All published articles of this journal are available on ScienceDirect.
Microgeodic Disease Affecting the Fingers and Toes in Childhood: A Case Report
Abstract
Microgeodic disease is a disease of unknown etiology that affects the fingers and toes of children, with ≥ 90% of cases involving the fingers alone. We present a rare case of microgeodic disease affecting an index finger and two toes simultaneously in a 7-year-old girl. X-ray and magnetic resonance imaging (MRI) showed multiple small areas of osteolysis in the middle phalanges of the left index finger, hallux, and second toe. Microgeodic disease was diagnosed from X-ray and MRI findings, and conservative therapy involving rest and avoidance of cold stimuli was provided. Although pathological fractures occurred in the course of conservative treatment, the affected finger healed under splinting without any deformity of the finger.
INTRODUCTION
Microgeodic disease was first reported by Maroteaux in 1970 [1], affecting the fingers or toes of children and causing spindle-shaped swelling and redness. However, the cause of microgeodic disease remains unclear. The disease prognosis is good, and most cases heal spontaneously without residual deformity or sequelae, but rare complications include pathological fracture and subsequent malunion [2, 3]. Over 90% of symptoms are seen in the fingers, and cases affecting the toes are rare [4-9]. Moreover, no cases with both fingers and toes affected at the same time have been reported. We report herein a rare case of microgeodic disease involving both fingers and toes concurrently.
CASE REPORT
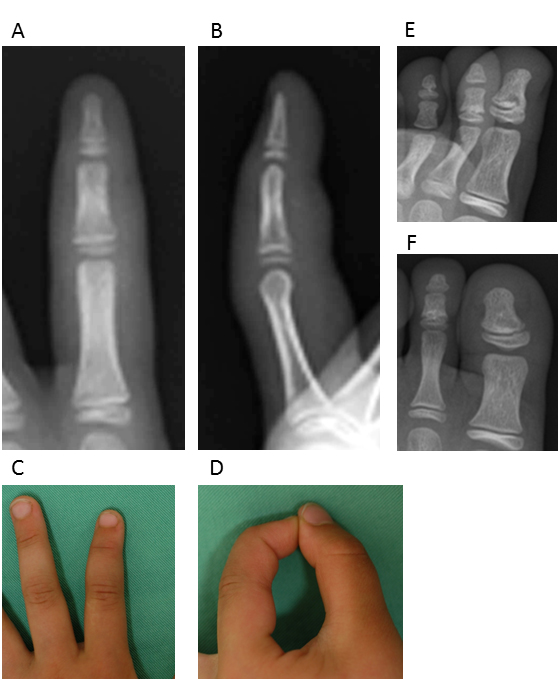
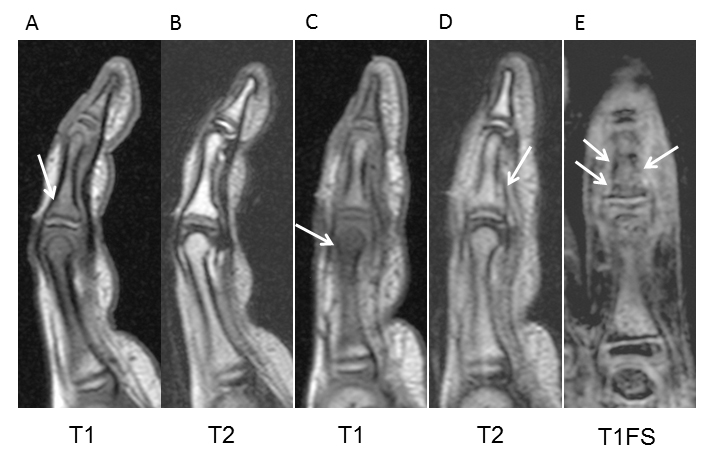
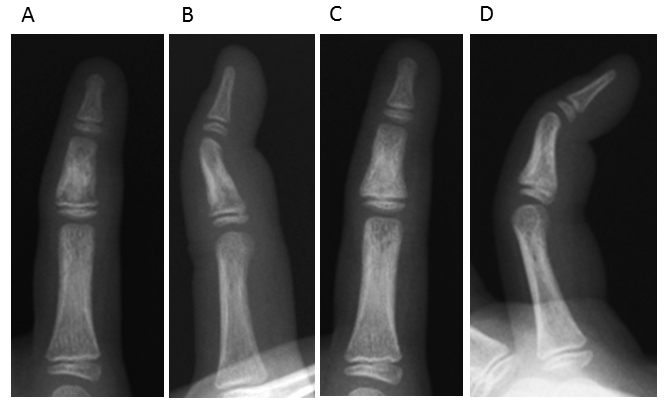
A 7-year-old girl visited a local doctor with swelling and mild pain in the left index finger and hallux and second toe of the left foot without any apparent experience of injury in February. She often played outside, and always went barefoot in the house. No past history or family history was evident. She was subsequently referred to our institution in March. Radiography at the initial consultation showed small, round, radiolucent images in the middle phalanx of the left index finger, as well as an irregular shadow on the distal phalanx of the left hallux and middle phalanx of the left second toe (Fig. 1). Conditions at that time included mild pain, spindle-shaped swelling, and redness over the left index finger and left hallux and second toe (Fig. 1). Range of motion of the left index finger was from 0-90° for the distal interphalangeal (DIP) joint and 0-70° for the proximal interphalangeal (PIP) joint. Similarly, swelling, redness, and cyanosis were found on the left toes. Laboratory data, including a blood cell count and routine biochemical screening tests for function of the liver and kidneys, amylase, total protein, and total cholesterol showed no abnormalities. Magnetic resonance imaging (MRI) showed low-intensity areas on T1-weighted and T1-weighted fat suppression imaging (Fig. 2). Clinical findings, radiographs, and MRI led to a diagnosis of microgeodic disease, and we instructed the patient to rest and avoid cold stimuli. However, this patient could not keep the affected hand and foot at rest. Two months after the onset of symptoms, radiography showed an irregular shadow and fracture-like condition in the middle phalanx of the left index finger (Fig. 3). We immobilized the affected finger with a splint to avoid deformity and shortening of the finger. Within 3 months of onset, the swelling, redness, pain, and limited range of motion improved, but an irregular shadow on the middle phalanx of the left index finger was still evident on radiographs. Swelling and redness in the left hallux and second toe were also improved, but irregular shadows again remained visible on radiographs (Fig. 4A, B). Within 4 months of onset, redness and swelling of the toes improved, and pain subsided. Irregular shadows on the left index finger and left hallux and second toe were also no longer apparent on radiographs (Fig. 4C, D). The patient is currently leading a normal life. The parents of the patient provided written informed consent.

