RESEARCH ARTICLE
Evaluation of an Image-Based Tool to Examine the Effect of Fracture Alignment and Joint Congruency on Outcomes after Wrist Fracture
Emily A Lalone 1, 2, Ruby Grewal 1, 3, Graham W King 1, 3, Joy C MacDermid*, 1, 2, 3
Article Information
Identifiers and Pagination:
Year: 2015Volume: 9
First Page: 168
Last Page: 178
Publisher ID: TOORTHJ-9-168
DOI: 10.2174/1874325001509010168
Article History:
Received Date: 23/11/2014Revision Received Date: 7/2/2015
Acceptance Date: 19/2/2015
Electronic publication date: 15/5/2015
Collection year: 2015

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Some mal-alignment of the wrist occurs in up to 71% of patients following a distal radius fracture. A multiple case study was used to provide proof of principle of an image-based technique to investigate the evolution and impact of post-traumatic joint changes at the distal radioulnar joint. Participants who had a unilateral distal radius fracture who previously participated in a prospective study were recruited from a single tertiary hand center. Long term follow-up measures of pain, disability, range of motion and radiographic alignment were obtained and compared to joint congruency measures. The inter-bone distance, a measure of joint congruency was quantified from reconstructed CT bone models of the distal radius and ulna and the clinical outcome was quantified using the patient rated wrist evaluation. In all four cases, acceptable post-reduction alignment and minimal pain/disability at 1-year suggested good clinical outcomes. However, 10 years following injury, 3 out of 4 patients had radiographic signs of degenerative changes occurring in their injured wrist (distal radioulnar joint/radio-carpal joint). Proximity maps displaying inter-bone distances showed asymmetrical congruency between wrists in these three patients. The 10-year PRWE (patient rated wrist evaluation) varied from 4 to 60, with 3 reporting minimal pain/disability and one experiencing high pain/disability. These illustrative cases demonstrate long-term joint damage post-fracture is common and occurs despite positive short-term clinical outcomes. Imaging and functional outcomes are not necessarily correlated. A novel congruency measure provides an indicator of the overall impact of joint mal-alignment that can be used to determine predictors of post-traumatic arthritis and is viable for clinical or large cohort studies.
INTRODUCTION
Distal radius fractures (DRF) are a common orthopedic injury accounting for more than 44% of all upper extremity fractures in the United States in 2001, and it has been estimated that hand and wrist fractures accounted for 1.5% of all visits to the emergency room [1]. Residual deformity in the form of joint mal-alignment occurs when anatomic reduction is not achieved following treatment. Some mal-alignment of the distal radioulnar and radio-carpal joint has been estimated to occur in up to 71% of patients following a DRF [2]. Controversy exists however surrounding the extent to which residual deformity contributes to pain and disability [3, 4]. Much of the current research has focused on the association of these radiographic measures of deformity with functional and patient reported outcomes and has highlighted particular radiographic parameters that significantly correlated and predicted future function. However other studies have shown that acceptable radiographic reduction of the distal radius was not associated with greater health status,lower disability or greater satisfaction [5] nor was there a significant relationship found between residual deformity and patient reported outcomes of pain and disability [6].
Previous studies however have determined the predictive value of radiographic measures in identifying patients that are most likely to develop Osteoarthritis [7-10]. The results of these previous studies emphasize the importance of accurate reduction of the joint in preventing the development of Osteoarthritis. Residual deformity of the joint may affect loading mechanics that can contribute to development of post-traumatic arthritis as well as increase the risk for chronic pain and disability. Planar x-rays however, although used extensively in the treatment and monitoring of distal radius fractures clinically, by their very nature, are limited in their view as they project a 3D structure to a 2D plane requiring lateral and poster-anterior views for analysis. This can make it difficult to perceive details of complex bone fractures as they appear overlapped. Additionally, from these 2D projections, the 3D alignment is reduced even further into single radiographic parameters of inclination, angulation and length which may or may not reflect the actual deformity (i.e. fracture could have translated volarly or dorsally or rotated internally or externally). The difficulty is that deformities do not necessarily occur in single planes and are often not in isolation. Combined deformities of the distal radius are significant in determining clinical outcomes [11]. Additionally, 2D radiographic measures are not able to determine the overall effect the distal radius deformity has on the resulting joint mechanics. We have therefore developed a CT- based joint congruency algorithm [12] to assess the effect of residual deformity on resulting joint mechanics and to reflect the overall alignment of a joint. We suspect that joint congruency may play a role in the development of post-traumatic arthritis and may contribute to increased pain and disability. Using a multiple case study design, the purpose of this study was to evaluate a novel image-based approach as a tool to indicate 3D joint congruency of the distal radioulnar joint in uninjured and injured wrists and determine its impact on clinical status in the long-term follow-up of a distal radius fracture.
