All published articles of this journal are available on ScienceDirect.
Anxiety and Osteoarthritis Disability: Updated Overview and Commentary
Abstract
Introduction:
Osteoarthritis, a widespread highly painful often incapacitating joint disease continues to impose immense personal and societal challenges among adults of all ages, especially among older adults. In the absence of any effective cure or treatment, it has become essential to explore all correlates of this chronic disabling disease, especially those that might be preventable or modifiable. Anxiety, a potentially remediable state of mental distress - found linked to chronically disabling forms of arthritis, in various imperceptible ways, and which may have an immense bearing on the outcomes of osteoarthritis, has not received as much attention in the related literature as other topics, such as surgery.
Objective:
In line with previous promising work, this narrative review elected to explore the extent to which current researchers in the field are pursuing this topic, and if so, the degree to which prevailing peer-reviewed data sources support an important role for continued research in this realm, and in what regard.
Methods:
Primarily explored were the key databases housing relevant publications that emerged over Aug 1, 2018-Feb 26, 2020 using the keywords Osteoarthritis and Anxiety. Using a descriptive approach, the relative progress made over the past five previous years in this regard was assessed, in addition to what joints have been studied and with what frequency, and how the degree of interest compares to other currently researched osteoarthritis themes. The potential for intervening in the osteoarthritis pain cycle by addressing anxiety was also examined.
Results:
Findings show a high level of current interest in this topic, and that despite the paucity of prospective studies, studies on joints other than the knee and hip joints, some equivocal conclusions, small numbers of anxiety-related studies compared to other topics, and substantive design limitations, it appears that future research in this realm is strongly indicated.
Conclusion:
This topic if examined further is likely to produce highly advantageous results at all stages of the osteoarthritic disease process and in the context of primary, secondary, as well as tertiary measures to ameliorate osteoarthritis pain and disability.
1. INTRODUCTION
Osteoarthritis, the most prevalent musculoskeletal condition affecting older adults commonly produces varying degrees of local pain in and around one or more freely moving joints, such as the hip and knee joints. At the same time, the presence of unrelenting osteoarthritis pain often increases the risk for - or exacerbates concurrently associated chronic health conditions [1], such as obesity, osteoporosis, and depression, while lowering life quality. Its successful remediation or resolution is however, not readily accomplished, despite years of research, and although highly sought, intervening to alleviate osteoarthritis disability or retard its progression remains an extremely challenging undertaking at best. Indeed, despite their overall success rates in ameliorating pain and dysfunction, joint replacement surgeries, as well as selected pharmacologic interventions, which may be helpful, are not universally indicated, or risk free, and do not reverse the disease process, and often do not fully restore function or reduce pain sufficiently and consistently.
In this regard, anxiety, an emotional response to a real or perceived threat, that may also exist independently or concurrently as a prevailing mental state is not only quite prevalent among adults in general, but more so among adults with a variety of medical disorders [2], such as osteoarthritis in particular [3]. Indeed, increasing research shows that while osteoarthritis is largely considered a biomechanical disease, anxiety may still have a role to play in its pain, disability, and disease progression cycle, even if this not explicitly acknowledged as one of the six osteoarthritis phenotypes recently described [4]. That is, anxiety in its various forms may not only be present in sizeable numbers of cases with osteoarthritis, as this population is usually in their advanced years, but in consideration, that osteoarthritis is the most prevalent disabling musculoskeletal disorder among this population who commonly experience persistent disease associated pain and possibly pain and discomfort from concurrent illnesses. As such, it seems reasonable to suggest that the presence of anxiety, which commonly denotes a state of apprehension and distress, will be quite prevalent in osteoarthritis patients who have advanced mobility and pain problems, especially if efforts to uncover and intervene upon any attendant or inherent proclivity to anxiety are not forthcoming.
To support the above propositions, and in light of the failure of modern medicine to attenuate the personal and societal costs of osteoarthritis in any meaningful way, including the burgeoning use of opiate derivatives, this current review aimed to examine the most recent data concerning this issue. A second goal was to establish the degree of progress in this realm in recent years and whether there is sufficient ongoing support for expanding upon the current research base in this regard, and if so, in what respect. A third goal was to explore whether screening for anxiety is indicated, and if so, what approach might be most practical, along with any definitive intervention approaches that have been proposed to counter anxiety in people with osteoarthritis.
