RESEARCH ARTICLE
Long-Term Outcomes after Colton Type I and II Fractures of the Olecranon
Thord von Schewelov1, Fredrik Hertervig1, Per-Olof Josefsson1, Jack Besjakov1, Ralph Hasserius1, *
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 208
Last Page: 216
Publisher ID: TOORTHJ-13-208
DOI: 10.2174/1874325001913010208
Article History:
Received Date: 09/06/2019Revision Received Date: 12/09/2019
Acceptance Date: 17/09/2019
Electronic publication date: 15/11/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
It is unclear if the outcomes differ in different subtypes of olecranon fractures.
Objective:
Evaluate the outcomes of different Colton types of olecranon fractures, and if outcomes differ in dominant and non-dominant arms and in men and women.
Methods:
We evaluated primary journals and radiographs in 40 men and 55 women with isolated olecranon fractures and classified fractures according to Colton. Mean 19 years after fracture event, we re-examined subjective, clinical and radiographic outcomes in the former patients, using the uninjured arms as controls.
Results:
89% of patients with Colton type I fractures reported at follow-up no subjective differences between the elbows, 84% with type II oblique/transverse fractures and 84% with type II comminuted fractures (p=0.91). The uninjured to former fractured arm differences in elbow range of motion and strength were no different in the 3 fracture types, the proportions of individuals with radiographic elbow degenerative changes were greater in type II than in type I factures (p<0.001), and there were no differences between the proportions of individuals with reduced joint space in the 3 groups (p=0.40). The outcomes were no different if the fractures had occurred in the dominant or non-dominant arms (p=0.43), or in men or women (p=0.43).
Conclusion:
There were no different outcomes after Colton type I, type II oblique/transverse or type II comminuted fractures, no different outcomes between fractures in dominant or non-dominant arms and no different outcomes in men and women.
1. INTRODUCTION
Olecranon fractures are estimated to occur with an incidence of 1.15 per 10,000 person-years [1-3]. This corresponds to approximately 10% of all upper extremity fractures [1-3]. The fractures may occur in different anatomic regions, after a direct trauma with the elbow flexed 60–110°, usually in the deepest part of the sigmoid notch, after a direct trauma with the elbow flexed more than 110°, usually in the olecranon process and after a direct trauma with the elbow extended usually distal to the coronoid process [3-6]. A sudden contraction of the triceps muscle, with the elbow in extension, may finally result in proximal avulsion fractures [3-6].
Even though outcomes after olecranon fractures are generally regarded as favourable [7, 8], fracture appearance and anatomic location may influence the outcomes. Comminuted fractures are more often associated with long-term disability and osteoarthritis than undisplaced fractures [2, 8, 9] and fractures that involve weight-loaded parts of articular surfaces are more commonly associated with post-traumatic osteoarthritis and disability than extra-articular fractures [1, 10]. Finally, fractures distal to the insertion of the triceps tendon are more exposed to displacing forces than fractures proximal to the insertion [3-6]. Studies ought, therefore, to evaluate outcomes after each subtype of olecranon fractures separately.
There are also concerns that outcomes after olecranon fractures may be affected by the choice of treatment. However, open reduction and internal fixation with figure-of-eight cerclage or tension band wiring technique have been reported with similar clinical outcome, indicating that several surgical techniques may lead to similar outcomes [8, 11]. Plate fixation is another surgical technique that has gradually gained popularity, but it is questioned whether this method improves the outcomes [12-14]. Recent reviews have, therefore, stated that because the quality of studies that evaluate the outcomes following different surgical techniques is poor, it is difficult to use them as a guide to decisions on how to treat olecranon fractures [7].
Most outcomes studies in patients with olecranon fractures have been short-term [13, 15-17], but there are few long-term studies [2, 18]. One such evaluated the outcomes of transverse displaced non-comminuted fractures a minimum 10 years after the injury, a study that found good or excellent patient-reported outcomes measures (PROM) with the outcomes being durable with time in most patients [18]. Similar inferences were put forward in a study that followed patients a minimum of 15 years [2]. There are, however, no long-term evaluations published that have followed specific subtypes of olecranon fractures. A recent review stated that this should be done, as the outcomes and the trend to develop posttraumatic osteoarthritis may differ between the subtypes [16].
