All published articles of this journal are available on ScienceDirect.
Arthroscopic Partial Meniscectomy with Suture Repair for Discoid Lateral Meniscus in Patients under 40 Years of Age
Abstract
Background:
Damage to a discoid meniscus often indicates a complex tear, the treatment for which has not yet been resolved. This study aimed to assess the clinical efficacy of arthroscopic partial meniscectomy with suture repair for discoid lateral meniscus in patients under 40 years of age.
Methods:
A total number of 10 patients aged < 40 years who underwent partial meniscectomy with meniscal repair for lateral discoid meniscal tears were included in the study. Clinical assessment was evaluated pre-and post-surgery, and magnetic resonance imaging was performed at a mean of 9.5 months after surgery.
Results:
The Lysholm score improved from 43 ± 19.3 to 87.2 ± 7.8 (range: 94 − 100) at the last follow-up after surgery. The International Knee Documentation Committee score improved from 21.8 ±10.4 to 87.7 ± 4.8 at the last follow-up time after surgery. MRI revealed partial healing of the meniscus in six patients and residual damage of the meniscus in four patients. Extrusion was noted in three patients shown in coronal plane images.
Conclusion:
Arthroscopic partial meniscectomy with suture repair for discoid lateral meniscus in 10 patients under 40 years of age led to satisfactory clinical outcomes after a mean period of 11.2 months. However, in three cases, although the symptoms have improved, the remaining meniscus had worn off.
1. INTRODUCTION
A discoid meniscus is a congenital malformation and is said to be more common in Asians than in Westerners [1-5]. The lateral discoid meniscus is more common than the medial discoid meniscus [6]. Owing to its anatomical form, injury often develops without a clear trigger, such as trauma. In addition, congenital malformation often leads to malformation of the lateral femoral condyle. A higher age of onset is associated with a greater degree of malformation of the lateral femoral condyle and varied the morphology of the injury.Damage to a discoid meniscus often indicates a complex tear. The treatments for a torn discoid meniscus include total meniscectomy, partial meniscectomy, and partial meniscectomy with repair. The meniscal function of the residual discoid meniscus should be preserved. Therefore, we performed a partial meniscectomy with repair to preserve as much of the meniscus as possible.
2. METHODS AND MATERIALS
A total number of 23 patients underwent arthroscopic surgery for symptomatic lateral discoid meniscus between June 2013 and December 2020 at our institute. A total of 10 patients who underwent partial meniscectomy with meniscal repair for lateral discoid meniscal tears were selected. The exclusion criteria included patients who did not undergo partial meniscectomy with meniscal repair and age older than 40 years. The group was composed of five males and five females with a 22 ± 9.0 years (14 − 40 years) mean age at the time of surgery. The time between the appearance of symptoms and the operation was 2.6± 2.5 months (1 − 9 months). The mean follow-up time was 11.2 ± 3.7 months (5 − 13 months) (Table 1).
| Characteristic | Value |
| Mean age | 22± 9.0 |
| Gender (male/female) | 5/5 |
| Side, right/left | 6/4 |
| Duration of symptoms, month | 2.6± 2.5, (1-9) |
| Follow-up time, month | 11.2± 3.7 |
The discoid meniscus was classified intraoperatively using the Watanabe classification [7]. An inside-out meniscal repair technique was employed, and non-absorbable material was used. Meniscal stimulation, such as fibrin clot, was used in two cases.
2.1. Clinical Assessment
Clinical evaluations were performed using the Lysholm and Subjective International Knee Documentation Committee (IKDC) 2000 scores pre-and post-surgery. Radiological evaluations were performed using magnetic resonance imaging (MRI) examination at a mean of 9.5 months after surgery.
2.2. MRI Technique
MRI was performed on a 1.5 T system (Signa, General Electric Medical Systems, Milwaukee, WI) using a dedicated send-receive extremity coil (General Electric). All MRI studies were interpreted by an experienced musculoskeletal radiologist (HP) [5]. Statistical analysis was performed using R2.8.1. The Mann-Whitney U test and Welch t-test were used for the comparison procedure [8].
3. RESULTS
As per the Watanabe classification, seven and three patients had complete and incomplete discoid meniscus, respectively. Four longitudinal tears, four horizontal/complex tears, and two radial/horizontal tears were observed (Table 2).
| Factors | Value |
| Injury pattern | - |
| Longitudinal | 4 |
| Horizontal/complex | 4 |
| Radial/horizontal | 2 |
| Anatomic type | - |
| Complete | 7 |
| Incomplete | 3 |
3.1. Clinical Assessment
The patients’ mean preoperative Lysholm score was 43 ± 19.3 (range: 14−66). The mean postoperative score was 87.2 ± 7.8 (range: 94−100) at the last follow-up after surgery (p<0.001). The patients’ mean preoperative IKDC score was 21.8 ± 10.4 (range: 8−35.6). The mean postoperative score was 87.7 ± 4.8 (range: 79.3−93.1) at the last follow-up after surgery (p<0.0001) (Table 3).
| Factors | After Op. |
| Extrusion | - |
| Sagittal 1/3~2/3 | 1 |
| Coronal 1/3~2/3 | 2 |
| 1/3 > | 1 |
| Repair | - |
| Healed | - |
| Partly healed | 6 |
| Residual damage, wear out | 4 |
3.2. MRI Evaluation
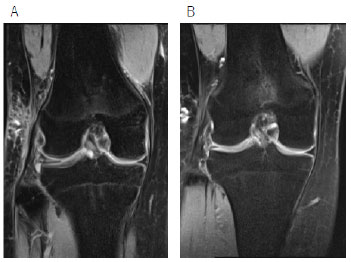
MRI revealed partial healing that the signal intensity of the meniscus was improved in six patients, and residual damage of the meniscus in four patients at 9.5 months (5 − 12 months) after surgery (Table 3). Extrusion and wear out of the meniscus were noted in three patients, as observed in the coronal plane images (Fig. 1).