2. METHODS
Since there are several summary reports that discuss this topical theme in the current database [5], this present report was delimited to an analysis of those data published in the past six years as reviewed over two distinctive time periods in order to examine the rate of current progress being made in this sphere of research. Stemming primarily from salient publications housed in PUBMED, this current review incorporates almost all salient publications in that database, if not all key topical reports published since 2014. However, to ensure a comprehensive report, the search strategy employed was supplemented using GOOGLE SCHOLAR, SCOPUS, ACADEMIC SEARCH COMPLETE, and WEB OF SCIENCE CONSOLIDATED databases over the same time period. Primary search terms used in all instances were Osteoarthritis and Anxiety, and others noted in Table 1. In this regard, all apparently pertinent reports were downloaded and carefully scrutinized. Those selected were summarized in a narrative manner given the diversity of the material, as well as a sizable number of research design issues.
| Key Terms Applied |
Search 1 Jan 2014-Aug 2018 |
Search 2 Aug 2018-Feb 2020 |
% Increase Tme 1-2 |
|---|---|---|---|
| Osteoarthritis | 24475 | 9756 | 40 |
| Osteoarthritis + Treatment | 15726 | 5840 | 35 |
| Anxiety + Treatment | 32258 | 10159 | 31 |
| Osteoarthritis + Pain | 8365 | 3438 | 41 |
| Anxiety + Pain | 8577 | 3546 | 41 |
| Osteoarthritis + Anxiety | 249 | 212 | 85 |
| Osteoarthritis + Anxiety +Treatment | 165 | 75 | 45 |
| Osteoarthritis + Anxiety + RCT | 53 | 18 | 34 |
| Osteoarthritis + Anxiety + Surgery | 117 | 47 | 40 |
| Anxiety + Arthroplasty Revision | 16 | 3 | 19 |
| Osteoarthritis + Depression | 474 | 237 | 50 |
To examine whether the present topic is being sufficiently explored, as recommended by earlier authors [5], the degree to which anxiety is currently being increasingly explored as an independent correlate of osteoarthritis was compared over two distinctive time periods, as well as to the research volume of other topics published in the related research realm over the same periods. Which osteoarthritic joints have been studied recently, and to what degree, was also examined, as were suggestions for intervening upon anxiety among osteoarthritis cases.
The term anxiety as applied in this report refers either to anxiety in general or trait anxiety versus state anxiety given the fact that there is no clear differentiation among these sub-categories of anxiety in much of the related osteoarthritis literature.
Since it was observed that this topic has only been studied in a limited fragmented manner, data from all forms of research design and obtained using any type of anxiety survey, as well as data emanating from osteoarthritis of any type or joint were deemed acceptable. Excluded were reports published prior to 2014, those that predominantly examined pain catastrophizing, or mixed cohorts of arthritis or depression alongside anxiety with no differentiation. Readers seeking a prior overview of this topic can refer to [5].
3. RESULTS
3.1. General Observations
As outlined in Table 1, showing some comparative research data over the past six years, it appears that despite its possible clinical relevance, only a very modest relative interest in the present topic of anxiety prevails, when weighed against other topics of osteoarthritis research. However, this interest is increasing more markedly, than other related health topics, as indicated. In addition, while Table 2 shows very few recent studies that have specifically discussed a role for anxiety as a potentially important osteoarthritis disease correlate in joints other than the knee and hip joints, the study of anxiety in multiple forms of osteoarthritis is increasing. Moreover, despite the significant increase in related research publications on anxiety as associated with osteoarthritis over the last 18 months, information relative to anxiety in the context of joint replacement surgery clearly shows this correlate to be of increasing relevance in mediating long term outcomes. The number of randomized trials that are potentially linked to the amelioration of anxiety symptoms in osteoarthritis, while increasing numerically, is still very low, if compared to reported interventions on this topic, in general, however.
