All published articles of this journal are available on ScienceDirect.
Diaphyseal Femoral Fractures in Children: Comparison Between Elastic Stable Intramedullary Nailing and Conservative Management
Abstract
Background:
Femoral shaft fractures are one of the most common fractures of the lower extremities in children. Although many approaches and options are available for their treatment, the most appropriate treatment option for school going children is still debatable.
Objective:
This study investigated the efficacy, safety, and outcome of surgical intervention with Elastic Stable Intramedullary Nailing (ESIN) in 3–12-year-old children with diaphyseal femoral fractures and compared them with those of conservative management.
Methods:
In this prospective study, 41 children with diaphyseal femoral fractures were recruited between April 2013 and April 2016. The fractures were divided into two equal groups: one treated with ESIN, and the other with early spica casting or noninvasive traction followed by hip spica casting. Demographic data, clinical information, and serial radiographic findings were collected and compared between the two groups. Flynn’s scoring criteria pertaining to time to union, assisted weight bearing, independent ambulation, return to school, and complications were applied. Fischer’s exact test was used for statistical analyses.
Results:
Compared with spica casting-treated fractures, ESIN-treated fractures healed faster with lower average time to assisted weight bearing, independent ambulation, and return to school. Hip spica-treated children had a higher rate of major complications than ESIN-treated children. At 1-year follow-up, higher limb length discrepancy was reported in hip spica-treated children than in ESIN-treated children (P < 0.001).
Conclusion:
ESIN is a safe and effective approach for treating femoral shaft fractures in children; it provides better functional and radiographic outcomes than spica casting and can be used in preschool-age children.
1. INTRODUCTION
Femoral shaft fractures are one of the most common fractures of the lower extremities in children, with an incidence rate of 20–25 per 100,000 children per year [1, 2]. Different treatment approaches can be used for their successful treatment depending on the child’s age, type of fracture, surgical facilities available, associated injuries, and socioeconomic factors [3]. Various treatment options are available, including closed reduction with hip spica casting and surgical stabilization with intramedullary devices, submuscular bridging plate and screws, and external fixators [2-9]. Although spica casting is effective in <5-year-old children, rigid antegrade interlocked intramedullary nail is the best option for skeletally mature teenagers. Nonetheless, the most suitable treatment option for school going children is controversial [10, 11].
Complications associated with closed reduction with hip spica castings, such as malunion, joint stiffness, angulation, shortening, and delays in functional recovery, are common in older children. Moreover, conservative treatment options require prolonged hospitalization, increasing burden on the hospital authorities and causing financial losses to the patient’s family [12-14]. In the last decade, there has been a gradual trend towards new treatment approaches that allow rapid mobilization. Most orthopedic surgeons have recognized the adverse psychosocial effects associated with prolonged hospitalization and spica cast immobilization on children and their families [13]. These psychosocial factors, along with the increasing emphasis toward minimizing the hospital stay and its consequences, have generated interest for the internal and external fixation of pediatric diaphyseal femoral fractures, even though the combination of traction and cast immobilization provides favorable results [9, 15].
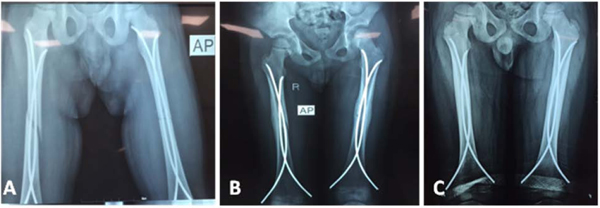
The ideal implant for treating most femoral fractures in children would be a simple, load-sharing, internal implant that allows mobility and maintenance of the alignment and length of the extremity until bridging callus forms. The implant would use a child’s dense bone, rapid healing, and remodeling ability without endangering the distal femoral physis or femoral head blood supply. Elastic Stable Intramedullary Nailing (ESIN) offers these features. However, although it is an effective treatment option, it is not free of complications (Fig. 1) [4, 5, 16].
Ligier et al. [17, 18] reported excellent results of ESIN in the treatment of femoral shaft fractures in children. Numerous recent studies have described the outcome and complications of treatment with ESIN; however, few studies have compared the results of ESIN with those of conservative management methods, such as hip spica casting [3, 10].
