CASE REPORT
Tibial Tubercle Avulsion Fracture in a Case of Pre-existing Osgood-schlatter Disease
Takatomo Mine1, *, Takuho Matusita1, Michio Shinohara1, Ryutaro Kuriyama1, Yasunari Tominaga1, Koichiro Ihara1, Takanori Yonehara1
Article Information
Identifiers and Pagination:
Year: 2023Volume: 17
E-location ID: e187432502306160
Publisher ID: e187432502306160
DOI: 10.2174/18743250-v17-e230714-2023-1
Article History:
Received Date: 11/01/2023Revision Received Date: 19/05/2023
Acceptance Date: 31/05/2023
Electronic publication date: 07/08/2023
Collection year: 2023

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
Osgood-Schlatter's disease (OSD) is a well-known condition; however, a tibial tubercle avulsion fracture following an OSD is rare. We reported a case of tibial tubercle avulsion fracture with pre-existing OSD in a 12-year-old boy.
Case Presentation:
A 12-year-old boy had right knee pain and could not walk after kicking a ball with his right leg during a soccer game. He had been diagnosed with OSD at another hospital 2 months previously. He was then diagnosed with a right tibial tubercle avulsion fracture. The fragment was thin, and the patient was treated with internal fixation using cannulated cancellous screws. The patient demonstrated near-normal knee function and was allowed to return to sporting activities 6 months postoperatively.
Conclusion:
In this case, the tibial tubercle avulsion fracture might have been associated with OSD. Care should be taken while treating OCD to prevent tibial tubercle avulsion fractures.
1. INTRODUCTION
Extensor mechanism injury during sporting activities is relatively rare in childhood [1-9]. Acute tibial tubercle avulsion fractures are also uncommon. Conversely, Osgood-Schlatter's disease (OSD), a condition with a favorable prognosis that causes tibial tuberosity damage due to contraction of the quadriceps muscle, occurs frequently in childhood [10, 11]. Whether OSD is a risk factor for tibial tubercle avulsion fracture remains controversial. We reported a case of tibial tuberosity avulsion fracture in a patient with pre-existing OSD.
2. CASE PRESENTATION
A 12-year-old boy complained of left knee pain two months earlier. He was diagnosed with OSD at another hospital and was undergoing conservative treatment with follow-up. After the diagnosis, he continued to play football because he belonged to the boys' soccer club.
The patient had sudden right knee pain and was unable to walk after kicking a ball with his right leg during a football game. He was diagnosed with a right tibial tubercle avulsion fracture at another hospital and was referred to our hospital for treatment. His past medical history and family history were unremarkable.
Physical examination revealed swelling, tenderness, and localized warmth in the right knee joint.
X-ray images showed an avulsed fracture fragment in the proximal right tibia (Fig. 1).
Computed tomography (CT) showed a cortical bone defect at the patellar tendon insertion and a thin avulsion fragment in the proximal tibia (Fig. 2).
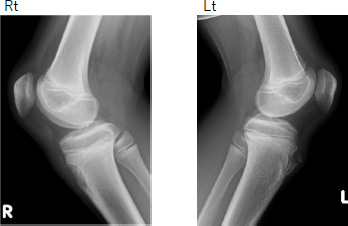 |
Fig. (1). Preoperative X-ray image. Lateral view. |
Magnetic resonance imaging demonstrated a cortical bone defect at the patellar tendon insertion and no rupture in the patellar tendon; however, a high intensity in the peripheral part of the patellar tendon was observed (Fig. 3).
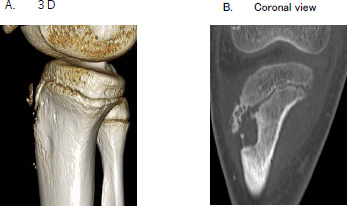 |
Fig. (2). Computed tomography. (A) 3D. (B) Coronal view. |
 |
Fig. (3). Preoperative magnetic resonance imaging. T2-weighted image, sagittal view. |
A surgery was performed using the anterior approach. The avulsed fracture fragment was reduced, stabilized using a Kirschner wire (1.8mm in diameter), and fixed using two cannulated cancellous screws with washers. The fixed fracture was reinforced using a non-absorbable suture (Fig. 4).
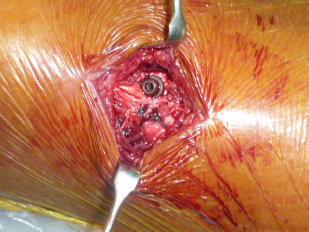 |
Fig. (4). Intraoperative view. The avulsed fracture fragment was fixed using two cannulated cancellous screws with washers and was reinforced using a non-absorbable suture. |
For 2 weeks after the surgery, a knee brace locked at 20° of flexion was applied, and weight bearing was prohibited. Full weight bearing was achieved 6 weeks postoperatively.