| Osteoarthritis Type |
Time Period Jan 2014-Aug 2018 |
Time Period Aug 2018-Feb 2020 |
% Increase Time 1-2 |
|---|---|---|---|
| Knee | 249 | 65 | 26 |
| Hip | 34 | 16 | 47 |
| Spine | 24 | 11 | 46 |
| Shoulder | 3 | 5 | 166 |
| Hand | 22 | 5 | 23 |
| Neck | 11 | 3 | 27 |
| Temporomandibular | 1 | 1 | 100 |
| Foot | 6 | 1 | 17 |
| Wrist | 2 | 3 | 150 |
| Thumb | 3 | 2 | 67 |
These numbers as detailed on PUBMED are arguably not a precise reflection of the state of the art because search terms were limited and hence other data may have been overlooked. However, no further information was forthcoming when employing the same strategy for GOOGLE SCHOLAR, SCOPUS, ACADEMIC SEARCH COMPLETE and WEB OF SCIENCE CONSOLIDATED databases. Nonetheless, as in all the databases reviewed, the number of PUBMED data listings clearly overestimate numbers of salient research publications focusing on the specific topic of anxiety and osteoarthritis, since a sizeable number of housed articles only detailed depression or peripheral or central sensitization issues, or other forms of comorbid illnesses. Gaining a clear picture of what role anxiety plays or does not play in osteoarthritis, is further challenged by the presence of studies using mixed samples, samples with no clearly defined osteoarthritis, the application of unsubstantiated osteoarthritis treatment approaches, or proposed protocols, rather than completed intervention studies.
Confusion also arises when trying to organize the data for aggregation purposes because the definitions of anxiety are multiple, but not always stated, the instruments used to examine anxiety differ widely, and are commonly based on self-reports, with no clear clinical validation, or universally applied survey scoring procedures. The prevailing degrees of joint pathology, age ranges, and comorbid disease profiles studied are also highly diverse and not always clearly factored into the analyses. Surprisingly too, is the almost complete absence of any current documentation concerning the prevailing extent of any anxiety prevalence in a particular research sample, even when surveys are used, thus it is impossible to discern if anxiety rates are increasing, decreasing, or remaining static, or are clinically important or not; for example, whether they denote the possibility of a specific osteoarthritis sub-grouping, or are affected by gender, age, obesity, and extent of numbers of affected joints. Instead, most current researchers appear to have assumed anxiety as likely to exist in some form among osteoarthritis sufferers, and have thus applied this assumption as the rationale for examining the interrelationships of anxiety to the disease and its presentation and outcomes. However, in both related studies with significant results, as well as those with ‘null’ results, the percentage of cases with or without clinical anxiety is commonly impossible to estimate, and with very few carefully controlled prospective studies, the ability to estimate and record the independent or interactive effects or both of anxiety in adults with any form of osteoarthritis is virtually impossible at best.
Regardless of these shortcomings and others though, as outlined in several presently reviewed studies, screening osteoarthritis patients for anxiety appears warranted, especially for patients scheduled for surgery, and those with an anxiety history. But how and when this should be done and by whom is generally unclear as there seems to be little uniformity as regards the various instruments used in the related literature to screen for anxiety among people with osteoarthritis. Most anxiety assessment tools too, are somewhat complex research-oriented surveys that have not necessarily been validated for osteoarthritis cases, rather than practical clinical tools. Moreover, whether all or any have adequate as well as comparable measurement properties, adequate reliability and are sensitive to change in the context of progressively disabling osteoarthritis disease manifestations is not clear. The degree of accuracy when using these surveys listed in Table 3 is also in question because some may not capture all features of osteoarthritis that may provoke anxiety, while others may not clearly differentiate anxiety from depression or stress.
