All published articles of this journal are available on ScienceDirect.
Median Nerve Schwannoma of the Hand and Wrist: 3 Cases
Abstract
Tumors of the median nerve are difficult to diagnose and median nerve schwannomas are rare. During a ten-year period, we treated eleven median nerve schwannomas found on the hand (nine) and wrist (two). All the tumors were treated by enucleation under loupe magnification and tourniquet application. All had a favorable result at a mean follow up of five years. We present three of our most typical cases, with schwannomas found on the wrist, palm and thumb. We also review the literature offering a wider view on the pathology, diagnosis and treatment of schwannomas in general.
1. INTRODUCTION
Peripheral Nerve Sheath Tumors (PNST) are uncommon, comprising less than 5% of the soft tissue tumors of the upper limb [1]. The most common amongst them are neurilemmomas, also known as Schwannomas, that are derived from Schwan cells and are more common in the hand and wrist [2] and neurofibromas, comprised of cells of mixed origin, that seem to be more common in the brachial plexus [3]. Schwannomas are usually solitary tumors arising from the Schwann cells that support the peripheral nerve fibers. Schwannomatosis comprises multiple non-cutaneous Schwannomas, but a very rare condition with 38 cases has been reported in the literature so far [4]. Schwannomas are benign in the vast majority of cases and malignant transformation or relapse post-excision is almost non-existent [5, 6]. They are usually asymptomatic in the early stages, and are not noticed, until they either become palpable, or develop nerve compression [7]. Computerized tomography and ultrasound were originally used as the main imaging modalities, yet recently, Magnetic resonance imaging has become the gold standard in imaging [8]. Treatment consists of intralesional excision by sparing the fascicles where possible, with predictable pain relief and low complication rate/recurrence [6].
Tumors of the median nerve are diagnostically challenging and median nerve schwannomas are rare. During a ten-year period, we treated eleven schwannomas of the median nerve found on the hand (nine) and wrist (two).
All the tumors were treated by enucleation under loupe magnification and tourniquet application. All had a favorable result at a mean follow up of five years. We present three of our most typical cases, with schwannomas located at the wrist, palm and thumb (Table 1).
2. MATERIALS AND METHODS: CASES
2.1. First Case
A 35-year-old male patient complained about a painful mass on his right wrist. His past medical history was clear. Three months prior, he had noticed a mass growing on the palmar surface of his wrist. The mass was small, palpable, immovable in the longitudinal but mobile in the perpendicular axis and it was soft. His chief complaint was his inability to keep up with his job as a guitar player. Upon examination, Tinel sign was positive, with otherwise normal sensory and motor function. MRI revealed a mass eccentric to his median nerve. The patient underwent tumor enucleation under general anesthesia and tourniquet. Loop magnification was used and all fascicles were salvaged. The patient had a difficult postoperative recovery and complained about paresthesias postoperatively, which eventually recovered at the 3 months follow up visit. Tinel’s was negative at the 6-month postoperative visit. (Figs. 1 and 2)
2.2. Second Case
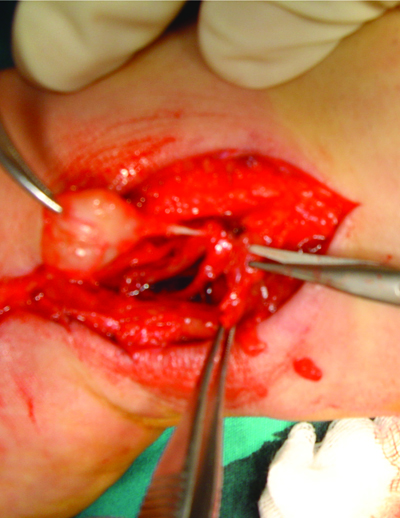
A female patient 60 years of age, presented with a painful palpable mass on her right hand. The mass had been growing for a year and was not mobile. The patient’s medical history was otherwise unremarkable. Tinel’s sign was present without sensory or motor loss. Upon MRI, a mass on the common digital nerve was evident and prominent. Under general anesthesia and tourniquet use, with loop magnification, the mass was surgically enucleated. There were no wound healing problems, or novel neurologic impairment. The patient complained about paresthesias which eventually disappeared at 6 months follow- up visit, along with her Tinel sign.(Fig. 3).
2.3. Third Case
An 80 year old female patient , with a painful mass on the left thumb that had been growing for the two years with no other symptoms. No Tinel’s sign was present, and there was no motor or sensory loss or limitation in thumb motion. The patient had a medical history of atrial fibrillation with a pacemaker and anticoagulant therapy. The patient could not undergo MRI due to her pacemaker. Under regional anesthesia and finger tourniquet, the tumor was enucleated. No wound healing problems or hematoma was observed postoperatively, however the patient complained of paresthesias till the 2 year postoperative visit. (Fig. 4).
At the final follow-up visit, there was no evidence of recurrence or novel neurologic symptoms. Histology was consistent with Neurilemoma in all three cases, and patients reported good pain relief.
