing smoothly because of these symptoms. Diagnosis is usually made with visualized popping and catching with active extension at the PIP joint [108]. In addition, swelling and tenderness to palpation can be appreciated at the A1 pulley [108]. Ultrasound can be used to observe static and dynamic mobility of the flexor tendons in addition to a hypertrophied A1 pulley [111].
Management consists of a short course of rehabilitation to focus on activity/grip modification and custom orthosis fabrication. In addition, symptoms may resolve spontaneously with anti-inflammatory medication and immobilization of the PIP joint. Over 50% of patients have complete symptom relief from management with these strategies alone [112]. Corticosteroid injections, described as early as 1953, are the second line of treatment. Patients with diabetes mellitus, long-standing disease, and multi-digit involvement may not benefit from this treatment [108]. For refractory cases, percutaneous versus open release of the A1 pulley can be considered. A concern for percutaneous release involves potential damage to digital nerves, arteries, and flexor tendons [108]. The open release allows for wider exposure and improved visualization of the entire A1 pulley for surgical release. Mobilization is initiated at 2 days post-operative and advanced as tolerated based on the patient’s comfort level.
2.3.2. Hook of Hamate Fracture
Hook of hamate fractures are one of the few acute injuries that golfers face. It exclusively occurs in the leading hand from a direct blow to the end of the golf club [113]. This is most likely to occur during the downswing with direct impact on a hard surface, such as a rock or the cart path [10]. Golfers with shorter club lengths may be predisposed to this injury as the end of the club is in direct contact with the hook of the hamate [7].
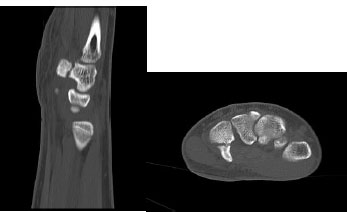
Patients generally complain of focal pain in the hypothenar eminence [113]. Some may complain of numbness and tingling in the ring and small fingers if there is associated involvement of the adjacent ulnar nerve. It may be difficult to identify a fracture line on standard radiographic imaging of the hand [114]. A carpal tunnel view of the wrist in full extension may be performed; however, this can be difficult to obtain if the patient is in significant pain [114]. The gold standard of diagnosis is CT imaging, which is 97-100% sensitive for diagnosis (Figs. 6a and b) [115]. Associated flexor tendon tears have been reported. This is further evaluated using ultrasound imaging [85]. EMG can also be considered to rule out ulnar nerve involvement [114].
Non-operative management includes cast immobilization for 6-12 weeks [116]. Displacing forces from the pisohamate ligament, flexor digiti mini brevis, and opponens digit minimi tendons lead to high rates of non-union (reported above 40%) [116, 117]. Thus, providers generally elect to recommend operative treatment in hopes of allowing for an earlier range of motion and return to play. Options include surgical excision and open reduction internal fixation with headless compression screws. Neurolysis of the deep motor branch of the ulnar nerve or Guyon’s canal release may also be performed [118]. There is favorable evidence for operative versus non-operative treatment of these injuries in high-level athletes [119]. In one case series, all eight golfers who underwent surgical excision were able to return to play, though complications of transient ulnar neuropathy and painful scarring were noted in five golfers [120]. Formal progressive rehabilitation plays a role post-operatively. Patients are placed in a resting orthosis for 2 weeks, with gradual initiation of strength and range of motion exercises at that time [120]. This is opposed to prolonged periods of immobilization (6 weeks) for patients who undergo open reduction internal fixation. Golfers return to play at approximately 6 weeks [120].
2.3.3. Hypothenar Hammer Syndrome
The ulnar artery travels through Guyon’s canal as it crosses the hamate bone, where it divides into the superficial and deep palmar branches. Hypothenar Hammer Syndrome (HTHS) is characterized by a vasospasm in the superficial palmar branch of the ulnar artery [121]. This leads to either thrombosis or aneurysm formation, depending on the extent of disruption of the arterial wall.
Symptoms can be highly variable, including digital pain (commonly in the 2nd-5th digits), cold sensitivity, blanching or discoloration of the fingertips, finger claudication, or hypothenar pain. Repetitive trauma is the presumed etiology of this condition, as the hook of the hamate acts as an anvil against the ulnar artery through repetitive motion [121, 122].
Though rare in incidence, golfers can be at higher risk of developing this condition. It has been reported to occur in the leading hand of the golf swing [122]. This is likely due to the direct impact of the end of the club on the hypothenar eminence. This occurs more frequently in amateur players, who often grip the club too tightly [122]. Diagnosis can be made with ultrasound or CT/MR angiogram. This will reveal a “corkscrew” formation of the ulnar artery with an associated occlusion or aneurysm at the level of the hook of the hamate [121-124].
Treatment is guided by duration, pathology, and the digital brachial index. For patients with thrombosis greater than 2 weeks, lifestyle modifications, including activity modification and smoking cessation, demonstrate great efficacy (80%) [121, 123-125]. For patients with thrombosis without an aneurysm less than 2 weeks, endovascular fibrinolysis can be considered [123, 125, 126]. For patients with a digital brachial index greater than 0.7, arterial ligation can safely be performed [123, 125, 126]. Patients with severe ischemia, thrombosis with aneurysm, and failed conservative treatment may require segment excision and primary anastomosis versus vein grafting [125, 126]. Currently, there is no consensus on the optimal treatment for the latter group [127]. Graft patency rates at 2 months post-operative is approximately 84% [128].
CONCLUSION
An increased international presence has led to golf’s popularity as a recreational and competitive sport. The sport is dynamic in nature, such that golfers are prone to a variety of upper extremity injuries at the shoulder, elbow, forearm, wrist, and hand. It is important for front-line medical providers to appreciate and explore the injury patterns that can occur at specific phases during the golf swing in order to guide the patient athlete through optimal medical, surgical, and rehabilitative management.
The rehabilitation for upper extremity injuries in golfers should include discussions beyond the traditional restoration of motion, strength and endurance. Return to the sport of golf requires a basic understanding of the mechanics of the golf swing as well as a gradual and controlled integration of subskills to prevent re-injury. As medical providers, it is important to recognize the broad differential diagnosis of injuries that may occur in golfers and to best address each in order to facilitate their safe return to play.
LIST OF ABBREVIATIONS
| METs | = Metabolic equivalents |
| AC | = Acromioclavicular |
| SLAP | = Uperior labral anterior to posterior |
| GH | = Glenohumeral |
| MRI | = Magnetic resonance imaging |
| EMG | = Electromyography |
| ECRB | = Extensor carpi radialis brevis |
| EDC | = Extensor digitorum communis |
| EDM | = Extensor digiti minimi |
| APL | = Abductor pollicis longus |
| EPB | = Extensor pollicis brevis |
| FCR | = Flexor carpi radialis |
| TFCC | = Triangular fibrocartilage complex |
| PT | = Pisotriquetral |
| PLC | = Pisiform ligament complex |
| A | = Annular |
| PIP | = Proximal interphalangeal |
| HTHS | = Hypothenar hammer syndrome |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declared no conflict of interest, financial or otherwise.
ACKNOWLEDGMENTS
Declared none.


