All published articles of this journal are available on ScienceDirect.
The Acute Occult Salter-Harris Injuries in Children
EDITORIAL
Salter and Harris reported their five-part classification in children with open growth plates to grade fractures of the physeal plate according to the involvement of adjacent metaphysis and epiphysis. Their grading is the most commonly used classification for pediatric physeal fractures and is based on radiographic appearance, causal mechanism and prognosis, concerning the disturbance of growth [1-3].
Traditionally, the appearance of a fracture line on plain radiographs is needed for the primary diagnosis of a fracture. In the acute occult or obscure Salter-Harris injuries in children, there is no evidence of a fracture line at the initial anteroposterior and lateral radiographic survey. Occult undisplaced physeal fractures and specific bone bruises are the two subgroups of the acute occult Salter-Harris injuries in children. Such injuries should be clinically suspected, since they are always followed by a varying severity of tenderness, swelling, pain and refusal to use the injured extremity, and appropriately treated [4-10].
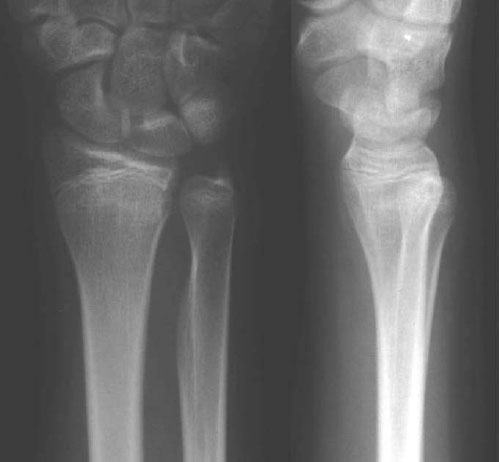
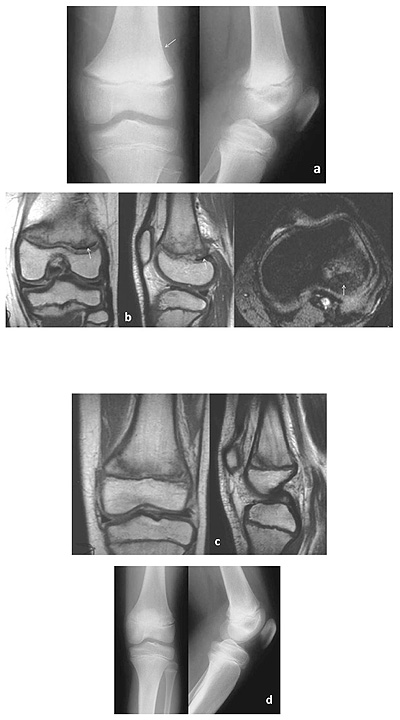
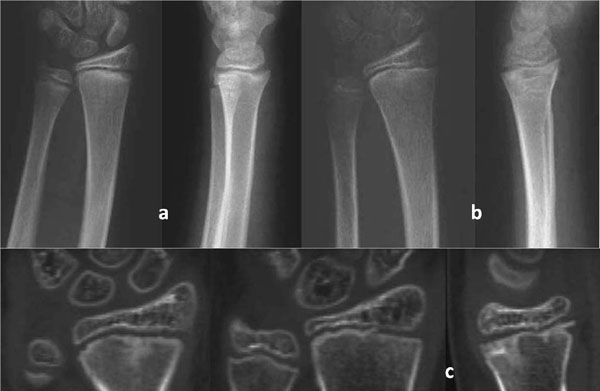
Radiographic diagnosis of the acute occult undisplaced Salter-Harris injuries of the extremities in children is usually secondary, referring to the findings that are consistent with the fracture healing process. These may include signs of periosteal healing and bone sclerosis, as well as the delayed appearance of a fracture line or a widened physeal plate [11-20]. There should be a clear distinction of these findings from the late radiographic signs of physeal injuries that are due to long-term complications, such as altered growth or premature closure of the growth plate, which are usually evident months or even years post-injury. The time of appearance of the radiographic signs of bone healing varies from a few days to 5 weeks, mainly depending on the age of the patient. Periosteal reaction is usually evident at 2 weeks after the injury. The subperiosteal new bone formation is due to the full thickness detachment of the periosteum from the metaphysis and diaphysis (Fig. 1). It is initially separable from the cortex but becomes incorporated in the cortex within a couple of months. Increased density due to the calcific callus formation is usually evident in the metaphyseal segment of the occult physeal injury (Fig. 2). It usually appears 4 to 5 weeks post-injury. The delayed appearance of a fracture line following a physeal injury usually involves the metaphyseal segment of the physeal injury. It is due to reabsorption involving an area of 1 to 2 mm of the bone at the metaphyseal fracture edges that have lost their blood supply. Bone reabsorption makes the metaphyseal fracture line become radiographically distinct, usually 2 to 5 weeks after the injury (Fig. 3). It may also occasionally involve the growth plate, appearing as physeal plate widening (Fig. 1). This radiographic finding should be clearly differentiated from the immediate post-traumatic widening of the physeal plate that is usually due to either a displaced fracture separation (slight widening) or soft tissue interposition (physeal gap of more than 3 mm) [21-23]. Therefore, it should be indicated that the secondary radiographic appearance of the widening of the growth plate may represent a healing sign of an unrecognized physeal plate injury [24, 25]. Physeal widening has also been diagnosed in the knees of high-level child athletes representing a sign of stress injury [26, 27]. It may also occasionally represent a significant predictor of subsequent growth disturbance [28].