4. DISCUSSION
Most of the patients with asymptomatic discoid meniscus do not require any treatment. Surgical treatment, including total open or arthroscopic meniscectomy, is performed when symptoms, such as pain and blockage, occur. However, several reports suggest a direct correlation between total meniscectomy and progression to osteoarthritis over time [9-11]. Currently, to preserve meniscal function, partial meniscectomy with reshaping or meniscal saucerization is performed. Arthroscopic partial meniscectomy is commonly recommended to change the meniscus to a normal shape and size; a 6 – 8 mm width of the remaining meniscus is advised [12-14]. In cases of peripheral tear, an arthroscopic meniscal repair can be performed with saucerization. The current treatment of choice for a torn discoid lateral meniscal is preservation with or without repair based on peripheral rim instability [9, 13-15]. The degree of meniscus resection is reportedly associated with the progression of degenerative changes. Ahn et al. reported that arthroscopic reshaping for symptomatic discoid lateral meniscus in children led to satisfactory clinical outcomes after a mean of 10.1 years. However, progressive degenerative changes appeared in 40% of the patients [16].
The normal meniscus is a fibrocartilage structure containing an abundant extracellular matrix. Meniscus contains collagen type I (most common), II, and III and acid mucopolysaccharides. It includes the vascular area, which lies within 3-5 mm of the peripheral rim [17-19]. On the other hand, Atay et al. reported collagen fibers to be fewer and to have a heterogeneous course in discoid meniscus compared to normal meniscus [20]. Papadopoulos et al. reported that disorganization of the circular collagen fiber system in the discoid meniscus matrix contributes to the pathogenesis of the high tear and degenerative lesion rate observed among menisci with discoid configuration [21]. Tudisco et al. reported that a discoid lateral meniscus is different from a normal meniscus in terms of distribution and shape of the cells, vascularity, and organization of collagen fibers, irrespective of the age of the patients [22].
Normal menisci are wedge-shaped semilunar tissues that stabilize the femoral condyle as it articulates against the tibial plateau. Reshaping or meniscal saucerization with repair can be performed, although gaining normal function is difficult in a discoid meniscus that has been reshaped with meniscal repair. Ahn et al. reported that progressive degenerative changes appeared in some patients who underwent arthroscopic reshaping for symptomatic discoid lateral meniscus [1]. In our study, even though one patient’s symptoms improved, the meniscus that was reshaped with repair for a complete type with horizontal rupture in the anterior portion, degenerative rupture in the middle portion, and longitudinal rupture in the posterior segment was worn out one year after surgery. The degenerative and extensively damaged discoid lateral meniscus is more likely to wear and extrude, even if partial meniscectomy with meniscal repair is performed. In the normal meniscus, Arnoczky and McAndrews reported that in the normal meniscus, some reorganization of the matrix may take place because of changes in the mechanical environment [10, 17]. In our case, the absence of healing may have caused the remaining meniscus to rapidly wear and extrude owing to the histological features of the discoid lateral meniscus.
5. LIMITATIONS
Our study had some limitations, including the small number of patients, the retrospective design of the study, no control group, and the lack of long-term follow-up. In addition, follow-up arthroscopy was not performed. Despite these limitations, the present study contributes to the current understanding of the possibility of partial meniscectomy with repair for lateral discoid meniscus.
CONCLUSION
Arthroscopic partial meniscectomy with meniscal repair for lateral discoid meniscal tears led to satisfactory clinical outcomes in patients under 40 years of age. However, the meniscus that was reshaped with repair was worn out one year after surgery in one patient. Although the reasons are not clear, histological features of the discoid meniscus might have caused this finding.
AUTHORS’ CONTRIBUTION
TM designed the study, analyzed the data, and wrote the manuscript. MS, KI, RK, YT, and TY collected the data and participated in the design of the study. HN analyzed the data and helped in writing. All authors have read and approved the final manuscript.
LIST OF ABBREVIATIONS
| MRI | = Magnetic Resonance Imaging |
| IKDC | = International Knee Documentation Committee |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethical Review Boards of Kanmon Medical Center (Shimonoseki, Japan).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The authors are unable to share raw data because ethical approval was not obtained for data sharing. In addition, informed consent for data sharing was not obtained from the individuals. Please find all summarized datasets reported in the results section and the tables.
FUNDING
This research was supported by the commissioned research expenses to Kanmon Medical Center (Shimonoseki, Japan) from Kyocera Japan and Japan Medical Dynamic Marketing INC.
ACKNOWLEDGEMENTS
Declared none.