The primary aim of this study was to evaluate the outcomes of different types of Colton fractures of the olecranon in a long-term perspective. The secondary aims were to evaluate whether there were different outcomes if the fractures had affected the dominant or non-dominant arms or occurred in men or women (Table 1).
2. MATERIALS AND METHODS
The Skane University Hospital, Malmo, Sweden, the only city hospital, served a city population of 264,937 in 1970. Virtually, all fracture patients in the city are treated at the emergency department in the hospital. All radiographs, referrals and reports are saved in the hospital archives, and have been so for the last century. This makes it possible to identify and reclassify old fractures. With the individual specific 10-digit Swedish personal number, which follows an individual from birth to death, it is further possible to identify former fracture patients for re-evaluation decades after the injury.
| - |
Type I (n = 19) |
Type II Transverse or Oblique Displaced (n = 57) |
Type II Comminuted (n = 19) |
|---|---|---|---|
| Age (years) | - | - | - |
| At injury | 24.9 ± 18.8 | 42.6 ± 20.4 | 40.4 ± 19.2 |
| At follow-up | 44.9 ± 18.3 | 61.1 ± 20.0 | 58.7 ± 18.2 |
| Follow-up period (years) | 20.0 ± 3.0 | 18.5 ± 3.0 | 18.3 ± 2.8 |
| Gender (n [%]) | - | - | - |
| Men | 9 (47%) | 20 (35%) | 11 (58%) |
| Women | 10 (53%) | 37 65%) | 8 (42%) |
| Trauma type (n [%]) | - | - | - |
| Low energy | 13 (68%) | 33 (61%) | 7 (37%) |
| High energy | 6 (32%) | 21 (39%) | 12 (63%) |
| Anatomic location (n [%]) | - | - | - |
| Proximal third of olecranon | 6 (31%) | 10 (18%) | 4 (21%) |
| Mid third of olecranon | 9 (47%) | 35 (61%) | 11 (58%) |
| Distal third of olecranon | 4 (21%) | 12 (21%) | 4 (21%) |
| Side | - | - | - |
| Right | 6 (32%) | 30 (53%) | 9 (47%) |
| Left | 13 (68%) | 27 (47%) | 10 (53%) |
| Primary treatment (n [%]) | - | - | - |
| Instant mobilisation | 6 (32%) | 0 | 0 |
| Plaster | 11 (58%) | 6 (11%) | 1 (5%) |
| Open reduction and internal fixation | 2 (10%) | 51 (89%) | 18 (95%) |
| Current workload (n [%]) | - | - | - |
| White collar | 9 (64%) | 19 (36%) | 9 (50%) |
| Blue collar | 1 (7%) | 4 (7%) | 3 (17%) |
| Retired | 4 (29%) | 31 (57%) | 6 (33%) |
In this retrospective case-control study, we re-evaluated all radiographs in patients treated at the hospital with elbow fractures between 1969 and 1979. We identified 2965 patients with elbow fractures, of whom 315 had isolated fractures of the olecranon. At follow-up, 216 of these patients had died or relocated out of the region. The 99 remaining former fracture patients were invited to our study (Fig. 1). Forty men and 55 women (attendance rate 96%) with a mean age of 38.6 years (range 5-77) at injury answered a questionnaire a mean 18.8 years (range 15.0-25.0) after the fracture event. Seventy-seven former patients (36 men, 41 women) with a mean age 37.8 years (range 5-70) at injury also attended a clinical exam a mean 18.8 years (range 15.0-25.0) after the fracture event and 80 former patients (36 men, 44 women) with a mean age of 38.1 years (range 5-70) at injury also attended a radiographic exam a mean 18.9 years (range 15.0-25.0) after the fracture event (Fig. 1).