Therefore, this study aimed to examine the efficacy, safety, and outcome of surgical fixation with ESIN in the treatment of 3–12-year-old children with femoral shaft fractures and to compare them with those of hip spica casting.
2. MATERIALS AND METHODS
2.1. Study Design and Participants
This prospective comparative study included 3–12-year-old children with diaphyseal femoral fractures who visited Shar and Slemani Teaching Hospitals between April 2013 and April 2016. Forty-one children were recruited and divided into two groups of equal number of fractures; the decision between surgical and conservative treatments was at the discretion of the surgeons, depending on their familiarity with the treatments. The first group was treated with elastic stable intramedullary nailing (the ESIN group), and the second group was treated with hip spica casting with or without traction (the SPICA group). The ESIN group included 20 children with 21 diaphyseal femoral fractures (bilateral fractures in one patient), whereas the SPICA group included 21 children with 21 femoral shaft fractures. The exclusion criteria were as follows: patients >12 or <2 years old or having Gustilo–Anderson fracture type III, pathological fractures, subtrochanteric and supracondylar fractures, neurological disorders (e.g., myelomeningocele and cerebral palsy), or metabolic bone disorders. The study followed the principles of the Declaration of Helsinki and was approved by the Institutional Ethical Committee. Informed consent was obtained from the parents of all participants.
2.2. Surgical Procedure and Postoperative Management
Surgery was performed under general anesthesia on a traction or radiolucent imaging table. Preoperative antibiotics (ampicillin + cloxacillin) were parenterally administered within 1 h of incision and continued for 24 h postoperatively. The standard technique for ESIN insertion described by Flynn et al. [4] and Narayanan et al. [5] was used wherein two identical titanium nails were inserted in a retrograde fashion through the distal part of the femur. The diameter of the nails was 40% of the narrowest diameter of the femoral diaphysis [4]. Fractures were reduced under fluoroscopic guidance. Nails were bent to a long smooth curve of approximately 30°. The nails were cut distally, keeping only 10–20 mm of their length outside the cortex. The extraosseous portion of the nail was not bent away from the bone and was left lying to be flushed with the metaphyseal flare to avoid future irritation. Open reduction was required in two of the 21 fractures due to lack of the F-tool for reduction as the surgeon was in the initial learning curve and traction table was not available.
Intraoperative stability was assessed by applying an axial load. In the case of comminuted fractures and doubtful stability, a single-leg hip spica cast was used for 2 weeks. Postoperatively, patients were mobilized using crutches or assisted weight bearing with the help of a physiotherapist and parents when the fracture caused no pain. After the appearance of a calcified external callus, independent ambulation was allowed. Titanium nails were removed under general anesthesia when the fracture line was no longer visible radiologically.
2.3. Data Collection
Demographic data of the participants, namely age, gender, weight, and mechanism of injury, were collected. Mechanisms of injury included low-energy (fall at the ground level), medium-energy (such as sport-related injuries, falling of a heavy object on the thigh, and fall from a bicycle), and high-energy (such as motor vehicle accident, fall from a height of ≥2.5 m, and collision between a motor vehicle and a pedestrian) traumas. The time spent in traction and its outcome as a definitive treatment, fracture description, presence of associated injuries, and operative details were also documented.
2.4. Follow-up
The follow-up period was 24 weeks. One patient in both groups was lost to follow-up, and the rest were followed until their fracture united and they resumed their normal activities. A questionnaire was administered to both groups during follow-up visits at 2, 6, 12, and 24 weeks. The range of motion of the knee and hip joints was recorded, and measurements of angulation in the sagittal and coronal planes were taken on standard anteroposterior and lateral radiographs. The patients were examined for limb length discrepancy and rotational malalignment. Age-based guidelines for acceptable alignment and limb length discrepancy were based on the parameters by Kasser and Beaty (Table 1) [6].
| Age | Varus/Valgus | Anterior/Posterior |
Shortening (mm) |
|---|---|---|---|
| 2–5 years | 15° | 20° | 20 |
| 6–10 years | 10° | 15° | 15 |
| 11 years to maturity | 5° | 10° | 10 |
The parameters included the range of motion of the knee and hip joints, measurements of angulation in the sagittal and coronal planes, time for beginning assisted weight bearing, full weight bearing, returning to school, removal of spica cast or titanium nails, presence of complications related to neurovascular system, knee synovitis, delayed union or nonunion, refracture, unscheduled surgery, and nail insertion site problems, such as pain, bursa formation, backed out nails, and infection. The recovery milestones, such as time to start assisted weight bearing, full weight bearing, return to school, spica cast removal, and nail removal, were also recorded.