Careful patient examination is particularly important in the acute occult undisplaced Salter-Harris injuries. Supplemental imaging, which usually includes oblique (tangential) projections, computerized tomography (CT) and magnetic resonance imaging (MRI), has been used to determine the precise fracture pattern in these injuries [29-32]. The detection of a fracture line on supplemental imaging indicates a subtle fracture. However, supplemental imaging rarely adds information that influences the treatment strategy of these fractures. Therefore, it is our standard policy not to perform other imaging studies, than the initial radiographic evaluation, in order to minimize the radiation dose and the imaging costs, and to treat all the injuries in children, in whom a potential fracture is clinically, but not radiographically, diagnosed with the appropriate immobilization.
The Salter and Harris classification scheme includes two acute injuries that may remain occult on conventional radiography in both the initial and follow-up evaluation. They are the undisplaced type I and the type V lesions.
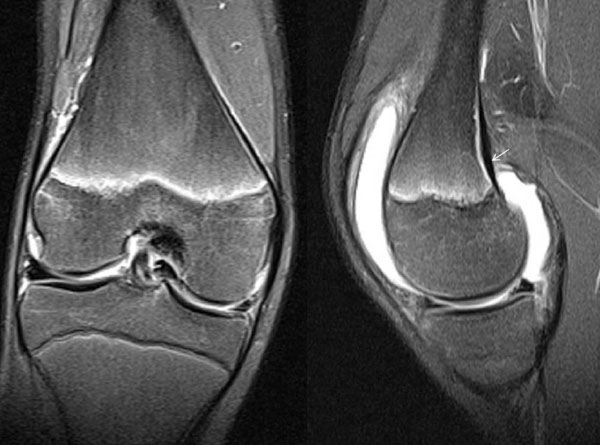
The Salter-Harris type I lesion represents a complete or incomplete fracture through the physeal plate without any bone fracture. It implies a shearing injury, although an avulsion or rotational injury cannot be excluded [1, 33]. When type I physeal injury occurs and the applied load is sufficient to disrupt the epiphyseal-metaphyseal unit, the periosteum may strip from the underlying bony cortex. This represents the earliest stages of physeal failure, preceding the failure of the continuity of perichondrium with the periosteum and displacement [5]. Radiographs are negative at the time of assessment in undisplaced injuries except for an associated soft tissue swelling. Stress radiographs to document displacement are generally unnecessary and probably unwise. The value of MRI was evaluated in a 9-year-old girl with a potential type I injury of the distal femur. The findings included widening of the physeal plate, perichondrial disruption, intracartilaginous fracture, and adjacent metaphyseal edema indicating a Salter-Harris type I fracture without displacement [34]. Other reports have described the MRI findings following soft tissue entrapment in displaced Salter-Harris type I injuries [35, 36]. It may be reasonable to consider that the nature of an undisplaced complete type I injury is most likely to be an initially minimally displaced lesion, in which the continuity of the perichondrium with the periosteum is preserved and the reduction is restored due to the elasticity of the perichondrium-periosteum complex. Therefore, it is mandatory to consider the MRI diagnosis of subperiosteal haematoma due to an even minor local metaphyseal detachment of the periosteum from the metaphyseal bone, as an initial absolute prerequisite for the diagnosis of an undisplaced complete type I growth plate injury (Fig. 4). Furthermore, it might be prudent to consider that a local minor disruption of the periosteum on the MRI findings can also be consistent with an undisplaced complete type I growth plate injury (Fig. 5). On the other hand, Salter-Harris type I incomplete physeal fractures may be associated with a pathological signal of the disrupted portion of the physeal plate but not with subperiosteal haematoma or a disrupted perichondrium-periosteum unit.