MATERIALS AND METHODOLOGY
Patients who had previously participated in a prospective study where baseline and standardized follow-up was performed for the year were contacted to participate in this long term follow-up study. Forty-eight patients who were eligible to participate (inclusion criteria: unilateral DRF, previous participation in a prospective study, had no contraindications for CT) were contacted and four (female) participants agreed to return to the clinic for a long term follow-up (September 2013-January 2014). The original baseline measures included radiographs and self-reported measures of pain and disability and health status with impairments in grip strength, range of motion (ROM) and dexterity. Eligible cases that consented agreed to evaluation by an orthopedic surgeon, computed tomography (CT) scans of both wrists as well as bilateral posterior-anterior and lateral wrist radiographs. Patients were re-tested during this long term follow-up visit (≤10 years) using the same battery of tests completed at the time of injury. The study protocol was approved by ethics review board of our institute and hospital and complied with the Declaration of Helsinki of 1975, revised 2000.
Patient Reported Outcomes
The primary clinical outcome measure was pain and disability which was quantified using the Patient Rated Wrist Evaluation (PRWE) which is a 15-item patient-reported outcome measure that has been shown to be reliable and highly responsive in the distal radius fracture population [3, 13, 14]. The PRWE allows patients to rate their levels of wrist pain and disability during a variety of activities of daily living for a total possible score of 100 (0=best possible score, 100=worst possible score). In 1 case, one data point was not available for baseline PRWE scores and this score was calculated using multiple imputations (regression method).
Radiographic Assessment
Pre-reduction, post-treatment and short-term follow-up (mean: 20 months) radiographs were retrieved for each patient. Repeat radiographs of both the uninjured and injured wrist were obtained at their long term follow-up visit (mean follow-up 9.4 years).
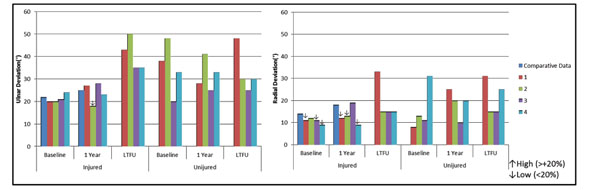
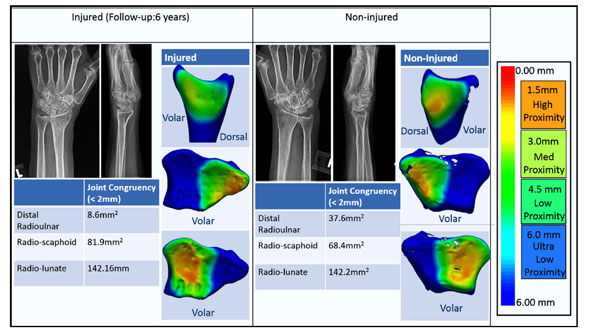
For short term and long term follow-up radiographs, radial inclination, ulnar shortening and volar tilt were measured using a digital goniometer. All measurements were performed according to a standardized process [15] and are shown in Fig. (1). Overall radiographic alignment was designated as unacceptable if the volar tilt was >20° or dorsal tilt >10°, if the radial inclination was <15° or if there was ≥3 mm of ulnar positive variance using the guidelines written by the American Society for Surgery of the Hand (ASSH) as well as by previous studies [5]. Radiographic evidence of osteoarthritis in the radio-carpal and distal radioulnar joint was assessed by grading the long term follow-up radiographs using the Kellgren and Lawrence Grading system [16]. Using this scale osteo-arthrosis is divided into five grades (0-None, 1-Doubtful, 2- Minimal, 3- Moderate, 4- Severe). Grades were indicated based on the presence of joint space narrowing, osteophytes, sclerosis and deformity of bone ends. A grade of greater than 0 indicated that this patient had radiographic signs of Osteoarthritis. Additionally, fractures as shown in the pre-treatment and post-treatment films were classified using the AO classification system.