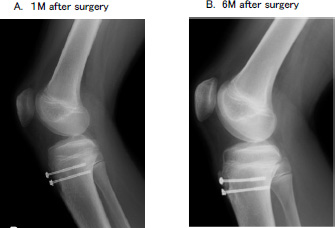 |
Fig. (5). Postoperative X-ray image. (A) Lateral view at 1 month after surgery. (B) Lateral view at 6 months after surgery. |
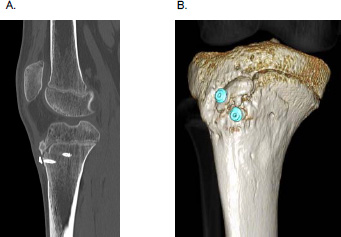 |
Fig. (6). Postoperative computed tomography. (A) Sagittal view. (B) 3D. |
At 6 months postoperatively, the patient had no pain and was able to resume daily activities. Full range of motion and no extensor lag were observed during the straight leg raise test. X-ray images demonstrated that bone union was almost complete; however, one proximal screw was slightly curved (Fig. 5). CT demonstrated complete bone union (Fig. 6). We expected that removing the screw would be difficult or that the screw might be broken. However, the screws were easily removed. The patient had a Lysholm knee score of 99 and was allowed to return to sporting activities.
3. DISCUSSION
Tibial tubercle avulsion fractures reported in children account for 0.4 -2.7% of epiphyseal injuries and less than 1% of physeal injuries [4, 5, 8]. Studies have reported that strong contraction of the quadriceps femoris muscle during leg extension causes failure of the physis at the patellar tendon insertion. An imbalance between rapid bone growth and muscle-tendon growth in adolescents is considered a risk factor for this condition.
In OSD, the proposed mechanism for the development of painful bony nodules at the patellar tendon insertion is repetitive injury from forceful contraction of the quadriceps muscle during jumping and sprinting movements. OSD has been reported to be a risk factor for tibial tuberosity avulsion fracture, although the scientific evidence remains inconclusive [12-19].
Regarding the relationship between pediatric tibial tubercle avulsion fractures and OSD, a history of OSD is present in 20-75% of patients with tibial tubercle avulsion fractures [1-3]. In addition, the time from the diagnosis of OSD to avulsion fracture ranges from 3 weeks to one year [13-17]. Several studies have reported that the structural weakening of the physeal cartilage secondary to repetitive stress in OSD and fibrocartilaginous maturation of the patellar tendon may increase the risk of avulsion injury. A tibial tubercle avulsion fracture is classified into various types by Watson-Jones and Ogden [6, 7]. Depending on their fracture morphology, tibial tubercle avulsion fractures may or may not be associated with OSD. The fracture type and history in this present case supported the hypothesis that patients with OSD are at an increased risk of having tibial tubercle avulsion fractures. Therefore, early detection and treatment of OSD may contribute to the prevention of tibial tubercle fractures.
There are various treatment methods for pediatric tibial tubercle avulsion fractures, such as fixation using K-wires, cannulated screws, compression plates, and suture anchoring. In this case, fixation using two cannulated cancellous screws was performed with suturing of the surrounding periosteum, and good fixation was obtained. The postoperative course was also favorable. At 6 months postoperatively, X-ray images demonstrated that bone union was almost complete; however, one proximal screw was slightly curved.
The slight curvature of the proximal screw might be related to the growth of the tibial tuberosity or the stress caused by the contraction of the quadriceps femoris muscle. To prevent this complication, we considered that using solid cancellous screws rather than cannulated cancellous screws for tibial tubercle avulsion fractures in children is important.
LIST OF ABBREVIATIONS
| OSD | = Osgood-Schlatter's Disease |
| CT | = Computed Tomography |
| MRI | = Magnetic Resonance Imaging |
| K-wire | = Kirschner Wire |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not Applicable.
CONSENT FOR PUBLICATION
We have obtained consent from the patient and his family to publish this case report.
STANDARDS OF REPORTING
Care guidelines were followed for conducting this research.
FUNDING
This research was supported by the commissioned research expenses to Kanmon Medical Center (Shimonoseki, Japan) from Kyocera Japan and Japan Medical Dynamic Marketing ING.
AVAILABILITY OF DATA AND MATERIALS
Not Applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.