| Research Group | Key Findings and Conclusions | ||
|---|---|---|---|
| Ali et al. [53] | Preoperative anxiety predicted dissatisfaction after knee arthroplasty surgery using the Hospital Anxiety and Depression Scale [HADS] | ||
| Alattas et al. [59] | Greater anxiety predicted a worse post-surgical outcome following knee replacement surgery, hence a validated screening tool for anxiety was recommended before surgery, and efforts to intervene should be forthcoming accordingly | ||
| Cho et al. [70] | No impact was noted of the effects of anxiety before total shoulder arthroplasty surgery for osteoarthritis as far as clinical outcomes are concerned, surgery improved psychological status as determined by the Hospital Anxiety and Depression Scale [HADS] | ||
| De Caro et al. [60] | Psychological factors and mental status in primary total hip + knee replacement cases can affect outcome + patient satisfaction. Strategies to identify and intervene accordingly are needed to improve outcomes of total joint replacement surgery | ||
| Dhurve et al. [54] | Patients with altered psychological profiles were less satisfied and functionally improved post-total knee arthroplasty surgery than those with normal profiles as measured by the Depression, Anxiety, and Stress Scale [DASS], Oxford Knee Score and goniometer- hence identifying and treating psychological distress as well as physical treatments may improve post-surgical satisfaction, as well as knee scores and range of motion | ||
| Ferreira et al. [40] | Women with knee osteoarthritis, mean age 67 years, have higher rates of anxiety as assessed using the State Trait Anxiety Inventory [STAI] when compared to control; in addition, they have a lower quality of life on the SF-36 survey instrument | ||
| French et al. [56] | Positive mental health predicted short term outcomes in hip osteoarthritis patients receiving exercise and manual therapy | ||
| Hanlandsmyth et al. [42] | Pre-surgical anxiety was related to pain intensity and distress in patients scheduled for total knee arthroplasty, thus the possibility of brief psychological interventions before surgery was discussed | ||
| Hanusch et al. [57] | Anxiety assessed by Hospital Anxiety and Depression Scale [HADS] questionnaire affected surgical outcomes of knee osteoarthritis cases, average age 71 years, negatively after undergoing total knee replacement in terms of worse knee function scores at 1 year, and should be taken into account when considering total knee replacement interventions | ||
| Helminen et al. [46] | Anxiety predicted pain and function at one year in knee osteoarthritis cases | ||
| Hassett et al. [47] | Presurgical affective symptoms not only have an effect on change in postsurgical pain, whereby lower preoperative scores on depression and anxiety were associated with lower postsurgical pain in patients undergoing lower extremity total joint arthroplasty surgery | ||
| Hiyama et al. [27] | Patients reported similar levels of anxiety regarding wounds, pain, gait, and falling at discharge after total knee arthroplasty. The severity of anxiety symptoms at discharge was negatively associated with the patient reported outcomes scores related to the Knee Society Score six-months postoperatively | ||
| Jones et al. [19] | Knee surgery cases are not impacted by pre-surgical anxiety | ||
| Khatib et al [60]. | Among patients eligible for knee arthroplasty surgery, the distressed group had significantly worse knee pain, knee function, and general quality-of-health scores. It was concluded that psychological health is an important often overlooked predictor of symptom severity and dysfunction in patients with knee arthritis and should be treated to help improve post-operative outcomes | ||
| Legha et al. [45] | Anxiety/depression predicted pain and function outcomes in people with knee osteoarthritis offered an exercise intervention | ||
| Liddle et al. [26] | Anxiety affected 8 year outcomes after unicompartmental knee replacement | ||
| Kohan et al. [55] | Anxiety impacts pain + function incrementally in glenohumeral osteoarthritis (p < .001) | ||
| O'Leary et al. [43] | Higher anxiety levels partially predicted worse outcomes in non surgical intervention applications for knee osteoarthritis, hence clinicians need to consider this issue when designing management strategies for this group | ||
| Sofat et al. [69] | A cross-sectional study of adults with mild and advanced knee osteoarthritis and healthy controls showed a multivariate analysis that indicated that body mass and the Hospital Anxiety and Depression Survey [HADS] scores were the most significant predictors of pain scores (p < 0.05) | ||
| Rasouli et al. [36] | Anxiety increases complications after total knee joint arthroplasty surgery | ||
| Rice et al. [62] | At 6 months after knee arthroplasty, a combination of preoperative pain intensity, expected pain, trait anxiety, and temporal summation was able to correctly classify 66% of patients into moderate to severe and no to mild persistent pain groups. At 12 months, preoperative pain intensity, expected pain, and trait anxiety correctly classified 66% of patients, implying a role for future intervention studies that aim to reduce the development of pain after surgery | ||
| Roger et al. [65] | Factors predicting discharge to rehabilitation after hip or knee arthroplasty surgery were older age, female gender, chronic obstructive pulmonary disease, anxiety-depressive disorder, and a history of stroke. Risk factors for 30-day readmission were male gender, obesity, and discharge to the rehabilitation unit | ||
| Shang et al. [58] | Long-term osteoarthritis, cardiovascular disease, and cancer were independent risk factors for incident depression and anxiety in both genders with osteoarthritis having the highest relative risk | ||
| Waimann et al. [64] | Anxiety leads to some degree to higher total knee replacement-related costs in patients with knee osteoarthritis. Preoperative interventions targeting these factors may reduce these costs and prove cost-effective | ||
Finally, while many proposed intervention approaches to counter anxiety prevail, along with an untested assumption that treating osteoarthritis cases presenting with anxiety using these may prove more helpful than not, regardless of anxiety subtype, very few actual well-designed and carefully controlled supportive studies exist.