In the 92 patients for whom we had data on type of trauma, we found that 53 patients (19 men, 34 women) had sustained a low-energy trauma (defined as a blow to the elbow or falling from standing height or less) and 39 (20 men, 19 women) a high-energy trauma (defined as a fall from higher than 2 metres or being involved in a motor vehicle accident). The right elbows were fractured in 45 (47%) and the left in 50 (53%) patients. In the 76 patients for whom we had data on arm dominance, we found that 37 (49%) had sustained fractures in the dominant and 39 (51%) in the non-dominant arm.
Six patients had been treated at injury with direct mobilization, 18 patients with immobilization in plaster for a mean 4.3 weeks (range 1.5-8.0 weeks), 34 with open reduction and internal fixation with figure-of-eight cerclage, 32 with open reduction and internal fixation with tension band wiring technique and 5 with other surgical techniques. After the operation, all surgically treated patients were immobilized in plaster, for a mean period of 4.4 weeks (range 0.1-7.0). Seventeen patients postoperatively had a remaining radiographic articular diastasis of more than 2 millimetres (mm) and 6 more than 3 mm. After the fracture had healed, 41/71 operated patients had a second operation, in all cases including removal of the osteosynthesis.
 |
Fig. (1). Flow-chart describing participants. |
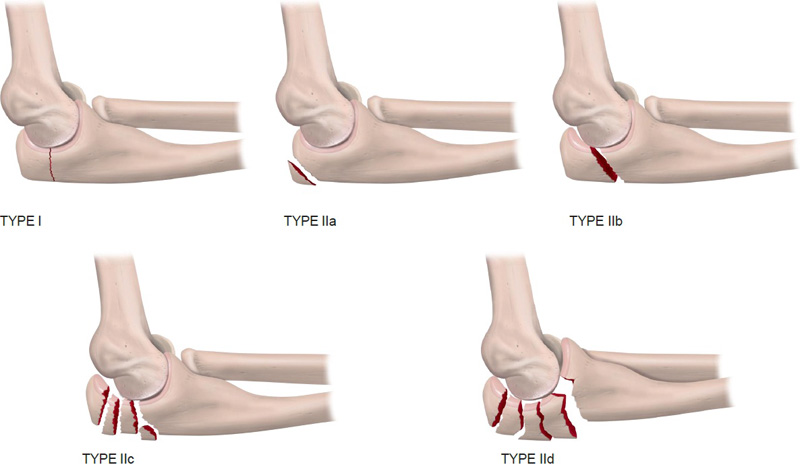 |
Fig. (2). Colton type I and II fractures of the olecranon. |
The 95 included patients answered a questionnaire that evaluated the subjective outcomes, where the former fractured and uninjured arms were compared with respect to pain at rest, pain on loading, instability, strength and whether there were any differences between the elbows.
The 77 patients who attended the clinical re-evaluation had both arms examined by two consultants in orthopaedics who were uninvolved in and unaware of the treatment of the patients. Arm circumferences were measured 10 centimetres (cm) above and below the tip of the olecranon with a measuring tape. Elbow flexion and extension, wrist flexion and extension, forearm pronation and supination and elbow valgus/varus angle in extension were measured with a goniometer. Grip strengths were measured with a Martin vigorimeter (Heinrich C. Ulrich, Werkstätten für Medizinmechanik®, Ulm-Donau, Germany).
Primary radiographs were classified according to Colton [19]. Colton type I factures include fractures that are displaced less than 2 millimetres (mm), also with the elbow in 90° flexion or with the elbow extended against gravity. Type II fractures include fractures that are displaced more than 2 mm, then further subtyped into (a) avulsion fractures, (b) oblique or transverse fractures, (c) comminuted fractures and (d) fracture-dislocations (Fig. 2) [19]. Since our study only identified patients with isolated articular olecranon fractures, no Colton type II a and type II d fractures were included. Furthermore, since no structural clinical exams were conducted at fracture event, we could not be sure that the type I fractures at injury had a remaining displacement at 90° in elbow flexion or in extension against gravity. We must, therefore, regard our classification as being a modified Colton type I classification. With this definition, we found 19 type I fractures, 57 type II transverse or oblique fractures (type II b) and 19 type II comminuted fractures (type II c).