The pathology of an undisplaced Salter-Harris type II injury can be similar to that of a type I injury (Fig. 6). The roughly triangular variably-sized Thurston-Holland metaphyseal fragment is recognized as the hallmark of the Salter-Harris II injury [1, 37], while children with occult SH type II fractures of the distal femur that were evident on the MRI examination were all found to have posterior periosteal disruption and other soft tissue findings, thus indicating a hyperextension mechanism of injury [38].


Compared with radiography and CT, MRI is more expensive, but it is recommended in the literature because it provides a noninvasive means for the detection of the Salter-Harris acute occult fractures and may also alter the Salter-Harris staging [6, 29-31].
In addition, the diagnostic criteria were evaluated in the patients who were initially diagnosed with a complete undisplaced Salter-Harris type I lesion from the hospital database. In most of the cases, the diagnosis was based on the clinical findings. A small number of these patients were evaluated with a CT. In all of them, the diagnosis was changed to a Salter-Harris type II lesion due to the detection of a tiny or flake metaphyseal fragment that was attached to the epiphysis (Fig. 7). It was realized that the value of MRI to define a metaphyseal fragment becomes less with tiny or flake metaphyseal fragments. On the other hand, the value of CT to visualize tiny metaphyseal fragments is not limited. Therefore, it may be prudent to consider all the radiographically-diagnosed complete undisplaced Salter-Harris type I lesions as potential type II injuries until a CT scan proves the contrary, whenever the CT examination value is considered sufficiently reasonable.
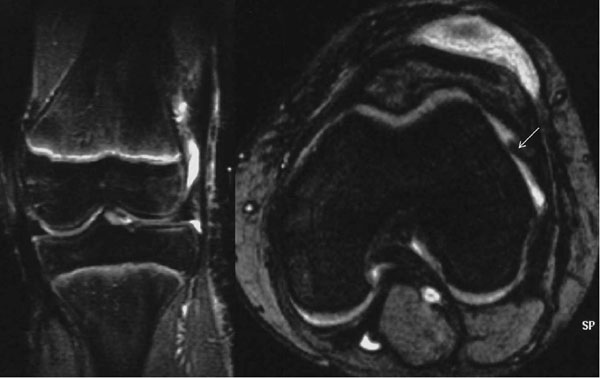
The Salter-Harris type V lesion represents a radiographically occult compression injury of the growth plate, following considerable axial load [39]. This should be differentiated from the crushing of physeal cells that may occur in any other type of Salter-Harris physeal fracture [40-47]. The definition that the type V injury is a longitudinal compressive force on the physis damaging only the physeal cells, but not a fracture since no trabeculae are broken [48, 49] has been questioned. This statement was not consistent with the description of type V injury given by Salter and Harris in their original article, who defined it as an injury resulting from a very severe crushing force applied through the epiphysis to an area of the epiphyseal plate [1]. The first inclusion criterion to diagnose a type V lesion, requiring normal findings on roentgenograms taken in at least two planes at the time of injury [49], should also be reevaluated. It would probably be prudent to change it to indicate no evidence of a fracture line to the physis, epiphysis or metaphysis. The two other inclusion criteria indicating that the patient has not received any form of manual treatment and that a retrospective diagnosis is made only after premature partial or complete growth arrest, secondary to physeal bridge formation, are absolute prerequisites to define a type V injury. The radiographic and/or CT appearance of impaction or diminution of the width of the physis associated with no evidence of a fracture line, as well as the persistence of significant pain at the level of the physeal plate following a period of immobilization, exceeding 5 to 6 weeks, for an occult physeal injury could be absolute indications to perform a MRI. The appearance of two significant bone contusions opposing one another on either side of the injured physeal plate, associated with local diminished width of the growth plate, has been considered to be pathognomonic of a Salter-Harris type V injury [50, 51]. The primary etiological factor of a type V lesion has been supposed to be ischemic damage rather than direct cellular compression in
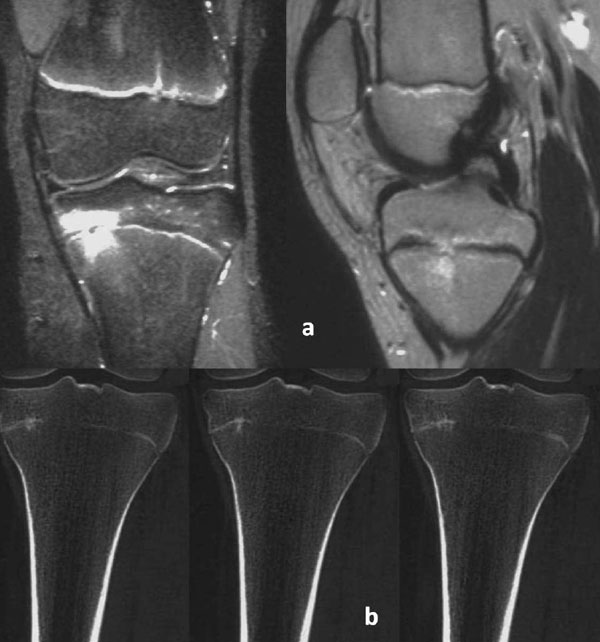
the germinal zone [49]. Histologic findings of the distal radius and ulna supported this concept suggesting that microscopic trauma may lead to microbridges in the form of transphyseal linear ossific striations, which may not necessarily lead to a complete arrest. However, they may interfere with growth leading to the well-recognized variations in the relative length of the distal radius and ulna [52]. In addition, growth disturbance is not encountered whenever the Salter-Harris type V injury occurs at the end of the growth (Fig. 8).