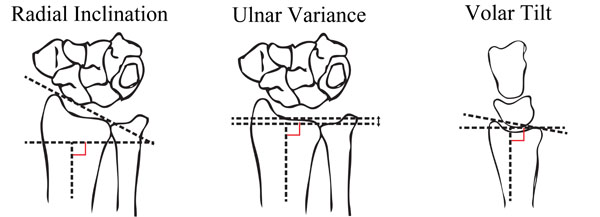 |
Fig. (1). Radiographic measures. |
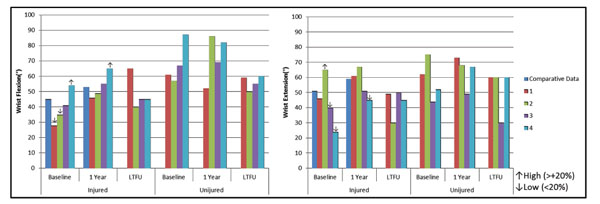 |
Fig. (2B). Range of motion: wrist flexion/extension. |
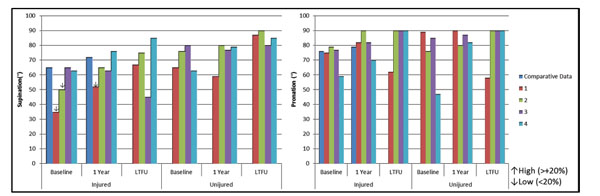 |
Fig. (2C). Range of motion: wrist supination/pronation. |
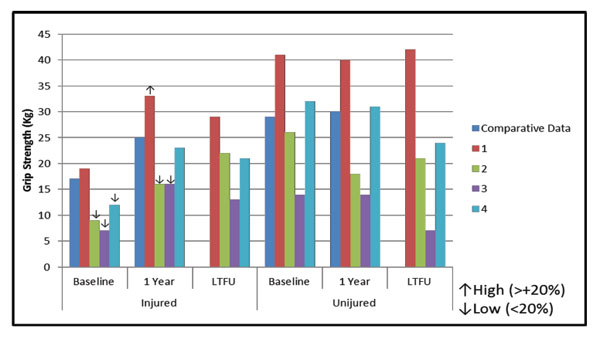 |
Fig. (2D). Grip strength. |
Impairment Testing
Grip strength was also assessed at the long term follow-up visit using the NK digit-grip device to reliably measure static pain-free grip strength scores [17]. Ranges of motion (ROM) measures were taken on both the injured and uninjured wrist using a goniometer. Range of motion measurements included radial and ulnar deviation, wrist flexion and extension and pronation and supination.
CT Scanning
Bilateral CT scans were obtained solely at the long term follow-up visit using a 64-slice scanner (GE Discovery CT750 HD, Waukesha, WI). Approximately 200 slices were acquired for each patient in the supine position with the patients arm extended 180° over their head and their wrists fully pronated (slice thickness=0.625mm, pixel spacing approximately 0.4 x 0.4mm, 50mA, 120 kVp).