The 80 patients who attended the radiographic re-evaluation had both elbows and both forearms evaluated by anteroposterior and lateral projections. All radiographs were reviewed by one radiologist, uninvolved in and unaware of the treatment, type of fracture and outcome. Degenerative changes were defined as having at least one of the following signs: subchondral sclerosis, subchondral cysts, osteophytes or joint space narrowing greater than 1 mm compared to the uninjured elbow. We defined joint space narrowing above 1 mm as a radiographic sign of osteoarthritis.
Data are presented as numbers, proportions (%), mean ± standard deviations (SD), mean with ranges and mean with 95% confidence intervals (95% CI). Group comparisons are done with Fisher’s exact test, Chi-squared test, paired Student’s t-test, unpaired Student’s t-test and analyses of variance (ANOVA). A p < 0.05 is regarded as a statistically significant difference.
3. RESULTS
There were no statistically significant differences in subjective outcomes when comparing Colton type I, Colton type II oblique /transverse or Colton type II comminuted fractures (p=0.91). A majority of patients within all 3 types of fracture reported favourable outcomes (Table 2). The only objective impairments were reduced grip strength in the former fractured arms in patients with type I fractures, and deficit in extension in the former fractured elbows in patients with type II oblique/transverse fractures (Table 3). There were no statistically significant uninjured to former fractured arm differences between the 3 types of Colton fractures (Table 3). Three individuals had a deficit in the range of motion (ROM) that exceeded 25°, two with type II oblique or transverse fractures and 1 with a type II comminuted fracture. These 3 patients reported a markedly inferior subjective function in the former fractured elbows.
| - |
Type I (n = 19) |
Type II Transverse or Oblique (n = 57) |
Type II Comminuted (n = 19) |
p-value |
|---|---|---|---|---|
| Elbow pain at rest | - | - | - | - |
| Yes | 0 | 3 (5%) | 1 (5%) | 0.59 |
| No | 19 (100%) | 54 (95%) | 18 (95%) | |
| Elbow pain at load | - | - | - | - |
| Yes | 1 (5%) | 8 (14%) | 1 (5%) | 0.40 |
| No | 18 (95%) | 48 (86%) | 18 (95%) | |
| Elbow instability | - | - | - | - |
| Yes | 0 | 1 (2%) | 0 | 0.71 |
| No | 19 (100%) | 55 (98%) | 19 (100%) | |
| Elbow weakness | - | - | - | - |
| Yes | 0 | 5 (9%) | 3 (16%) | 0.21 |
| No | 19 (100%) | 52 (91%) | 16 (84%) | |
| Status compared to uninjured elbow | - | - | - | - |
| No difference | 17 (89%) | 48 (84%) | 16 (84%) | 0.91 |
| Slightly inferior | 2 (11%) | 7 (12%) | 2 (11%) | |
| Markedly inferior | 0 | 2 (4%) | 1 (5%) |
| - | Type I (n =14) | Type II Transverse or Oblique (n = 46) | Type II Comminuted (n = 17) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| - | Fractured Arm | Uninjured Arm | Uninjured to Fractured Arm Difference | Fractured Arm | Uninjured Arm | Uninjured to Fractured Arm Difference | Fractured Arm | Uninjured Arm | Uninjured to Fractured Arm Difference |