Major complications were defined as loss of reduction, delayed union, or permanent disability due to lack of treatment. Minor complications included temporary problems not requiring an additional surgical intervention and not causing a threat of permanent disability. The outcomes were graded as excellent, satisfactory, or poor according to the TEN outcome scoring system (Table 2) described by Flynn et al. [4].
| Excellent | Satisfactory | Poor | |
|---|---|---|---|
| Leg length discrepancy | <1.0 cm | 1.0–2.0 cm | >2.0 cm |
| Malalignment | <5° | 5°–10° | >10° |
| Pain | None | None | Present |
| Complications | None | Minor and resolved | Major complication and/or lasting morbidity |
Children exceeding the criteria in the poor category were assigned the worst result.
2.5. Statistical Analysis
Statistical Package for Social Sciences version 22 and Microsoft Excel spreadsheets were used for statistical analyses. Data are presented as mean and standard deviation (SD). Two-sample t-tests were used to evaluate the degree of differences in continuous data between the two groups, and chi-square test was used to determine the difference in the proportions of various parameters between the groups. P < 0.05 was considered statistically significant.
3. RESULTS
Of the 41 patients, one from each group was lost to follow-up and therefore excluded from the analysis. The demographic data and patient characteristics are shown in Table 3.
| Characteristic | SPICA | % | ESIN | % | P |
|---|---|---|---|---|---|
| Age (years) | – | – | – | – | – |
| Mean ± SD | 5 ± 1.4 | – | 6 ± 2.4 | – | 0.11 |
| Range | 2–8 | – | 3–11 | – | – |
| Weight (kg) | – | – | – | – | – |
| Mean ± SD | 18.5 ± 3.3 | – | 21.7 ± 5.9 | – | 0.04* |
| Range | 14–28 | – | 13–36 | – | – |
| Males | 15 | 75 | 16 | 80 | – |
| Females | 5 | 25 | 4 | 20 | – |
| Male/Female | 3/1 | – | 4/1 | – | – |
| Time to definitive treatment (days) | – | – | – | – | – |
| Mean ± SD | 3.4 ± 3.1 | – | 2.3 ± 0.9 | – | 0.13 |
| Range | 1–10 | – | 1–4 | – | – |
| Mechanism of injury | – | – | – | – | |
| Low-energy trauma | 8 | 40 | 4 | 20 | – |
| Medium-energy trauma | 6 | 30 | 5 | 25 | – |
| High-energy trauma | 6 | 30 | 11 | 55 | – |
| Fracture location | – | – | – | – | |
| Midshaft | 14 | 70 | 14 | 70 | – |
| Proximal third | 4 | 20 | 6 | 30 | – |
| Distal third | 2 | 10 | none | 0 | – |
| Fracture pattern | – | – | – | – | |
| Spiral | 10 | 50 | 5 | 25 | – |
| Oblique | 3 | 15 | 3 | 15 | – |
| Transverse | 6 | 30 | 11 | 55 | – |
| Winquist type 1 | 1 | 5 | none | – | – |
| Winquist type 3 | none | – | 1 | 5 | – |
| Operative time (min) | – | – | – | – | |
| Mean ± SD | 30.3 ± 4.1 | – | 60.8 ± 21 | – | <0.0001* |
| Range | 25–40 | – | 35–110 | – | – |
The ratio of boys-to-girls in the SPICA and ESIN groups was 3:1 and 4:1, respectively. The mean age was comparable between the two groups. The ESIN group children were relatively heavier than the SPICA group children (P < 0.05). More than half of the ESIN group children had high-energy injuries, whereas low-, medium-, and high-energy injuries were somewhat equally distributed in the SPICA group. The mid-shaft fracture was the most common fracture type in both groups. The predominant fracture pattern was spiral in the SPICA group and transverse in the ESIN group. In terms of associated injuries, in the SPICA group, only one patient had fractures of the left tibia and fibula, whereas, in the ESIN group, two patients had fractures of the left tibia and fibula; one had fractures of the ilium, contralateral femur, and clavicle; and one had supracondylar fracture of the humerus.