Joint Congruency
To investigate relative joint inter-bone distances and overall joint congruency of the distal radioulnar joint (DRUJ) and radiocarpal joints (radioscaphoid and radiolunate joints), an inter-bone distance algorithm was employed [12]. This technique was originally developed for use in an in vitro biomechanical testing laboratory and its accuracy was previously described and assessed using a gold standard experimental silicone casting technique [18]. The DICOM data (Digital Imaging and Communications in Medicine) obtained from the CT scan were imported into Mimics 14.12 (Materialise, Leuven, Belgium). Reconstructions were created using a threshold-based semi-automatic segmentation with a threshold which was selected and verified by viewing the 2D slice data overlaid with the reconstructed 3D bone to ensure that the threshold selected accurately traced the corresponding bone/soft tissue boundary. Once the 3D reconstructions had be generated, a custom software was used to manually segment the articulating regions of the distal radius, and distal ulna and saved separately. These regions on the distal radius included the sigmoid notch and the scaphoid and lunate fossa. The entire scaphoid and lunate were included in the measurements. Joint congruency was measured using an inter-bone distance algorithm which has been described in detail previously [12]. Briefly, the algorithm calculates minimum inter-bone distances between opposing bone surfaces using a point-to-point distance measurement. These measurements were taken using the vertices of the surface mesh as points and represent the 3D joint space which is a measure of congruent/close the opposing surfaces are to one another. Inter-bone distances are displayed using a colored proximity contour map (0mm=red, 6mm=blue). High proximity was characterized in this study as having an inter-bone distances less than 2.0mm and corresponded to the yellow-green transition on the colored proximity map and the surface area on the radius or ulna that had an inter-bone distance less than 2.0mm was quantified and was termed ‘inferred close contact region’. This region is called inferred contact region as it does not consider cartilage thickness. The surface area is reported for the long term follow-up CT scans for the injured and non-injured. Additionally, the overall % of the surface area that is in the inferred contact region was calculated for the distal radioulnar joint. The total surface area of the subchondral region was determined by manually segmenting the subchondral region of the 3D bone model reconstruction. The surface of the 3D bone model itself is a tesslated surface composed of triangles. The surface area of each triangle within the manually segmented region was measured and the total surface area of the entire subchondral surface was then determined. The % surface area therefore is the surface area within the inferred contact region divided by the total surface area of the subchondral region.
Comparative Data
Comparative scores for grip strength, PRWE, ROM and grip strength were acquired using a previous study which assessed these measures in 275 patients who have had a distal radius fracture at the following time points; baseline, 3 months, 6 months and 1 year [3, 4]. The mean values reported in this previous study define ‘average’ values for patient’s status and were used in this current multiple case series to rank patients experienced pain and disability (PRWE) as being average, high (Patient Score Average Score +20%) or as having low pain and disability (Patient Score≤ Average Score -20%) as measured on a particular time point (Table 1) [4]. Similarly patients were considered to have low ROM if their scores were 20% less than average or considered to have high ROM values if their scores were 20% higher than reported averages.
Demographic and Patient Rated Wrist Evaluation Scores at Baseline, One Year following injury and at Long Term Follow-up. PRWE scores are shown for four illustrative cases and compared against cohort values published previously to rank patients pain and disability (+/- 20%).
| Baseline | 1 year | Long Term Follow-up | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PRWE | PRWE | PRWE | ||||||||||||
| Case | Gender | Age at Injury | Age at LTFU | Dominant Hand |
Injured Wrist | Treatment | AO | Average Cohort Score (75) | Pain and Disability Ranking |
Average Cohort Score (15) |
Pain And Disability Ranking |
|||
| 1 | F | 40 | 52 | R | L | External Fixation plus Pins | A | 62 | -20% | low | 1 | -187% | low | 8 |
| 2 | F | 60 | 71 | R | L | Open Reduction Internal Fixation(dorsal plate-hardware removed) |
C | 88 | +16% | average | 15 | 0% | average | 12 |
| 3 | F | 48 | 57 | R | R | Pins | B | 69 | -9% | average | 15 | 0% | average | 4 |
| 4 | F | 65 | 71 | R | L | External Fixation plus Pins | C2 | 85 | +12% | average | 0 | -200% | low | 60 |
Unacceptable Parameters: (ASSH guidelines).
RI: Radial Inclination<15°.
DA: Dorsal Angulation >10° Dorsal Tilt(-), >20° Volar Tilt (+).
UV: Ulnar Variance ≥3mm.