| Elbow flexion (degrees) | 144±6 | 144±6 | 0 (0.0, 0.0) | 140±10 | 143±6 | 3 (–0.0, 5.2) | 137±7 | 138±6 | 1 (–1.2, 3.0) |
| Elbow extension (degrees) | 2±5 | 0±10 | –2 (–5.6, 2.1) | –5±10 | –2±7 | 4 (1.2, 6.3) | –6±11 | –1±4 | 6 (0.4, 10.8) |
| Forearm pronation (degrees) | 85±7 | 86±7 | 1 (-0.8, 2.2) | 84±11 | 85±7 | 1 (–1.3, 3.9) | 83±11 | 83±12 | –1 (–1.8, 0.7) |
| Forearm supination (degrees) | 83±20 | 84±17 | 1 (–0.8, 2.2) | 85±9 | 86±5 | 2(±0.9, 3.9) | 85±9 | 85±8 | 0 (–0.3, 0.9) |
| Elbow valgus angle (degrees) | 5±6 | 7±9 | 1 (–1.7, 4.5) | 10±6 | 8±4 | –1 (–2.7, –0.2) | 7±4 | 6±4 | –1 (–3.1, 0.6) |
| Wrist flexion (degrees) | 71±14 | 74±9 | 3 (-1.8, 8.2) | 66±14 | 67±12 | 1 (±1.5, 3.1) | 67±10 | 67±10 | –1 (–2.4, 1.2) |
| Wrist extension (degrees) | 66±9 | 67±9 | 1 (–0.3, 1.8) | 62±14 | 61±12 | –1 (–2.3, 1.1) | 63±12 | 63±13 | 1 (–4.7, 6.0) |
| Circumference upper arm (cm) | 25.7±3.0 | 25.9±3.1 | 0.2 (–0.0, 0.4) | 27.1±2.9 | 27.1±2.9 | 0.0 (–0.2, 0.2) | 28.2±2.8 | 28.2±2.6 | 0.0 (–0.4, 0.4) |
| Circumference forearm (cm) | 24.3±2.2 | 24.3±1.9 | 0.1 (–0.3, 0.5) | 24.7±3.1 | 24.6±3.1 | 0.0 (–0.2, 0.1) | 25.5±3.3 | 25.5±3.1 | 0.0 (–0.6, 0.5) |
| Grip strength (kp/cm2) | 0.77±0.39 | 0.84±0.39 | 0.06 (0.01, 0.12) | 0.77±0.39 | 0.84±0.39 | –0.00 (–0.03, 0.03) | 0.86±0.31 | 0.87±0.27 | 0.01 (–0.06, 0.10) |
| - | Type I (n =15) | Type II Transverse or Oblique (n =48) | Type II Comminuted (n =17) | Comparison Fractured Elbows | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| - | Fractured Elbow | Uninjured Elbow | p-value | Fractured Elbow | Uninjured Elbow | p-value | Fractured Elbow | Uninjured Elbow | p-value | p-value | |||||||
| Osteophytes | - | - | - | - | - | - | - | - | - | - | |||||||
| Yes | 2 (13%) | 1 (7%) | 0.58 | 18 (38%) | 4 (9%) | 0.001 | 7 (41%) | 0 | 0.003 | 0.17 | |||||||
| No | 13 (87%) | 13 (93%) | 30 (62%) | 42 (91%) | 10 (59%) | 17 (100%) | |||||||||||
| Cysts | - | - | - | - | - | - | - | - | - | - | |||||||
| Yes | 1 (7%) | 0 | 0.33 | 19 (40%) | 1 (2%) | <0.001 | 7 (41%) | 0 | 0.003 | 0.04 | |||||||
| No | 14 (93%) | 14 (100%) | 29 (60%) | 45 (98%) | 10 (59%) | 17 (100%) | |||||||||||
| Subchondral sclerosis | - | - | - | - | - | - | - | - | - | - | |||||||
| Yes | 5 (33%) | 1 (7%) | 0.08 | 40 (83%) | 5 (11%) | <0.001 | 16 (94%) | 3 (18%) | <0.001 | <0.001 | |||||||
| No | 10 (67%) | 13 (93%) | 8 (17%) | 41 (89%) | 1 (6%) | 14 (82%) | |||||||||||
| Reduced joint space | - | - | - | - | - | - | - | - | - | - | |||||||
| Yes | 2 (14%) | 0 | 0.14 | 2 (4%) | 1 (2%) | 0.56 | 1 (6%) | 0 | 0.31 | 0.40 | |||||||
| No | 12 (86%) | 14 (100%) | 45 (96%) | 46 (98%) | 16 (94%) | 17 (100%) | |||||||||||
| Any degenerative changes | - | - | - | - | - | - | - | - | - | - | |||||||
| Yes | 5 (33%) | 1 (7%) | 0.08 | 42 (88%) | 5 (10%) | <0.001 | 17 (100%) | 3 (18%) | <0.001 | <0.001 | |||||||
| No | 10 (67%) | 13 (93%) | 6 (12%) | 43 (90%) | 0 | 14 (82%) | |||||||||||
| - | Arm Dominance | Gender | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| - | Fracture in Dominant Arm (n=37) | Fracture in Non-dominant Arm (n=39) | p-value |
