All published articles of this journal are available on ScienceDirect.
Retained Sponge: A Rare Complication in Acetabular Osteosinthesis
Abstract
Retained sponges after a surgical treatment of polytrauma may cause a broad spectrum of clinical symptoms and present a difficult diagnostic problem. We report a case of retained surgical sponge in a 35-year-old man transferred from another hospital, that sustained a open acetabular fracture. The fracture was reduced through a limited ilio-inguinal approach. After 4 days, he presented massive wound dehiscence of the surgical approach. An abdominal CT scan showed, lying adjacent to the outer aspect of the left iliac crest, a mass of 10 cm, identified as probable foreign body. The possibility of this rare complication should be in the differential diagnosis of any postoperative patient who presents with pain, infection, or palpable mass.
Introduction
Retained sponges after a surgical treatment may cause a broad spectrum of clinical symptoms and present a difficult diagnostic problem, so orthopaedic surgeons should be aware of this possibility. We report a case of retained surgical sponge in a patient and illustrate the surgical findings of this infrequent but critical cause of postoperative complications.
Case report
A 35 year old man was admitted in our department, transferred from another hospital, after a car accident.
He sustained an anterior wall left acetabular fracture extended to the ilium [1], cranioencephalic trauma with subdural hematoma, chest wall trauma with six costal fractures, and a large traumatic gluteal wound that was sutured, so the acetabular fracture could be considered as open, Tipe 3A of Gustillo [2]. He developed a nosocomial pneumonia, caused by pseudomonas aeruginosa, during his stay in the Intensive Care Unit, and the wound needed to be dressed several times.
On arrival at our center, 45 days after the initial accident, the patient was stable and the gluteal wound showed no signs of complication, so we decided to operate the pelvic fracture, as it affected almost the vast majority of the iliac wing and was severely displaced (Fig. 1).

Plain radiograph of the acetabular fracture.

Wound dehiscence of the anterior surgical approach.
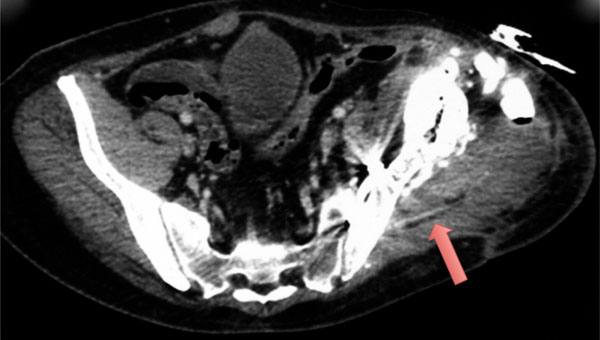
The CT-scan findings describe a mass of 10 cm, identified as probable foreign body (arrow).

Steps of the posterior wound revision. The patient was positioned in lateral decubitus. Retained sponge on a proper surgical sponge.
The fracture was reduced through a limited ilio-inguinal approach, using just the lateral window, and was fixed by 2 plates and screws.
After 4 days, he presented with fever and massive wound dehiscence of the surgical approach with abundant exudate (Fig. 2).
Laboratory examination showed normal leukocyte count, thrombocythemia and raise of inflammatory markers.
An abdominal CT scan was performed, showing, lying adjacent to the outer aspect of the left iliac crest, a mass of 10 cm, identified as probable foreign body (Fig. 3). Surgery was performed and confirmed the diagnosis of a retained surgical towel (Fig. 4). Profuse irrigation was done followed by wounds closure. Culture of the foreign body was negative. Four days later, he was asymptomatic and there were no problems with the wounds healing and no further episodes of fever, so the patient was discharged well from hospital.
Discussion
Retained foreign objects after surgical or invasive procedures continue to challenge surgeons and operating room staff as major errors that must be avoided. The most common retained surgical item that requires a second operation to remove is a surgical cotton gauze sponge, probably because of their ubiquity [3]. Once they are placed within a tissue space and absorb blood, their original shape and color becomes unrecognizable and cannot be seen in the surgical field, making them hard to find.
These situations often leave the medical arena and enter into the legal domain. Since these rates are calculated only on the basis of malpractice claims, they are most likely underestimated [3, 4]. Retained surgical sponges have been discovered in many ways. The accident most frequently occurs both in general and digestive surgeries and in gynecological and obstetrical surgeries [5-8]. There have been very few cases described in the literature and, to the best of our knowledge, there are not reports describing this complication in the management of pelvic fractures.
Diagnosis can be difficult if this error happens, mostly because of low clinical suspicion. A missed instrument remains silent and is discovered accidentally because it is sterile and inert. However in close proximity to the retained sponge, as happened in our case, there is an exudative, acute inflammatory reaction with the formation of an abscess, as it is made up of cotton, appearing as wound infection. This response usually leads to early detection and surgical removal.
Even if all the safety measures are taken in the operation theatre, there are still some cases in which foreign bodies are retained in the patient. This has happened particularly under conditions as emergency operations with unplanned changes in the procedure, increased body mass index, high blood loss and multiple operative teams, improper lighting in the theater and absence of a swab and instrument counting system [9].
In over 80% of retained sponge cases the count performed before the procedure is completed has falsely been called correct [10]. This most likely has to do with the fact that even a simple duty, such as counting items, in a very complex atmosphere, with multiple interferences and competing tasks, has a low but predictable error rate.
Several recommendations may help to prevent this misfortune [11]. Current practices in place in most centers include the use of surgical counting of sponges, instruments, and needles, and variably incorporate the use of intraoperative radiographs. Surgeons should perform a systematic wound examination in every case, and not close wounds in cases in which there has been an incorrect count reported. When the count is incorrect, unless the patient is unstable, wound closure must categorically be delayed until the miscounted sponge is found. Only sponges, towels, and laparotomy pads with radio-opaque markers should be used in an open cavity [12]. In our case the retained sponge, as it was a simple cotton gauze dressing used to cover the wounds instead of being a proper surgical sponge, did not contain radiopaque liners, so probably was misplaced in a wound dressing during his stay in the Intensive Care Unit, so pre and postoperative radiographs failed to locate it. Plain radiography, ultrasound, and magnetic resonance imaging have been used for diagnosis, but the first diagnostic modality to rule out a retained foreign body should be a CT scan and frequently it is the only examination needed [13, 14]. The problem is that radiologists are not fully educated about what these objects can look like, as the prevalence is low.
Imaging is the key for diagnosis but clinical suspicion is essential. The possibility of this rare complication should be in the differential diagnosis of any postoperative patient who presents with pain, infection, or palpable mass.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGeMENTS
Declared none.