Radiographic Measures taken at Short-term Follow-up (mean: 20 months) and Long Term follow-up (mean: 113 months). Radial Inclination (RI), Dorsal Angulation (volar +, dorsal -) (DI), Ulnar Variance (mm)-measured at the height of the distal radio-ulnar articulation (UV).
| Short Term Follow-up | Long-Term Follow-Up (Injured Wrist) |
Long-Term Follow-Up (Non-Injured Wrist) |
KL OA Scale | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RI | DA | UV | RI | DA | UV | RI | DA | UV | Injured | Uninjured | |||
| Case | Radiocarpal | DRUJ | Radiocarpal | DRUJ | |||||||||
| 1 | offline | offline | offline | 20.7 | 3.1 | 1.05 | 20.4 | 9.92 | 1.57 | Grade 0 | Grade 0 | Grade 0 | Grade 0 |
| 2 | 17.3 | 17.2 | 2.48 | 20.1 | 14.5 | 2.32 | 29.5 | 13.6 | 0 | Grade 1 | Grade 1 | Grade 0 | Grade 0 |
| 3 | 36.7 | 8.2 | 0 | 38.9 | 8.6 | 0.92 | 29.3 | 12.5 | 0 | Grade 1 | Grade 2 | Grade 1 | Grade 0 |
| 4 | 21.2 | -2 | 1.88 | 22.3 | -2.6 | 1.06 | 22.8 | -0.2 | 0.61 | Grade 1 | Grade 0 | Grade 0 | Grade 0 |
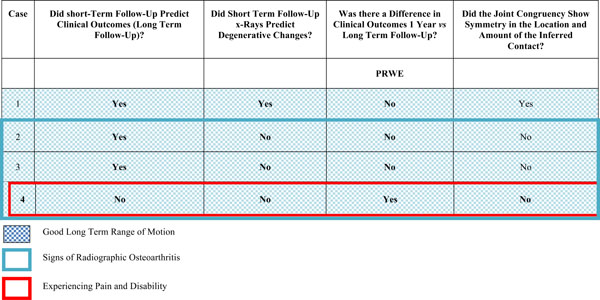
Predictive values of short-term follow-up X-rays in predicting clinical outcomes and degenerative changes and joint congruency measures. At short-term follow-up, radiographs in all four cases indicate that fracture reduction has healed in good alignment and patients are experiencing low or average pain and disability. However, in three out of four cases, these patients developed degenerative changes seen in their injured wrist. At long term follow-up all patients had good range of motion, but one patient was experiencing high pain and disability. Proximity maps indicate deviations in the overall joint congruency between the injured and non-injured wrist of patients (symmetry of inferred contact) who have degenerative changes seen approximately 10 years later post fracture injury. This suggests that patients may need to be instructed that even mild mal-alignment can result in post-traumatic arthritis, but that it is possible that they will be symptom free in the longer term.
 |
Analysis
A descriptive analysis was used to describe how initial injury parameters and post reduction mal-alignment were related to long term joint status; and the relationship between joint congruency and symptoms reported and the role of the CT analysis in defining these.
RESULTS
Four patients who were eligible to participate in the study agreed to come into the clinic for follow-up. Table 1 lists the demographic data for these cases (gender, age at injury, age at long term follow-up visit, hand dominance, injured wrist, treatment and AO fracture classification) as well as their baseline, 1 year and long term follow-up scores for the PRWE. Table 2 describes the radiographic measures for the short term, long term follow-up (for the injured and non-injured wrist) as well as their Kellgren Lawrence Osteoarthritis Scale. Table 3 is a summary chart which compares the radiographic measures measured at the short term follow-up visit and uses these values (acceptable or unacceptable) to predict long term clinical outcome, and long term degenerative changes(as defined by a grade of greater than 0 on the Kellgren Lawrence OA scale). As well, this table summarizes the differences in clinical outcomes between 1 year and 10 years and examines the symmetry of the joint congruency proximity maps.