There are also very few new facts about anxiety in the realm of osteoarthritis when compared to the focus anxiety clearly assumes in the realm of other chronic conditions, and almost no studies attempt to examine the interactive correlates of anxiety on various aspects of osteoarthritis disease using validated biomechanical, biochemical, and advanced serological and neurological assays, among others.
3.2. Research-Based Observations
As outlined previously by Stubbs et al. [5] as well as by Tan et al. [6], a sizeable number of patients with a diagnosis of osteoarthritis may be expected to exhibit various degrees of anxiety, ranging from moderate to severe. Of these cases however, Perez-Garcia et al. [7] found only 17 percent had been previously diagnosed, and only 5.8% were in therapy. Moreover, even though anxiety as a clinically relevant outcome indicator or mediator has been disputed in some cases [8, 9], those osteoarthritis cases suffering from anxiety alone, or anxiety and depression appear more likely than not to suffer from chronic or excessive chronic pain, among other negative disease correlates [10-12]. These negative anxiety-associated consequences include, but are not limited to, an increased risk for post-operative joint replacement surgical complications [13] in addition to pain [14, 15], plus heightened difficulties with activities of daily living and physical functioning [16, 17].
Barnett et al. [18] likewise found adults with joint pain reporting clinical anxiety, were not only quite numerous, in general, but were more likely than not to exhibit severe, rather than mild pain. It was further observed that the number of pain sites was also positively associated with the presence of clinical anxiety, and that those adults with symptoms of clinical anxiety appeared less likely to undertake general fitness exercises. They were also more likely to use walking aids and assistive devices, plus opioids than non-anxious adults with joint pain.
While generally poorly studied at the early disease stages, it appears that as the disease progresses and requires surgical intervention, almost 50 percent of preoperative osteoarthritis surgical cases may be expected to exhibit anxiety symptoms as observed by Jones et al. [19]. While this high number of anxious cases may have been attributable in part to the self-report mode of estimating anxiety as normal or abnormal, Wong et al. [20] as well as Castano et al. [21], Stubbs et al. [5] and Guglielmo et al. [22] all reported the presence of anxiety to be of the order of 20 percent or higher in various osteoarthritis or arthritis samples when this has been assessed. Moreover, anxiety rates observed among community-dwelling knee osteoarthritis clearly exceed those prevailing in the general population [23], and where present, these anxious osteoarthritis patients tend to have higher pain levels at rest as well as on initiating any activity when compared to non-anxious patients.
Bierke et al. [24] found trait anxiety, which is commonly indicative of an inherent anxiety state, to be present in approximately 14 percent of cases with disabling osteoarthritis awaiting treatment. Importantly, those identified as having a habitual pattern of anxiety behavior had higher mean dissatisfaction scores at 6 and 12 months post-surgery than those with no anxiety. Khan et al. [11] similarly found high levels of anxiety to prevail among osteoarthritis cases compared to non-osteoarthritis cases, especially among women.
More recently, Burston et al. [14] reported that osteoarthritis cases with high anxiety levels, independently from depression, exhibited lower pressure pain detection thresholds at sites local to and distant from the painful joint site. Separately, high anxiety scores predicted an increased risk of knee pain onset in 3274 originally pain-free individuals over the 1-year period (odds ratio = 1.71; 95% confidence interval = 1.25-2.34, p < 0.001). Similarly, this group found that rats used to uncover the mechanisms of anxiety in humans in a parallel experiment, developed significantly lower ipsilateral and contralateral hind paw withdrawal thresholds, compared with control rats (p = 0.0005), thus their clinical finding was mirrored by that obtained from an accepted model of painful osteoarthritis. Of additional import was the finding that the augmented pain phenotype that was observed was significantly associated with increased glial fibrillary acidic protein immunofluorescence in those brain regions associated with pain, thus implying that supraspinal astrocyte activation may serve as a significant determinant of underlying anxiety-augmented pain behavior that might be extremely helpful to explore in the future.
