RESEARCH ARTICLE
Proximal Humerus Fractures in Children: Experience from a Central London Paediatric Orthopaedic Service
Woojin Chae1, *, Akib Khan2, Sarah Abbott3, Angelos Assiotis2
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 202
Last Page: 207
Publisher ID: TOORTHJ-13-202
DOI: 10.2174/1874325001913010202
Article History:
Received Date: 19/05/2019Revision Received Date: 27/08/2019
Acceptance Date: 20/09/2019
Electronic publication date: 15/11/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective:
Proximal humeral fractures are commonly observed in children who sustain falls whilst running, or from heights. Appropriate and correct treatment is key in order to avoid limb length discrepancy and functional deficiencies. Current treatment methods include non-operative management such as collar and cuff immobilisation, and operative methods such as elastic stable intramedullary nails or Kirschner wires. This paper aims to present the demographics of this patient population and our experience in managing patients with proximal humerus fractures in an urban tertiary referral centre.
Method:
We assessed 41 cases across two sites in central London, identified via hospital electronic notes and our radiology digital system. We analysed patient demographics, mechanism of injury, time to discharge from orthopaedic services taking into account radiological and clinical union, and the treatment methods utilised.
Results:
The mean age of the cohort was 8.6 years old. 70% of the injuries were due to falls and 85% of cases were treated without an operation. The mean time to discharge from our service following radiological and clinical union was 46 days (9 – 161 days). Mean radiological and clinical union were 21.8 and 36.2 days respectively.
Conclusion:
These results support a non-operative approach, especially in cases with patients under 10 years of age. Surgery should only be undertaken in patients who have severe displacement and who have failed attempts at closed reduction. We would advocate a similar approach in institutions dealing with a comparable population of patients, as long as there are provisions for referral of more complex cases that require surgical stabilisation.
1. INTRODUCTION
Proximal Humeral Fractures (PHF) are relatively uncommon amongst children and adolescents. They account for 3% of all fractures and contribute to 4-7% of all the physeal fractures in the child and adolescent age group [1-4]. Fractures involving the epiphysis are more likely to displace in comparison to metaphyseal PHF [5]. This anatomical area is important as 80% of longitudinal growth of the arm occurs at the physis of the proximal humerus; a fact that explains the great potential for remodelling in young children [6-8]. PHF are mostly seen in children experiencing frequent falls whilst running or from a height. Adolescents usually present such fractures after a sporting accident or direct trauma to the arm. The incidence of these fractures peaks between the ages of 10 and 14 [9]. Males are affected more often than females with prevalence in the non-dominant arm [5].
Undisplaced and minimally displaced PHF are managed non-operatively [5, 10, 11]. The non-operative approach involves placing the affected limb in a sling or collar and cuff with gradual physiotherapy-guided exercises. The management of fractures that are more displaced continues to be debated and the current literature proposes several different approaches [1, 10, 12-16]. Most centres advocate a surgical approach with techniques including closed reduction with internal fixation or Open Reduction with Internal Fixation (ORIF) [1, 10, 12-16]. Fixation is achieved with the use of Elastic Stable Intramedullary Nails (ESIN) or Kirschner wires (K wires) which can be buried or left exposed.
This paper aims to present the epidemiology of patients with PHF in a large tertiary referral centre for children’s orthopaedics in an urban area and the management principles employed in this centre.
2. METHODS
This is a retrospective case series from a tertiary paediatric hospital trust with two sites across Central London. We present all primary presentations of PHF between the 1st of June 2017 and 1st of June 2018 in patients under 16 years of age who were skeletally immature. We excluded skeletally mature patients, those who presented to other centres first, and those with incomplete or missing medical records (Table 1).
Patients were identified using hospital electronic notes on Evolve (Kainos, Dublin) and the in-house Picture Archiving and Communication (PACS) radiology system. Search terms were “shoulder” and “humerus”. All cases had formal radiologist reports confirming the presence of PHF. The electronic clinic letters were retrieved using the Evolve system for the patients who met the inclusion criteria. Data collected included demographics (age, gender, side of injury), mechanism of injury, date of discharge from orthopaedic services (due to either radiological union and/or satisfactory clinical progress) and treatment methods. Radiological union was defined as bridging callus at three out of four cortices on anteroposterior (AP) and lateral orthogonal radiographic views. Satisfactory clinical progress entailed a detailed clinical examination with fracture stability, adequate movement and no pain at fracture site. Angulation and displacement were calculated on the initial radiographs. Follow-up AP and lateral view radiographs were reviewed to determine the date of confirmed radiological union.
