RESEARCH ARTICLE
Superficial Peroneal Nerve Incarceration in the Fibular Fracture Site of a Pronation External Rotation Type Ankle Fracture
P Ellanti*, K.M.S Mohamed , K O’Shea
Article Information
Identifiers and Pagination:
Year: 2015Volume: 9
First Page: 214
Last Page: 217
Publisher ID: TOORTHJ-9-214
DOI: 10.2174/1874325001509010214
Article History:
Received Date: 28/12/2014Revision Received Date: 31/3/2015
Acceptance Date: 10/4/2015
Electronic publication date: 26/6/2015
Collection year: 2015

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Ankle fractures are common representing up to 10% of all fractures with an incidence that is rising. Both conservative treatment and operative management of ankle fractures can lead to excellent outcomes. Neurovascular injuries are uncommon but can be a source of significant morbidity and associated poor outcome. The superficial peroneal nerve (SPN) in the lateral approach and the sural nerve in the posterolateral approach are at risk of injury. We report an unexpected finding of a superficial peroneal nerve incarcerated in the fibular fracture site of pronation external rotation type/ Weber-C ankle fracture. To the best of our knowledge we believe this to be the first English language report of an incarcerated SPN at a fibular ankle fracture site.
INTRODUCTION
Ankle fractures are common representing up to 10% of all fractures [1] with an incidence that is rising [2]. Both conservative treatment and operative management of ankle fractures can lead to excellent outcomes [3, 4]. Operative management of ankle fractures is not without its complications with wound breakdown, infections and loss of reduction being the most common [5]. Neurovascular injuries are uncommon but can be a source of significant morbidity and associated poor outcome [6].
The superficial peroneal nerve (SPN) in the lateral approach and the sural nerve in the posterolateral approach are at risk of injury [7]. We report an unexpected finding of a superficial peroneal nerve incarcerated in the fibular fracture site of pronation external rotation type/ Weber C ankle fracture. To the best of our knowledge we believe this to be the first English language report of an incarcerated SPN at a fibular ankle fracture site.
CASE REPORT
A 34-year-old man presented to the Emergency Department (ED) with pain and deformity to his left ankle subsequent to a fall playing soccer. This was an isolated closed injury. There were no neurovascular deficits on examination. Plain film radiographs revealed a pronation external rotation/Weber-C type ankle fracture (Fig. 1).
 |
Fig. (1). Anteroposterior and lateral radiographs of the right ankle demonstrating a pronation external rotation/Weber-C type ankle fracture. |
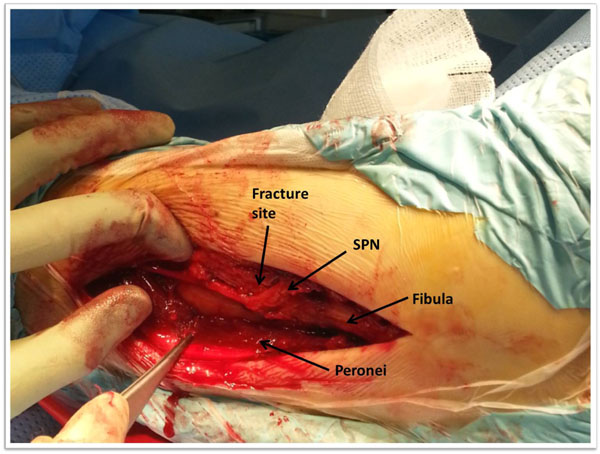 |
Fig. (2). Intraoperative photograph demonstrating the SPN coursing from an anterior position proximally into the fracture site before returning to a more anterior course distally. |
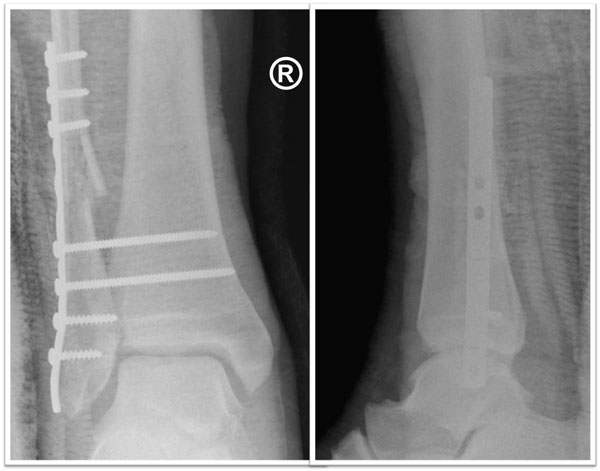 |
Fig. (3). Post-operative anteroposterior and lateral radiographs demonstrating the internal fixation of the ankle fracture. |
The patient was brought to the operation theatre for open reduction internal fixation of the ankle fracture. A direct lateral approach via a lateral incision centred on the fracture site was utilised. The SPN was identified anteriorly at the proximal end of the incision and it traversed the woundposteriorly towards the fracture site. The SPN was carefully dissected and noted to be incarcerated in the fracture site (Fig. 2) beyond which it continued distally along a more anterior course. The nerve was incarcerated in the fracture site approximately 4cm proximal to the ankle joint. This was unexpected as the patient reported no paraesthesia or sensory deficit along the SPN distribution. The nerve was carefully freed from the fracture site and upon closer inspection was intact and not visibly bruised. The nerve was transposed anteriorly and protected during the procedure. The comminuted fracture site was bridged using a 10 hole 1/3rd tubular plate and two syndesmosis diastasis screws were used as the syndesmosis which was ruptured on stressing (Fig. 3).