According to Harmelink et al. [25] and others such as Liddle et al. [26], even if anxiety rates are deemed acceptable or clinically unimportant, based upon the findings of Burston et al. [14] and others, it is hard to refute the fact that anxiety may accompany painful osteoarthritis, and that acknowledging the presence of any form of anxiety, if present, is very crucial not only in osteoarthritis remediation efforts, but also in primary, and secondary, as well as tertiary preventive efforts. In this regard, Hiyama et al. [27] found the median score for anxiety post knee surgery for the factors of wounds, pain, and gait of 4.0 to be quite substantive at discharge five days after surgery. The median score for anxiety about falling, a very important risk factor for complications post-surgery, was also 4.0. The level of anxiety regarding wounds, pain, gait, and falling was also associated in a negative manner with the knee function scores six-months postoperatively even after adjusting for all confounding factors. As well, the severity of the anxiety symptoms at discharge was negatively associated with physical function recovery six-months postoperatively.
As well as its negative impact on post-surgical reconstructive outcomes [28], unrelieved anxiety is expected to exacerbate harmful chronic oxidative stress levels and inflammatory responses that could impact healing [29]. Anxiety has been shown to raise the risk of premature mortality [30], in addition to explaining or mediating suboptimal post-operative physical improvements [31], especially in the short and medium post-operative periods [32]. The presence of anxiety is consistently found to heighten the risk of post-operative joint replacement surgical complications [33-36]. Anxious post-surgical osteoarthritis patients may also experience a lower subjective assessment of the possibility of returning to work during the lengthy post-operative rehabilitation period, plus a reduced degree of readiness to undergo treatment [37] in addition to a heightened risk of post-surgical complications [38, 39], poor life quality [40], sleep disruptions [41], excess pain [42], plus non-surgical multidisciplinary treatment outcomes [43].
Indeed, even where low anxiety rates prevail, anxiety appears to foster or mediate multiple negative osteoarthritis outcomes [44, 45]. Conversely, efforts to reduce prevailing anxiety severity, for example, among those requiring surgery for ameliorating their osteoarthritis disability, tend to yield better pain and functional outcomes than those not requiring any surgery [46, 47].
Unfortunately, despite these potentially relevant findings, as well as those published previously, results of recent community-based efforts to address and treat anxiety among osteoarthritis cases have not shown any degree of anticipated promise [48-50]. However, as pointed out by Hirakawa et al. [51], and others highlighted in Table 3, at a minimum, efforts to uncover and reduce persistent and oftentimes pervasive negative thoughts regarding future pain among osteoarthritis cases may yet help to minimize feelings of low self-efficacy and excess pain [48], plus lower than desirable satisfaction, and life quality [52], along with protracted recovery post-surgery, as well as excess post-operative pain [53-70]. To this end, and as implied by several authors cited in Table 3, the use of careful routine mental health assessments, as well as the application of appropriate follow-up interventions to minimize anxiety may yet prove helpful not only for attenuating or averting its oftentimes long-term negative effects in a fair proportion of disabled osteoarthritis patients, but for heightening overall health status, even if evidence is presently weak in this regard [33]. Moreover, even if anxiety is actually reduced by surgery, or does not have any long-term impact on recovery from joint replacement surgery [66, 67], identifying anxiety or its risk earlier, rather than later, as well as its correlates [68], is cited to be more likely than not to benefit a sizeable number of subjects with osteoarthritis, and inherent trait or chronic generalized anxiety disorders, as well as state anxiety, regardless of disease status. However, examining recommended interventions such as those advocated in Table 4 more closely must also be forthcoming to determine whether one or more of these approaches would be efficacious, and in what respect. Alternately, a fair percentage of patients may continue to experience excess pain and delayed surgical recovery [71], and contrary to findings of Cho et al. [70] may not improve as anticipated simply by undergoing joint replacement surgery alone if pre-surgical anxiety is not specifically treated or even identified as observed by Balik et al. [72].