The data was tabulated and analysed. Statistics were calculated using RStudio 1.1.456 developed by RStudio Inc (Boston, Massachusetts) for both parametric data and non-parametric data.
| Inclusion and Exclusion Criteria | |
|---|---|
| Inclusion | Exclusion |
| - Under 16 years of age - Primary presentation to either hospital site - Included all types of Proximal Humeral Fracture regardless of mechanism of injury |
- Skeletally mature patients - Secondary presentations - Missing or incomplete records |
Ethical approval was sought and deemed unnecessary by the local hospital Research and Development panel.
3. RESULTS
The search terms initially returned 450 matches. Radiology reports were reviewed and 54 cases of PHF were identified. No cases were excluded due to skeletal maturity. One case was excluded due to the patient initially presenting to a different hospital several weeks prior to attending one of our centres for follow-up (as our hospitals were more conveniently for the patient to visit). There were 12 excluded cases due to missing clinic notes. The 41 remaining cases met the inclusion criteria specified in Table 1. See Appendix 1 for a full table of results.
3.1. Age and Gender
Data collection from the included patients showed that the mean age of children with PHF was 8.6 years old with 56% of these fractures occurring in females and 44% in males. The age of the cohort ranged from one month to 15 years old.
3.2. Mechanism of Injury
The most common cause of injury was falls (70%, n=29). There were two sports-related injuries (5%), both of which were in male patients. There was one fracture from a non-accidental injury (2.4%) and one suspected pathological fracture in a patient with global developmental delay and suspected disuse osteoporosis (2.4%). It should be noted that 20% of the cases did not have a recorded mechanism of injury.
3.3. Management
Choice of treatment was non-surgical in 85% of cases (n=35). These cases were managed in either a poly-sling or collar and cuff. Only one patient had an elastic stable intramedullary nail (2.4%) and two had an ORIF with K wire fixations (5%). There were three cases where fy the treatment method (7%) was not specified which were excluded from the analysis.
3.4. Time to Discharge
The overall mean time to the radiological union from the date of injury was 21.8 days with a range of nine to 78 days. The time to discharge due to satisfactory clinical assessment was a mean of 36.2 days from the date of injury ranging from five to 161 days. The earliest time to discharge was five days, at which time, the patient was clinically assessed and it was deemed appropriate to continue with non-operative management. The same patient who was from overseas subsequently travelled home after this assessment (Table 2).
| Mean Time to Discharge (days) | Mean Age | |
|---|---|---|
| Non-operative management | 45.51 | 8.21 |
| Operative management | 56.67 | 13.97 |
Non-operatively managed cases had a mean time to discharge of 45.51 days ranging from five to 161 days. The operatively managed cases had a longer mean discharge time of 56.67 days which ranged from 22 to 113 days.
4. DISCUSSION
The most common mechanism of injury in children is a backward fall onto an outstretched arm [17]. Adolescents usually present from sporting accidents, involving a direct impact to the arm or falls during sport [5, 9, 18-20]. Retrospective data from our orthopaedic centre supports other authors’ findings for the mechanism of injury. The demographics of our cohort showed a younger group of patients compared to other studies. This may be a result of a more densely-populated urban environment.
4.1. Anatomy and Biomechanics
The proximal humerus forms from three ossification centres. It is completely cartilaginous until four to six months of age when the primary ossification centre forms. The greater and lesser tuberosities form at three years and five years respectively, with the fusion of the nuclei at around seven years old. The growth plate of the humerus usually closes at 17 to 18 years of age [1, 16, 21].
The glenohumeral joint is encompassed in a joint capsule. The attachments of this capsule may help explain the Salter-Harris type II configuration of fractures of the proximal humerus in skeletally immature patients. Namely, the medial capsular structures extend from the glenoid and labrum superiorly onto the medial aspect of the metaphysis inferiorly. Additionally, the lateral capsular attachment to the anatomical neck of the humerus also exerts a potential force through the physis in trauma [5].
Structures that are closely related to the proximal humerus can complicate the treatment of the fracture. The axillary nerve wraps around the humeral neck and may be injured. As the tendon of the long head of biceps passes down along the bicipital groove, it may become incarcerated in the fracture site [7, 8, 11, 12, 19, 22]. An open approach may be necessary if surgical reduction of such fractures is attempted. The rotator cuff, pectoralis major and latissimus dorsi muscles act as distracting forces due to their insertions and direction of action [5, 22, 23].
Therefore, anatomical structures should be considered when reducing fractures and immobilising the arm, as this may affect the functional outcome and complicate the reduction of the fracture.
4.2. Treatment Protocol
Complications associated with PHF include a varus or valgus arm, a shortened arm and non-union. The goal of treating PHF is to restore the range of motion, full function, arm length and alleviate pain. Within our cohort, there was one incidence of complication during non-operative treatment. The patient had a subsequent fall after immobilisation which displaced the fracture, leading to a longer healing time. The patient was discharged from clinic 21 weeks following the subsequent injury with no report of pain, sensation change or functional deficits.