Fracture in Men (n=40) |
Fracture in Women (n=55) |
p-value | |||||||
| Elbow pain at rest | - | - | - | - | - | - | |||||||
| Yes | 2 (5%) | 2 (5%) | 0.96 | 3 (8%) | 1 (2%) | 0.17 | |||||||
| No | 35 (95%) | 37 (95%) | 37 (92%) | 54 (98%) | |||||||||
| Elbow pain at load | - | - | - | - | - | - | |||||||
| Yes | 5 (14%) | 5 (13%) | 0.96 | 5 (12%) | 5 (9%) | 0.61 | |||||||
| No | 32 (86%) | 33 (87%) | 35 (88%) | 49 (91%) | |||||||||
| Elbow instability | - | - | - | - | - | - | |||||||
| Yes | 1 (3%) | 0 | 0.31 | 0 | 1 (2%) | 0..40 | |||||||
| No | 36 (97%) | 38 (100%) | 39 (100%) | 54 (98%) | |||||||||
| Elbow weakness | - | - | - | - | - | - | |||||||
| Yes | 5 (14%) | 3 (8%) | 0.41 | 5 (12%) | 3 (5%) | 0.22 | |||||||
| No | 32 (86%) | 36 (92%) | 35 (88%) | 52 (95%) | |||||||||
| Status compared to uninjured elbow | - | - | - | - | - | - | |||||||
| No difference | 28 (76%) | 34 (87%) | 0.43 | 32 (80%) | 49 (89%) | 0.43 | |||||||
| Slightly inferior | 7 (19%) | 4 (10%) | 6 (15%) | 5 (9%) | |||||||||
| Markedly inferior | 2 (5%) | 1 (3%) | 2 (5%) | 1 (2%) | |||||||||
| - | Arm Dominance | Gender | ||
|---|---|---|---|---|
| - | Uninjured to Fractured Arm Difference when Fracture was Sustained in Dominant Arm (n=37) | Uninjured to Fractured Arm Difference When Fracture Was Sustained in Non-Dominant Arm (n=39) |
Uninjured to Fractured Arm Difference When Fracture was Sustained in Men (n=36) |
Uninjured to Fractured Arm Difference when Fracture was Sustained in Women (n=41) |
| Elbow flexion (degrees) | 3 (–0.7, 5.8) | 1 (–0.0, 2.0) | 3 (–0.2, 6.6) | 0 (–0.2, 1.2) |
| Elbow extension (degrees) | 4 (1.7, 7.3) | 2 (–1.0, 5.1) | 3 (–0.4, 6.3) | 3 (0.9, 5.9) |
| Forearm pronation (degrees) | 2 (–1.3, 4.8) | 0 (–1.3, 1.1) | 2 (–1.4, 5.0) | 0 (–1.0, 0.8) |
| Forearm supination (degrees) | 2 (–0.7, 5.0) | 0 (–1.0, 1.2) | 1 (–0.1, 5.0) | 1 (–1.2, 4.1) |
| Elbow valgus angle (degrees) | –2 (–3.2, –0.3) | 0 (–1.4, 1.4) | 0 (–2.1, 1.3) | –1 (–2.5, 0.0) |
| Wrist flexion (degrees) | 0 (–1.0, 1.6) | 2 (–1.5, 4.6) | 2 (–1.3, 4.6) | 0 (–1.5, 2–0) |
| Wrist extension (degrees) | 0 (–1.4, 2.0) | 0 (–2.9, 2.1) | 1 (–1.3, 4.6) | –1 (–3.0, 1.5) |
| Circumference upper arm (cm) | –0.1 (–0.2, 0.1) | 0.1 (–0.1, 0.3) | 0.1 (–0.1, 0.3) | 0.0 (–0.2, 0.2) |
| Circumference forearm (cm) | –0.3 (–0.5, –0.1) | 0.3 (0.1, 0.5) | 0.0 (–0.3, 0.2) | 0.0 (–0.2, 0.2) |
| Grip strength (kp/cm2) | 0.01 (–0.02, 0.05) | 0.00 (–1.4, 1.4) | 0.02 (–0.02, 0.06) | 0.01 (–0.02, 0.05) |
Type II oblique/transverse and Type II comminuted fracture were associated with radiographic degenerative changes, both when former fractured elbows within the same individuals were compared with the uninjured elbows, and when elbows with former type II fractures were compared with elbows with former type I factures (Table 4). There were no differences between the proportions of individuals with a radiographic elbow joint space reduction between the 3 types of Colton fractures (Table 4).