Table 4 shows the comparison of various parameters and outcomes between the two groups. The average operative time was significantly shorter in the SPICA group than in the ESIN group (P < 0.0001). The average durations of hospital stay (P = 0.06) and follow-up (P = 0.62) were comparable between the SPICA and ESIN groups. The ESIN group started assisted weight bearing and independent ambulation and returned to school significantly earlier than the SPICA group (all, P < 0.0001).
| – |
SPICA (Mean ± SD) |
ESIN (Mean ± SD) |
P |
|---|---|---|---|
| Duration | – | – | – |
| Spica removal (weeks) | 6.6 ± 1.2 | – | – |
| Assisted weight bearing (weeks) | 8.3 ± 1.4 | 4 ± 2.4 | <0.0001* |
| Assisted weight bearing with exclusion of associated lower limb fractures (weeks) | 8.2 | 3 | <0.0001* |
| Full weight bearing (weeks) | 9.8 ± 1.7 | 6.3 ± 2.5 | <0.0001* |
| Full weight bearing with exclusion of associated lower limb fractures (weeks) | 9.7 | 5.4 | <0.0001* |
| Return to school (weeks) | 9.8 | 6.7 | <0.0001* |
| Removal of the nails (months) | – | 5.3 ± 2.3 | – |
| Postoperative duration | – | – | – |
| Hospital stay (days) | 4.4 ± 2.1 | 3.3 ± 1.2 | 0.06 |
| Follow-up duration (months) | 11.3 ± 3.8 | 12.1 ± 6 | 0.62 |
| Union (weeks) | 7.2 ± 1.2 | 6.2 ±1.6 | 0.043* |
| Alignment | – | – | – |
| Coronal plain angulation (°) | 6.9 ± 7.96 | 1.9 ± 8.6 | 0.08 |
| Sagittal plain angulation (°) | 5.9 ± 10.2 | 3.75 ± 7.4 | 0.46 |
| Rotational malalignment (°) | 8.2 ± 7.3 | 2 ± 4.5 | 0.008* |
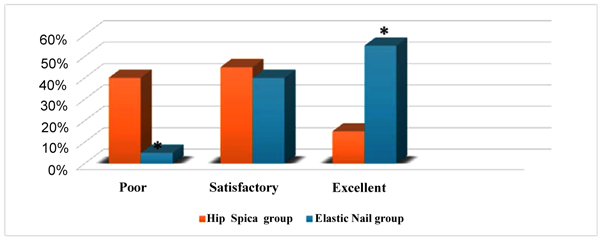
Limb length discrepancy was significantly less in the ESIN group (0.25 cm) than in the SPICA group (1.1 cm; P = 0.002). Based on the evaluation of outcome measures using the Flynn’s scoring criteria, in the ESIN and SPICA groups, 55% and 15% patients had excellent outcomes, 40% and 45% had satisfactory outcomes, and 5% and 40% had poor outcomes, respectively (Figs. 1-4).
Refracture occurred in only one patient in the ESIN group following nail removal due to an incomplete union; this refracture was subsequently treated with plate fixation. Problems related to the nail insertion site were observed in six patients, three of whom reported having pain at the lateral nail insertion site, two demonstrated ulceration and superficial infection that were cured after nail removal, and one showed bursa formation over the lateral nail insertion site; however, none of these patients required unscheduled reoperations. Overgrowth of 2 cm was reported in one patient in the ESIN group, whereas shortening of 0.5–1 cm was reported in three patients in the SPICA group.


4. DISCUSSION
During the last few decades, there had been an increasing trend toward surgical management of children’s fractures that were previously treated conservatively [19]. Although hip spica casting is a safe and effective treatment for many pediatric femoral shaft fractures, the associated complications, such as skin irritations, malunion, joint stiffness, and prolonged immobilization, are common [17, 18, 20, 21]. Numerous studies have also increased awareness regarding adverse psychosocial, educational, and economic effects of spica cast immobilization on the affected children and their families [13, 14]. Recently, ESIN has been advocated by many studies for treating pediatric femoral shaft fractures [1, 3-5]. Although many studies have compared ESIN and spica casting in several countries, only a few have been conducted in Iraq [22, 23]. Furthermore, surgical treatment with ESIN in lower-age group (3-year-old) patients has been evaluated in few studies in other countries [16, 24].