3. DISCUSSION
Schwannomas, despite being the commonest of all PNST’s in the upper limb [2], are rare and consequently often misdiagnosed, or diagnosed postoperatively on the pathology examination. All major nerves of the upper limb can be affected with tumors of the ulnar, radial and median nerves being most commonly encountered, but Schwannomas have also been described affecting the axillary, musculocutaneous, posterior and anterior interossei and digital nerves [2, 6, 9, 10].
Neurilemmomas are usually solitary, benign tumors, however multifocal neurilemmomas [11] and multiple neurilemmomas on the same nerve have been described [12]. In the previous decade, Schwannomatosis was classified as a distinct clinical entity, with multiple non-cutaneous schwannomas in the absence of signs of neurofibromatosis type 2. It is, however, very rare, with only 38 cases reported so far according to a systematic review by Chick et al [4]. Despite their soft tissue origins, neurilemmomas have also been reported in intraosseous [13], subungual [14] and intramuscular [9] locations. In the largest published series, malignant Schwannomas were rare [5] and no malignant transformation was reported at mid-term follow up in a study of 234 benign solitary Schwannomas [9]. Ozdemir et al., in their series of 14 cases of median nerve Schwannomas reported no recurrence with a mean follow-up of 12 years [7].
Schwannomas tend to be asymptomatic in the beginning with nothing more than a palpable mass and an insidious onset of symptoms which are reflected in the long time intervals from the onset of symptoms to presentation seen in the largest series with Knight et al reporting a mean of 35 months [9] and Ozdemir et al reporting a mean of 25 months [7]. Acute onset of symptoms has been reported in a case of hemorrhaged Schwannoma [15, 16] but it is very rare. The main complaint is a palpable mass with Tinel’s sign being present in most patients (reported range 80-94%) [6, 7, 9]. The mass is usually mobile in an axis perpendicular to that of the affected nerve but not in a longitudinal direction. Spontaneous pain, altered sensation and muscle weakness have also been reported, but are not as common [7], and usually present later in the disease process, as the mass increases in size and causes compressive symptoms [17]. In our series, one patient presented early (3 months) with a chief complaint of a palpable mass on his dominant wrist which was probably noticed due to occupational reasons (guitar player). The other two patients presented more than one year after onset of symptoms.
Gadolinium enhanced MRI is useful in the diagnosis of Schwannomas, with the characteristic “target sign”, that is a biphasic or triphasic pattern, where the periphery has a higher intensity on the T2 sequence and low intensity on the Gadolinium enhanced T1 and vice versa on the central part. It was shown to have a specificity of 100% and a sensitivity of 59% in a histologically verified study by Koga et al [18]. Distinction between Schwannomas and Neurofibromas is not always easy and radiological signs suggest that the former is in an eccentric position in relation to the parent nerve and heterogenous appearance. Calcifications can be seen in chronic lesions, the so-called ancient Schwannomas [8].
Histological examination reveals a combination of areas with numerous Schwann cells, the Antoni A areas and areas that are relatively hypocellular, the Antoni B areas. Schwannomas tend to be encapsulated and eccentrically placed, thus allowing intralesional excision with fascicle preservation, whereas neurofibromas are usually non-encapsulated and centrally placed, thus hindering fascicle preservation during tumor excision. S-100 staining is strongly positive in Schwannomas which helps in differentiating it from NF [20].
In all cases, enucleation of the lesion under loop magnification should be attempted in an effort to preserve all fascicles [10], as was the case in all three of the patients. Pain relief has been shown to be a reproducible result in the vast majority of patients in the literature with rates exceeding 80%, with Tinel’s sign disappearing postoperatively [2, 3, 6]. Complications consist mainly of novel neurologic impairment and paresthesias have been reported with widely varying rates from 1.5-80% [9, 19]. The most common complication reported are paresthesias that seem to resolve over time [10]. Predictive factors for complications are age under 50 years and lesion size over 3 cm [18]. In our series, paresthesias were present in all our patients, but were resolved in the first postoperative year Table 1.



| Case | Age | Sex | Location | Time to Presentation | Chief Complaint | Tinel’s | Treatment | F/U | Complications/ Resolution |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 35 | M | Wrist | 3 months | Palpable mass/pain | Positive | Intralesional excision | 48 | Paresthesia/ 3 months |
| 2 | 60 | F | Hand | 14 months | Pain | Positive | Intralesional excision | 60 | Paresthesia/ 6 months |
| 3 | 80 | F | Thumb | 24 months | Pain | Negative | Intralesional excision | 72 | Paresthesia/ 12 moths |
CONCLUSION
Neurilemomas of the median nerve are rare, and can have an insidious onset of symptoms. A high index of suspicion and adequate imaging is necessary to ensure an adequate diagnosis. Enucleation of the tumor with fascicle preservation can yield predictably good outcomes with minimal recurrence rates.
ETHICS APPROVAL AND CONTENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
STANDARD FOR REPORTING
CARE guidelines have been followed.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