Although the techniques used in surgical intervention vary, there is a general consensus regarding the indications leading to operative management. These include an angulation of greater than 50 degrees in 10 year-olds or younger, 20 degrees or translation of greater than 50% in 11 year-olds or above, and failure of closed reduction of the fracture within the parameters mentioned above [1, 22, 24].
Most professionals agree that the three main factors which govern the decision to operate children with PHF are age, angulation and skeletal maturity of the patient [5, 7]. This has given rise to three distinct treatment groups within the paediatric population, namely patients of ages under 10, older than 13 and between 10 and 13.
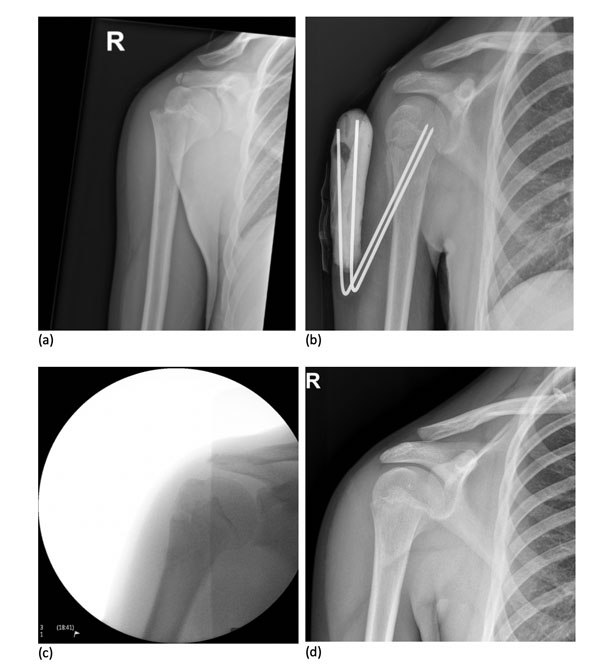
In the first group (under 10 years of age), a non-operative approach is preferable (see Fig. 1 for non-operative approach X-Rays). As seen in our case series, even a severely displaced fracture of 21mm of translation and 49 degrees of AP angulation was deemed acceptable and treated with a collar and cuff. The outcome was successful with the restoration of full limb function. Although satisfactory clinical progress took longer than the average in our cohort, the risk of undergoing unnecessary surgery was avoided.
 |
Fig. (1). X-Ray images showing the progression from injury (a) to 7 days after (b) a non-operative approach. |
The second group (greater than 13 years of age) are more skeletally mature. Naturally, the remodelling potential is less than in younger patients. Studies show that surgical intervention is more common in this group [4, 22] typically with successful outcomes and in certain cases, a worse outcome without surgery [6, 8, 19]. Reasons for this include the fact that older children usually present with high energy impact injuries potentially leading to extensively displaced and angulated fractures. More aggressive management may be needed to reduce and stabilise the fracture and encourage union.
Notably, there were only three surgically treated patients in our cohort, of which two had buried K wires and one patient underwent stabilisation with ESIN (Fig. 2). The preference of buried over-exposed K wires is due to the increased risk of infection due to exposed wires [5, 25]. Literature suggests that ESINs are used more frequently in severely displaced fractures and favoured over K wires due to their ability to allow earlier mobilisation post-operatively [1, 13]. However, the utilisation of ESIN requires extensive experience to yield a positive outcome. Therefore, many surgeons prefer to use K wires [1].
There remains debate regarding the optimal management of the third group (10 to 13 years of age). These patients may undergo both non-operative and operative treatment methods. This is because the biological age of the patient does not always truly reflect skeletal age and maturity. Therefore, more flexibility in management decisions is advisable [1, 5, 22]. In our cohort of 10 to 13 year-olds, the number of non-surgically treated patients was higher than surgically treated patients.
Non-operative treatment was favoured in this case series, in agreement with current literature. The remodelling potential of children is extraordinary, providing a basis for excellent outcomes without surgical intervention. However, as previously discussed, the decision to operate should include a consideration of age, fracture angulation and skeletal maturity.
4.3. Time to Discharge from Orthopaedic Services
The focus of this study was the time to discharge from orthopaedic services due to clinical union. In 73% (n=30) of cases, the discharge time and radiological/clinical union date were the same. In cases when the discharge date was later than the radiological/clinical union, this was due to subsequent injuries, or other fractures. The majority of patients in the cohort would be deemed to have achieved a radiological and clinical union on the same date due to the time intervals between outpatient appointments. Furthermore, with non-displaced fractures in younger children, a repeat radiograph was not carried out as it was clinically unnecessary and did not justify the radiation exposure.
5. LIMITATIONS
Limitations of this study include its retrospective nature. Furthermore, the lack of records and missing clinic letters contributed to the reduction of the included cohort size.