DISCUSSION
In 1970, Maroteaux first described this condition of unknown cause affecting the fingers of children [1]. This disease is comparatively rare, with only a few cases reported, and the incidence and prevalence remain unclear. This may be due to the good prognosis of phalangeal microgeodic disease and the self-limiting nature of the disease process, with symptoms resolving within 3-6 weeks without specific treatment [4, 7]. In addition, the disease may go undiagnosed in the absence of adequate knowledge regarding this pathology. Typically, radiographic examination shows a small, round radiolucency at the edge of the metaphysis [8, 10]. Because the radiographic appearance resembles a microgeode, the condition was named ‘microgeodic disease’. Commonly, the middle phalanx of the finger, particularly the index finger, is affected. Cases involving toes are rare [3, 10], and no cases with both fingers and toes affected at the same time have been reported. We treated a rare case of microgeodic disease concurrently involving a finger and both toes.
The majority of cases have been reported in Japan [2, 3, 7-13]. Many cases occur in children up to 15 years old, and the mean age of onset is 3 years 11 months [8]. In previous reports, this disease has been shown to appear during the cold season between December and March in Japan [7, 9, 12]. Symptoms include swelling, redness, local heat, and mostly mild pain in the fingers. The present patient showed a similar clinical profile. The lesion appears to result from vascular insufficiency in the hands and feet causing bone infarction secondary to intense vasospasm precipitated by cold [9]. Other possible causes of this disease include infection and allergic reaction. The present patient had been exposed to cold stimuli prior to symptom onset and symptoms resolved spontaneously with the arrival of warmer weather. Exposure to cold stimuli was thus considered the main cause in this case.
Differential diagnoses include osteomyelitis, tuberculosis, sarcoidosis, syphilis, parathyroid dysfunction, and complex regional pain syndrome [3, 11, 14]. In relation to this case, blood testing conducted at the time of first consultation showed negative results for osteomyelitis, syphilis, and parathyroid dysfunction. However, in cases where the condition persists, biopsy may be necessary to definitively exclude infection. A timely clinical diagnosis by a physician who is aware of the disease could prevent the need for invasive investigations [14]. Generally, microgeodic disease can be differentiated from tuberculous osteitis in several ways [8, 13, 15, 16]. Radiographically, tuberculous osteitis demonstrates unique medullary destruction with periosteal cortical thinning, while microgeodic disease does not demonstrate reactive periostitis unless another condition such as pathological fracture is present. Moreover, the small areas of lysis seen in microgeodic disease are not present in most patients with tuberculous osteitis [8]. We consider MRI to be a helpful investigative modality in those cases of phalangeal microgeodic disease in which doubt remains following clinical and radiographic assessments [4]. MRI allows a greater appreciation of the bone areas affected and adds specificity to radiography with regard to diagnosis. In this case, radiography and MRI showed irregular shadows, not reactive periostitis, in the finger and toes. Microgeodic disease can be differentiated radiographically from osseous sarcoidosis in that the latter pathology shows a lace-like, coarse trabecular pattern, large cystic cavity, and no evidence of periosteal new-bone formation [8, 11]. Chest radiography helps to exclude sarcoidosis, as lung involvement is usual in patients with osseous sarcoidosis [4].
This disease has a good prognosis, and the condition often improves with conservative therapy [1, 3, 8, 11]. However, early diagnosis is often difficult due to the rarity of this pathology. Delayed diagnosis may lead to clinical fracture and subsequent residual deformity, early closure of the epiphyseal lines, and a limited range of motion [3, 7, 11]. Yamamoto et al. reported a patient with rapid digital shortening caused by collapse attributed to bone atrophy in the metaphyseal region of the middle phalanx or repeated minor trauma to the affected finger [3]. Kaibara et al. reported a patient with pathological fracture of the middle phalanx, resulting in angulation deformity [2]. Sato et al. recommended protecting the affected digits with a splint to avoid stress fracture or physical damage to the physis [8]. In our case, the patient could not keep the affected hand and foot at rest. As a result, pathological fracture developed in the middle phalanx of the left index finger. Although this case healed with no serious consequences despite pathological fracture of the finger, some reports have described angulation deformity as an outcome [2, 3]. We therefore believe this disease should be considered, to allow correct diagnosis and careful follow-up to avoid complications.
LIST OF ABBREVIATIONS
| DIP | = Distal interphalangeal |
| MRI | = Magnetic resonance imaging |
| PIP | = Proximal interphalangeal |
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