Both treatment modalities have benefits and drawbacks. The advantages of fixation using ESIN for femoral shaft fractures in children include less postoperative immobilization, faster return of the range of motion of the joints, and easier care as parents can avoid the difficulties associated with handling a child with hip spica casting for several weeks [23, 24]. The drawbacks of ESIN include a possible risk of infection, a rare but serious possibility of injury to the adjacent neurovascular structures, the requirement of a second surgery to remove the implant (because of complications or as an elective procedure), and an increase in operative time compared with that required for spica casting. Despite internal fixation in ESIN, some patients with comminuted or length-unstable fractures may require additional external support, such as hip spica cast, for a few weeks [4, 5].
In this study, we observed a significantly higher operative time with ESIN than with hip spica casting; however, the duration of hospital stay between the two groups was comparable. This contrasted with the findings of Greisberg et al. [25] and Flynn et al. [11] who reported a shorter hospital stay for the ESIN-treated patients. The reasons for this discrepancy are that these studies used traction for 3 weeks in their SPICA group and the extended duration in our ESIN group was due to the time spent in the management of associated injuries. Our finding supported that of Saseendar et al. [10] and Heffernan et al. [24] who found that fracture healing is faster in ESIN-treated patients than in conservatively treated patients. Further, we observed that the ESIN group children could start assisted weight bearing earlier than the SPICA group children. These findings were consistent with those of Flynn et al. [11] and Shemshaki et al. [3] who found that the ESIN-treated children start independent weight bearing faster than hip spica cast-treated children. The recovery time frames in our study were comparable or slightly shorter than those reported by Saseendar et al. [10] and Shemshaki et al. [3] and even shorter than those reported by Flynn et al. [11]. This could be because, in previous studies, traction was used for 3 weeks in hip spica cast-treated patients, and the patients were older in these previous studies than in our study. On the other hand, the recovery time frames in our study were slightly longer than those reported by Heffernan et al. [24], probably because the mean age of their patients was less than that of our patients.
In our study, the significant difference in the recovery times between the two treatment groups was probably attributable to the fact that the ESIN group children commenced weight bearing once the pain stopped before achieving radiographic union, whereas it is difficult to keep them on non-weight bearing once they feel pain-free. The SPICA group was kept immobilized until there was evidence of radiographic union at an average of approximately 7 weeks, and it is usual for a child to take time to resume ambulation after a period of immobilization due to joint pain and stiffness. Similarly, early recovery milestones were reported by Greisberg et al. [25] in ESIN-treated patients.
In our study, major complications were higher in the SPICA group than in the ESIN group, which reported just only one major complication and six minor complications. The one major complication occurred in a 10-year-old boy (31 kg) who had sustained a left-sided midshaft transverse fracture due to a high-energy trauma. Delayed union, in this case, resulted in prolonged immobilization (4.5 months), followed by a refracture that occurred while removing the backed out nails. The refracture was subsequently treated with plate and screws, and the child resumed assisted weight bearing 4 weeks after the last surgery; the fracture healed uneventfully. The refracture had occurred because the surgery was performed in the initial period without using orthopedic table; open reduction was needed; and the nails were smaller than 40% of the narrowest diameter of the diaphysis, were non-divergent, did not reach the final destination, and did not achieve the biomechanical principles of three-point fixation of ESIN. Similar rates of major complications of ESIN were reported by Luhmann et al. [2/43 fractures (4.6%)] [16] and Narayanan et al. [2/79 fractures (2.5%)] [5]. Furthermore, in the study by Narayanan et al. [5], reoperations were considered in 10 of 79 patients (13%), but only two of them were considered to have major complications (reoperations in the remaining eight patients were aimed at trimming or proximal advancement of symptomatic nails). Reoperation for major complications was required in only one of these two patients.