The sample size of the study was moderate for a one-year time period. However, it was not large enough to yield significant guidelines for the care of PHF. This study should be taken as a recommendation from the experience of a tertiary paediatric orthopaedic centre.
CONCLUSION
In conclusion, the reported findings of the case series advocate non-operative treatment where possible, especially in children younger than 10 years old. Surgical treatment should only be reserved for adolescents (10 years or older) with a fracture that is displaced and where closed reduction is not possible. The surgical technique is at the discretion of the operating surgeon.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
APPENDIX
| Gender | Age | Side | Mechanism of Injury | Radiological Union (d) | Clinical Union (d) | Last Follow-up (d) | Treatment |
|---|---|---|---|---|---|---|---|
| F | 13.58 | L | Fall | N/A | 30.00 | 30.00 | Collar and cuff |
| F | 12.42 | L | Fall | 9 | 16.00 | 44.00 | Collar and cuff |
| M | 13.42 | R | Sports | N/A | N/A | 5.00 | Collar and cuff |
| M | 5.50 | L | Fall | N/A | N/A | 3.00 | Collar and cuff |
| F | 9.42 | R | N/A | N/A | N/A | 5.00 | Polysling |
| F | 12.00 | L | N/A | 31 | 31.00 | 52.00 | Polysling |
| F | 6.67 | R | N/A | 9 | 9.00 | 9.00 | Polysling |
| F | 7.33 | L | Fall | 22 | 22.00 | 22.00 | Collar and cuff |
| M | 3.75 | L | Fall | 11 | 32.00 | 32.00 | Collar and cuff |
| F | 7.83 | R | N/A | 35 | N/A | N/A | Collar and cuff |
| F | 0.08 | L | NAI | N/A | 36.00 | 137.00 | Collar and cuff |
| F | 3.00 | R | Fall | 35 | 70.00 | 161.00 | Collar and cuff |
| M | 15.00 | L | Path | N/A | N/A | 48.00 | Collar and cuff |
| F | 3.42 | R | Fall | 7 | 21.00 | 21.00 | Collar and cuff |
| M | 9.08 | L | Fall | N/A | N/A | 4.00 | Polysling |
| F | 8.42 | L | Fall | 14 | 63.00 | 63.00 | U slab |
| M | 13.75 | R | Fall | 22 | 22.00 | 22.00 | ESIN |
| F | 9.50 | R | Fall | 24 | 24.00 | 24.00 | Collar and cuff |
| F | 4.58 | L | Fall | 5 | 26.00 | 152.00 | Collar and cuff |
| M | 10.75 | L | Fall | 19 | 19.00 | 41.00 | Collar and cuff |
| F | 6.50 | L | Fall | N/A | N/A | 9.00 | Polysling |
| M | 5.25 | L | Fall | 12 | 26.00 | 75.00 | Collar and cuff |
| M | 12.83 | L | Fall | 11 | 39.00 | 39.00 | Collar and cuff |
| M | 13.50 | L | Sports | 78 | 113.00 | 113.00 | K wires ORIF |
| M | 8.08 | L | N/A | 18 | 46.00 | 46.00 | Polysling |
| M | 14.67 | R | N/A | 29 | 35.00 | 35.00 | K-wire ORIF |
| F | 6.25 | L | Fall | N/A | 10.00 | 10.00 | Polysling |
| M | 13.00 | L | Fall | 27 | 62.00 | 62.00 | Collar and cuff |
| F | 6.92 | L | Fall | 38 | 38.00 | 38.00 | Collar and cuff |
| F | 10.58 | R | Fall | 16 | 16.00 | 16.00 | Collar and cuff |
| F | 11.08 | R | Fall | N/A | 49.00 | 49.00 | Collar and cuff |
| F | 7.33 | L | N/A | N/A | 29.00 | 29.00 | Collar and cuff |
| M | 4.17 | R | Fall | N/A | 58.00 | 58.00 | Collar and cuff |
| F | 9.17 | L | N/A | 12 | 54.00 | 124.00 | Collar and cuff |
| M | 5.58 | L | Fall | 16 | 30.00 | 30.00 | Collar and cuff |
| F | 8.58 | R | Fall | N/A | 36.00 | 36.00 | Collar and cuff |
| F | 2.25 | R | Fall | 9 | 23.00 | 23.00 | Collar and cuff |
| M | 8.92 | R | Fall | 26 | 39.00 | 39.00 | Collar and cuff |
| F | 6.25 | L | Fall | 22 | 50.00 | 50.00 | Collar and cuff |
| M | 13.17 | L | Fall | 31 | 31.00 | 31.00 | Collar and cuff |
| M | 9.83 | L | Fall | 25 | 25.00 | 67.00 | Polysling |