The patient had an uneventful post-operative course and discharged the same day. At the two week outpatient review the wound had healed. The fracture had healed at 6 weeks and the diastasis screws removed at 8 weeks at which point the patient commenced full weight bearing mobilisation. The patient reported no paraesthesia or deficits along the SPN distribution throughout the post-operative course.
DISCUSSION
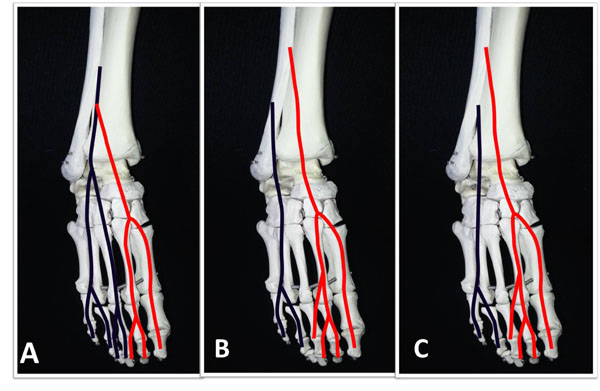
The SPN is a branch of the common peroneal nerve and has both motor and sensory function. It supplies the peroneus brevis and longus muscles (motor branch) in the lateral compartment before it perforates the fascia of the lateral compartment at which point the nerve is purely sensory. Here it further divides into two well described branches the medial dorsal cutaneous nerve (MDCN) and the intermediate dorsal cutaneous nerve (IDCN) that supply the anterolateral skin of the leg and dorsum of the foot including skin over the dorsum of 1st to 3rd toes, the medial aspect of the 4th toe and excludes the first web space which is innervated by the deep peroneal nerve [8]. The various branching patterns of the MDCN and IDCN have been studied in detail [9-12]. Blair et al. described 3 patterns (Fig. 4) and noted that Type B pattern where the IDCN coursed medially to cross the lateral aspect of the fibula at mean distance 4.5 cm above the ankle joint, occurred in 16% of cases and was particularly at risk of injury [10].
The careful examination of the injured ankle is important as SPN injuries can occur at the time the ankle fracture itself. While primary transection of the SPN is rare [13], symptomatic SPN injury has been documented up to 15% of ankle fracture patients with a significantly higher incidence in those undergoing operative fixation [6].
Based on their cadaveric study Huene and Bunnell described a safe incision site for the lateral approach which begins 12 mm posterior to the anterolateral border of the fibula at 10cm proximal to the lateral malleolar tip and extends distally to 10mmposterior to the anterolateral border of the fibula at 5cm proximal to the lateral malleolar tip [7]. Despite using this safe incision, a “straight to bone” approach to ankle fractures should be avoided. Careful dissection should be employed as the landmarks can be difficult to identify reliably in a swollen ankle. Furthermore our case report suggests that significant derangement of normal anatomy can be withstood by the SPN without clinical symptoms making it more likely to be injured during surgery.
Our patient remained asymptomatic post operatively. We believe this to be the first English language report of an incarcerated SPN in a fibular fracture site. The unexpected finding of the nerve incarcerated in the fracture site emphasizes the fact the careful dissection should be employed in all operatively managed ankle fractures.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.