There were no statistically significant subjective differences in elbow function between patients with fractures in the dominant or non-dominant arms (p=0.43) or when comparing men and women (p=0.43) (Table 5). The only objective consistent uninjured to former fractured arm differences were greater forearm circumferences in the dominant arms, irrespective of whether the fractures had occurred in the dominant or non-dominant arms (Table 6). There were no differences in uninjured to former fractured arm differences when comparing men and women (Table 6).
4. DISCUSSION
The long-term outcomes of isolated Colton type I, type II oblique/transverse and type II comminuted fractures of the olecranon are favourable, without subjective or objective statistically significant differences in the long-term outcomes between the 3 types. Only 3% of the included individuals rated their former fractured elbows markedly inferior compared to the uninjured, and only 4% had ROM deficits exceeding 25 degrees. We found further no differences when comparing fractures in dominant or non-dominant arms or in men or women. The results in this study also confirm the daily clinical impressions that posttraumatic degenerative changes of elbows are well tolerated.
Virtually all studies that evaluate olecranon fractures do not separate the outcomes within each specific subtype [7, 8]. Horne et al. when including all types of olecranon fractures, reported good clinical outcomes in 100 patients a mean 2.5 years after the fracture event [20]. Our research group has reported good or excellent outcomes in 85% of the patients, with the outcomes not being affected by the choice of surgical technique or hardware removal [7, 8]. Other reports have concluded that the outcomes are superior in fractures of the proximal or middle 1/3 of the trochlear notch [20] and that there are lower risks of developing osteoarthritis in undisplaced fractures and fractures without joint diastasis than in comminuted fractures and fractures with remaining articular diastasis [2, 8, 9]. Our study provides more detailed information, reporting that the subjective and objective outcomes are no different when comparing Colton type I, type II oblique/transverse and type II comminuted fractures.
Most studies infer that minor objective deficits in elbow ROM are of no clinical relevance. Holdsworth et al. reported in 52 patients with olecranon fractures, 2 years after surgery with tension band wiring technique, good or excellent outcome in 85% of the patients, although in 1/3 of the patients, there was a 10 to 30° extension deficit and in 6% deficits greater than 30° [21]. Eriksson et al. reported in 85 patients that 6 years after olecranon fractures, there was a severe disability in only 3% of the patients, although one third had elbow ROM deficits greater than 20° [22]. Good or excellent outcomes have also been reported in 95% of the patients with olecranon fractures 14 months after the fractures were treated with open reduction and fixation with tension band wiring technique [23] and in 93% after 16 months [24], in spite of a high proportion of patients with impaired elbow ROM. The researchers, therefore, concluded that as long as the patient could reach the face, reduction in elbow ROM is of minor clinical relevance [20]. Our data support this view, as most patients with slightly impaired ROM in our study had no clinical symptoms.