With the advent of fat-suppression techniques, a new category of injury has also been recognized on MRI. It refers to bone bruise or contusion, which usually involves a well-circumscribed area of cancellous bone. The nature of the high intra-osseous signal intensity on MRI using fat suppression is likely to represent focal edema and hemorrhage, following a microscopic trabecular injury and hemorrhage of bone marrow without disruption of adjacent cortices or articular cartilage [53-57].
The value of MRI was evaluated to diagnose non-radiographically evident injuries of the distal forearm and wrist, as well as of the ankle and foot, in children whose symptoms did not resolve after 5 to 6 weeks of immobilization. The MRI examination indicated the occult lesion of bone bruising in all the patients. It was suggested that the Salter-Harris type I complete undisplaced injuries were consistent with the MRI detection of bone bruising involving the metaphysis in close proximity to the distal radial growth plate, while bone bruises localized on both sides of the growth plate were considered as potential Salter-Harris type V injuries [58-60].
Finally, it may be prudent to extend the findings of this report to all the classification schemes for physeal injuries in children that have been reported in the literature, either before or after the Salter-Harris classification [61-71]. Our recommended mode of treatment for pediatric physeal injuries of the extremities when a fracture is clinically, but not radiographically, evident is splint immobilization to prevent displacement and allow fracture healing. The patient is reexamined clinically and radiologically once a week for a two-week period. In the cases that radiographic findings of bone healing are evident, as well as patients with no radiographic findings in the follow-up evaluation, but with persistent clinical symptoms, the immobilization period is prolonged for a sufficient period. In the latter, the period to resolve the clinical symptoms depends on the patient’s age. The period that is usually required for the clinical symptoms and signs to resolve following an acute occult physeal injury, which is more likely to be a Salter-Harris type II injury, varies between 4 weeks for the preschool ages to 5 weeks for older children. Children with persistent symptoms following a period of immobilization that would be sufficient for the healing of an acute physeal injury may suffer from bone bruising. The review of the related literature indicates that a limited MRI examination is useful and valuable in the detection of bone bruising in children with persistent symptoms following 5 to 6 weeks of immobilization.
CONCLUSION
In conclusion, the most challenging aspect of MRI-based diagnosis of the acute occult physeal injuries is the recognition of rare undisplaced complete Salter-Harris type I and type V injuries, as well as of bone bruising.
Traditionally, the appearance of a fracture line or signs of fracture healing on plain radiographs was needed to diagnose a fracture. Thus, children suffering from bone contusions might have been encouraged to use an injured extremity or to participate in sporting activities after an insufficient period of immobilization. An elongated immobilization and recovery period is the only required mode of treatment until complete resolution of the clinical symptoms and signs to prevent the subsequent development of insufficiency fractures. Bone bruising represents a distinct clinical entity with ‘benign’ characteristics since no long-term morbidity occurred in any of the reported patients. The single exception to this rule is the bone bruises which are associated with a Salter-Harris type V physeal injury in the growing skeleton.
CONFLICT OF INTEREST
The author certifies that he has no commercial associations (such as consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. The author received no financial support for this study.
ACKNOWLEDGEMENTS
Declared none.