We found minor differences in the mean coronal and sagittal angulations between the ESIN and SPICA groups, consistent with the findings of Saseendar et al. [10], Heffernan et al. [24], and Ramo et al. [26]. Two patients in the SPICA group showed unacceptable alignment at the time of union, one of whom was a 4-year-old boy with 20° varus and 30° anterior angulation, and another was a 4.5-year-old boy with 30° varus and 25° anterior angulation; both patients also showed limb length discrepancy at the time of union (2- and 2.5-cm shortening, respectively). These were considered as poor outcomes according to the Flynn’s scoring criteria [4]. The complications were most likely due to the technique used in spica casting and noncompliance to follow-up visits as they could have been prevented by wedging of the cast at approximately 7–10 days postoperatively. Longer follow-up is required to assess the final remodeling and the effect of these angular deformities on these children’s functional outcomes [27]. Moreover, limb overgrowth observed in our study might be attributable to the near anatomic reduction usually achieved with ESIN and the stimulations resulting from breaching of the periosteum and hyperemia in the region.
In our study, the mean rotational malalignment was greater in the SPICA group than in the ESIN group, consistent with the finding reported by Saseendar et al. [10]. One SPICA group patient demonstrated a significant rotational malalignment (20°–25° internal rotation) and in-toeing gait at 1-year follow-up. Therefore, although early spica casting is a favorable treatment option in young children, complications may occur if appropriate techniques are not used. No child in the ESIN group lost rotational alignment, consistent with the finding reported by Flynn et al. [11].
Pain or problems at the nail insertion sites were reported in 7%–29% cases by Flynn et al. [4] and Ligier et al. [18] and in 40% cases by Luhmann et al. [16]. In our study, six (30%) children treated with ESIN complained about insertion site problems.
In our study, 60% of the ESIN-treated patients showed excellent outcomes according to Flynn’s scoring criteria. The outcomes in other similar studies were not as high as those in our study. In a multi-center study conducted by Flynn et al. [4], the outcomes were satisfactory in 18 of the 58 (31.03%) ESIN-treated patients. However, among these 18 patients, malalignment was observed in six patients, length inequality in six, soft tissue irritation in four, refracture after nail removal in one, and backed out of nail in one. Luhmann et al. [16] reported satisfactory outcomes in 22 of the 43 (51%) fractures treated with ESIN. Ligier et al. [18] reported excellent outcomes, with no major angular or rotational malunion, in 123 fractures treated with ESIN. Due to the significantly shorter time to assisted weight bearing, independent ambulation, and return to school and significantly lower rate of major and minor complications in ESIN-treated children than in spica casting-treated children, we consider flexible intramedullary nailing a safe and effective method for treating diaphyseal femur fractures in children, with better early outcomes than those by spica casting.
This study has few limitations. First, a selection bias was possible because the fractures in the ESIN group likely included those that were caused by high-energy trauma with reported associated injuries or fractures and were therefore indicated for surgical intervention. Second, the duration of traction in the SPICA group was not equal in all cases and was influenced by factors such as bed occupancy, family considerations, and the surgeon’s decision. Third, we did not determine the long-term outcomes in our study as it is well known that the long-term outcomes of the treatment of diaphyseal femoral fractures in this age group are usually satisfactory and unlikely to cause a permanent disability. Fourth, our mean follow-up duration of approximately 11–12 months was short for determining the final alignment or limb length discrepancy.
CONCLUSION
In conclusion, children with femoral shaft fractures treated with ESIN achieved better and faster recovery with a lower rate of complications than those treated with hip spica casting. Most complications of ESIN in our study were minor and resolvable. Therefore, ESIN is a safe and effective method for treating femoral shaft fractures that provide better functional and radiographic outcomes than hip spica casting. Despite the technical pitfalls, ESIN should be the preferred modality for treating femur shaft fractures in 3–12-year-old children and should be selected after considering the patients’ age, weight, and fracture pattern; hospital facilities; and family’s psychosocial situation. We recommend the use of orthopedic tables during ESIN fixation for the ease of reduction, shorter operative time, and minimizing the need for unnecessary incisions. ESIN should be performed cautiously in segmental or comminuted fractures, and external support or other methods of fixation should be considered whenever adequate stability is not expected. Nail ends should not be bent away from the bone so that they can be flushed with the metaphyseal cortex to minimize problems at the nail insertion sites.
LIST OF ABBREVIATIONS
| ESIN: | = Elastic Stable Intramedullary Nailing |
| SD: | = Standard deviation |
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study followed was approved by the Institutional Ethical Committee.
HUMAN AND ANIMAL RIGHTS
The reported experiments are in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931)
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants.
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial, or otherwise.
ACKNOWLEDGEMENTS
Declared none