| Patient driven | Provider driven | Other |
|---|---|---|
| ▪ Acceptance therapy ▪ Art therapy ▪ Dance therapy ▪ Exercise ▪ Guided Imagery ▪ Journaling ▪ Mindfulness meditation ▪ Music therapy ▪ Muscle specific training + exercise ▪ Nutrient optimization ▪ Positive effect journaling ▪ QiJong ▪ Spa therapy ▪ Stress control ▪ TaiChi ▪ Yoga |
▪ Cognitive behavioral therapy ▪ Comprehensive evaluation and follow up of needs ▪ Counseling ▪ Education ▪ Group therapy ▪ Holistic careful individualized treatment ▪ Massage ▪ Medication monitoring and usage of Occupational therapy ▪ Pain relief/control ▪ Pastoral care/religious support ▪ Pharmacologic therapy + effective pain medication ▪ Physical therapy ▪ Psychotherapy ▪ Relaxation therapy ▪ Self-efficacy training ▪ Skills training ▪ Sleep related interventions |
▪ Empathetic patient-centered approach ▪ Family and social support ▪ Resource support as indicated ▪ Target inflammation ▪ Target pain communication processes ▪ Yoga + education |
4. DISCUSSION
Osteoarthritis, a highly prevalent health condition remains a serious impediment to the well-being of many older adults who seek to remain independent and mobile. However, even though life quality is often impacted negatively and significantly by osteoarthritis [40], and may stem from physical as well as psychosocial issues among others, care often appears to remain suboptimal despite evidence that well-conceived primary care and community-based interventions can effectively reduce osteoarthritic pain and disability [49]. In this respect, the present review examined the current evidence base concerning the possible role of either preexisting or emergent anxiety or both in mediating, moderating, or exacerbating osteoarthritis disability, given its potential for prevention or remediation. It also sought to examine if more research, as well as routine screening and attention in this realm is warranted, and if so, in what way.
In this regard, results of the present data search that focused largely on published reports from 2014 to February 2020 showed that anxiety, deemed to be a state of emotional distress of varying degrees is generally a mental health correlate that has a negative impact on adults suffering from osteoarthritis, as outlined by Nur et al. [17], Wilke et al. [30], Zhang et al. [95], Zambon et al. [96], Mat et al. [97]. However, even when compelling new evidence shows how the extent of drug dependence is related to anxiety [99], and that mortality is heightened by anxiety [30], it is striking that when examined in the larger context of osteoarthritis as well as anxiety research that only a meager degree of research of acceptable quality on this issue prevails or is emerging. Indeed, in light of the fact that osteoarthritis is the most prevalent musculoskeletal disabler of older adults and that the disease has no known cure, or all encompassing remedial treatment approach is safe and effective, its widespread negative disease influence is bound to increase rather than decrease as society ages and years of life are extended if this correlate continues and its independent and interactive effects are largely ignored in the mainstream literature and primary care and surgical settings.
On the contrary, while assessing anxiety clinically is arguably very time consuming, and negated in importance by some [e.g8, 9, 19], it is very hard to refute any argument in favor of ignoring a possible highly salient role for anxiety in exacerbating osteoarthritis disability wherein routine clinical screening [42] followed by personalized carefully construed intervention if indicated, will prove more effective, as well as more cost-effective than not based on the overall weight of the evidence [see Table 3]. Kohan et al. [55], for example, found patients with glenohumeral osteoarthritis who had scores corresponding to a diagnosis of anxiety to experience lower functional and higher pain scores compared to those with scores in the normal range (p < .001). Analysis of variance showed progressively lower functional and higher pain scores as anxiety severity increased (p < .001).
It is also possible that a higher number of studies that are designed to include more diverse osteoarthritis cases, such as those with neck and back pain [98], will help to strengthen the case in favor of anxiety screening, as well as to provide new insights, and possibly to expand osteoarthritis treatment options and more desirable long-lasting treatment outcomes. Carefully controlling for age, gender, co-interventions disease manifestations, and disease prognosis in comparison studies, along with the use of advanced measurement technologies, and universally agreed upon anxiety measures, will also help to more clearly demonstrate support for or against anxiety screening among at-risk osteoarthritis patients. Alternately, examining whether those osteoarthritis cases functioning suboptimally despite treatment are suffering from some form of anxiety may prove highly revealing.
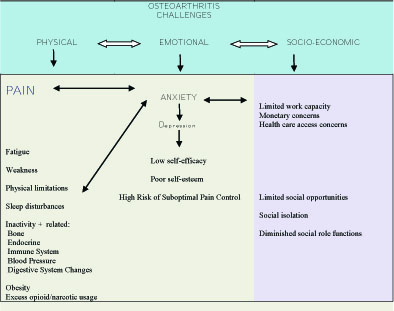
Indeed, as discussed by several authors, and as per Fig. (1), more work to tease out both the unique as well as the interactive effects of anxiety among cases with osteoarthritis with advanced technologies and in a prospective manner may greatly highlight the important interactive role played by cognitive factors in the disease cycle, even if these are currently ignored or overlooked more often than not. Such research is expected to reveal that the presence of anxiety is closely correlated with ensuing clinical outcomes, life quality, adherence to intervention recommendations and patient satisfaction.