Fractures that affect mechanically loaded articular surfaces and fractures that result in uneven articular surfaces are to a higher degree associated with post-traumatic osteoarthritis and disability than extra-articular fractures and non-displaced fractures [1, 10]. We found no difference in the proportions of individuals with joint space reduction when comparing the 3 Colton types of fractures. However, we found a higher proportion of individuals with radiographic degenerative changes in former type II oblique/transverse and type II comminuted fractures, than among type I fractures. It seems as if, radiographic degenerative changes are of minor clinical relevance. This view is supported by Gartsman et al. who in 29 patients, 3.6 years after the fractures, found degenerative changes in 20% of the patients, still with good or excellent outcome in virtually all [25]. Other studies have reported an even higher prevalence of degenerative changes, still with good or excellent outcomes in most patients [2, 8, 9]. We now extend the knowledge when reporting that a higher prevalence of radiographic degenerative findings is found in Colton type II oblique/transverse and type II comminuted fractures, but not in Type I fractures, and that radiographic degenerative changes are unrelated to clinical outcome.
Several reports infer the importance of obtaining even articular joint surfaces. Murphy et al. reported in 38 patients with olecranon fractures treated by surgery, a mean 2.8 years later that there were inferior outcomes in fractures with a postoperative articular diastasis of 2 mm or more [26]. These inferences were supported in another report which concluded that a 2 mm or greater diastasis in olecranon fractures is associated with osteoarthritis and disability [22]. Our data oppose these inferences. Although we found 17/95 (18%) elbows with a postoperative diastasis exceeding 2 mm, only 3/95 reported inferior elbow function. Furthermore, only 1 out of 3 patients with markedly inferior elbow function had a postoperative diastasis exceeding 2 mm. This suggests that factors beyond the postoperative joint diastasis may be of greater importance for the long-term outcomes. The different conclusion in our study compared to the studies by Murphy et al. [26, 27] and Eriksson et al. [22] may be attributable to different inclusion criteria and the fact that the cited studies also included other types of fractures and other treatment strategies.
Study strengths include the large sample size, the high attendance rate, the long follow-up, the population-based inclusion and the specific subtype reports. This would help us to improve accuracy in the future when discussing the expected outcome after each specific type of fracture. Evaluation of not only subjective, but also objective and radiographic outcomes is another study strength. The evaluations by professionals who were uninvolved in treatments and unaware of outcomes reduce the risk of bias. Weaknesses include the use of a non-validated questionnaire. If we had repeated the study today, we would have used validated PROMs such as the Disability of the Arm, Shoulder and Hand Score (DASH), the Mayo Elbow Performance Score (MEPS) or the American Shoulder and Elbow Surgeons (ASES) Shoulder Score. The lack of pre-fracture data and a clinical structured exam at fracture event forced us to use a modified Colton classification for type I fractures. It would also have been advantageous to include extra-articular fractures and fracture luxation, making it possible to evaluate type II a and type II d fractures as well. It would also have been advantageous to have elbow strength measured by a strain gauge torque sensor.
CONCLUSION
There are in general favourable long-term outcomes of isolated Colton type I, type II oblique/transverse and type II comminuted olecranon fractures, with no differences in subjective outcomes between the 3 subtypes. Development of postoperativ elbow joint space reduction is rare. In contrast, radiographic degenerative changes are common, although without clinical relevance. There are no different outcomes after fracture in the dominant or non-dominant arms or in men and women.
LIST OF ABBREVIATIONS
| mm | = Millimetres |
| SD | = Standard Deviations |
| 95% CI | = 95% Confidence Intervals |
| ANOVA | = Analyses of Variance |
| ROM | = Range of Motion |
| PROM | = Patient-Reported Outcome Measures |
| DASH | = Disability of the Arm, Shoulder and Hand Score |
| MEPS | = Mayo Elbow Performance Score |
| ASES Shoulder Score | = American Shoulder and Elbow Surgeons Shoulder Score |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethical Committee of the Lund University, Sweden (LU-345-95).
HUMAN AND ANIMAL RIGHTS
The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
We obtained verbal consent from all participants prior to data collection.
FUNDING
This study was funded by grants from ALF, FoUU, Herman Jarnhard, Kock and Skane University Hospital Foundations.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Magnus Karlsson participated in data collection.