In short, efforts to strengthen the current evidence base regarding the salience of anxiety in the context of the pathogenesis and treatment of osteoarthritis appears warranted. However, as outlined by Pan et al. [39] despite sufficient clinical as well as scientific rationale to more pro-actively, and comprehensively identify and treat prevailing modifiable mental health issue among cases suffering from osteoarthritis, not enough research or practice-based translation of the research prevails. As such, the immense personal and fiscal costs, plus the prevalence of anxiety and its adverse impacts are not only incalculable, but are more likely than not to continue to increase steadily each year, rather than decrease. Since this situation has enormous ramifications and implications not only for patients, but for families, employers, governments, and society as a whole-for example if we consider the opioid epidemic and its anxiety linkage, we strongly encourage osteoarthritis researchers and clinicians to keep anxiety in the forefront of their respective efforts.
CONCLUSION
Although the literature concerning the extent to which anxiety is a clinically relevant osteoarthritis determinant is very sparse with few robust studies when compared to the immense volume of literature on osteoarthritis and other independent topics shown in Table 1, it is concluded that there is a fairly strong case for considering anxiety as a contributor to disease burden, and that more extensive insightful careful scrutiny to address this possibility is not only warranted, but will be fruitful. In particular, further research to examine if the presence of anxiety is closely correlated with ensuing clinical outcomes, comorbid conditions, obesity, depression, central and peripheral pain sensitization, excess future disability, plus premature mortality is strongly indicated.
To further support this set of recommendations, efforts towards developing a clinically valid anxiety screening tool will be helpful in identifying those who may need psychological support. Researchers may also want to examine what would constitute best practices for the individual patient if anxiety is present, as there may be many diverse sources of anxiety among osteoarthritis cases, rather than any simple uniform manifestation. How to conduct a differential diagnosis in this respect and what degrees of anxiety are highly linked to suboptimal osteoarthritis outcomes also deserves attention. The possible use of a single modality that can be used at home to treat the physical as well as any anxiety correlate of osteoarthritis, such as QiGong versus the more passive approach of a provider-based intervention approach, or group therapy, should be explored as well.
In summary, psychological factors such as anxiety appear to be of significant importance in the context of efforts to comprehend and treat a substantive number of cases suffering from osteoarthritis disability, whether inherent, present as a generalized disorder, or a reactive state.
Indeed, while osteoarthritis is commonly considered a medical condition with distinct biological and biophysical attributes attributable to aging, rather than the presence of cognitive-associated attributes, anxiety in any form can clearly hamper the attainment of favorable osteoarthritis outcomes, including inflammation [99] and desired surgical outcomes [100]. As such, the societal burden attributable to the presence of untreated or unrecognized anxiety in fair numbers of osteoarthritis is inestimable, especially if this situation can be readily remediated early on in the disease process.
To this end, while it is encouraging to see a marked trend in the extent of research data in this field of thought as shown in Table 1, more research to examine the extent of, as well as the implications of anxiety in its various forms in the context of diverse stages of osteoarthritis and among a broad array of joints, not just the knee, or hip, is strongly urged. In addition, the application of a universally agreed upon valid and practical anxiety assessment method that can be used clinically for screening purposes is strongly indicated [101, 102], with a strong focus on a collaborative approach between patient and provider[s] in understanding the patient’s as well as the provider’s disease and outcome perspectives, along with appropriately tailored psychological interventions to minimize anxiety [103-105] and possible prolonged opioid usage [106] and other ill effect consequents [107].
As depicted in Fig. (1), and subject to further study, a thorough assessment of the whole patient (not just the anxiety), including comorbidities, the extent of anxiety plus other cognitive/emotional/behavioral characteristics, the social environment, and functional limitations of the patient is likely to help to foster more successful treatment outcomes [108]. In addition, sufficient research indicates that anxiety should be viewed as a probable potent osteoarthritis disease mediator or moderator, and one topic that warrants deserved attention clinically and empirically [17] to tease out possible clinically relevant behavioral versus neurobiological associations, and early indicators of a future pathogenic correlation [14, 31, 46, 59, 109-112], even if disputed or weakly supported by some [e.g9, 25, 66, 67, 70].
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None
CONFLICT OF INTEREST
The author declares that there is no conflict of interest regarding the publication of this article.
ACKNOWLEDGEMENTS
Not applicable.