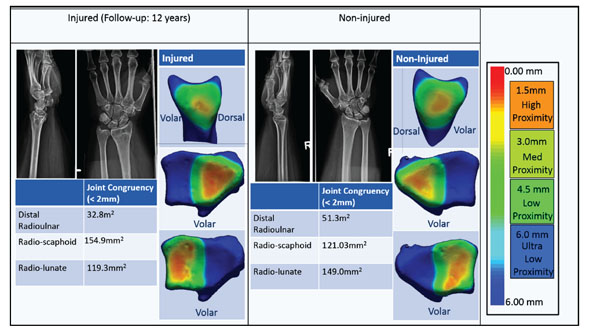
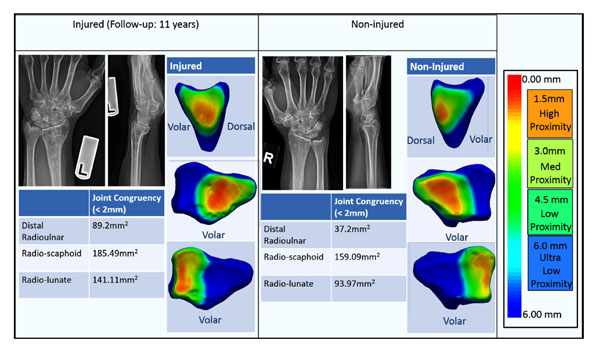
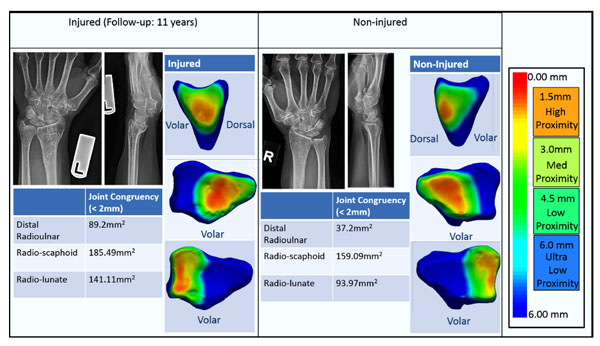
Fig. (2A-D) shows the ROM and grip strength scores for these four cases at baseline, 1 year and during their long term follow-up visit and include comparative data scores for these measures. Fig. (3A-D) shows the proximity maps for the long term follow-up CT scans of the injured and non-injured wrists for all cases as well as the radiographs (posterior-anterior and lateral) of the short term follow-up and long term follow-up for each case.
CASE 1
A 40 year old woman sustained an extra-articular fracture of her left distal radius which was treated with external fixation and percutaneous pins. Long-term bilateral CT scans were acquired of the injured and non-injured wrist (12 years post injury).
Fig. (3A) shows the proximity maps of both wrists showing a 3D view of the joint relative inter-bone distances. Proximity maps are shown on the distal radius but corresponding distal ulna, scaphoid and lunate maps were also created. Distal radioulnar joint congruency (as shown on the proximity maps) was similar in both wrist joints and proximity maps appear symmetric. Inferred high contact regions (shown in yellow) on the injured wrist had a reduced surface area (14.3% of the overall surface area) on the distal radius compared to the non-injured side (20.0% of the overall surface area) indicating that the injured wrist is less reduced at the DRUJ compared to the non-injured wrist. Radio-scaphoid and radio-lunate joint congruency has similar locations for the high contacting regions when comparing the injured and non-injured wrists. The surface area on the injured scaphoid fossa appears to be in high proximity (red-orange colors) when compared to the non-injured wrist.
At baseline her PRWE score (62) was considered to be low compared to the average baseline PRWE previously reported [4]. At one year this patient was reporting almost no pain and disability (PRWE:1) and at approximately 12 years post-fracture she has a PRWE score of 8 suggesting minimal pain and disability (Table 1). At her long term follow-up this patient had evidence of persistent loss in hand strength indicated by her having 69% of her contralateral grip strength (increased from 46% at baseline and 83% at 1 year). Fig. (2A-D) shows full range of motion recovery for both her wrists. Short-term, post definitive treatment radiographs were not available for viewing (> 10 years old) however radiological reports indicate that the fracture was positioned in near anatomical alignment and healed in neutral alignment. Bilateral Long-term follow-up radiographs acquired 12 years following injury are shown in Fig. (3A). Radiographs indicate mild deformity of the injured distal radius with the angulation of the distal radius appearing more neutral in the lateral plane (volar tilt: injured: 3.1°, non-injured: 9.92°) (Table 2). However, radiographic parameters are within normal ranges and are considered acceptable by the ASSH standards. Three-dimensional reconstructions as shown in Fig. (3A) further reveal this loss of volar tilt. The Kellgren-Lawrence OA grade was 0 for both the radio-carpal and distal radioulnar joint on the injured and non-injured wrist indicating a lack of post-traumatic arthritis (Table 2).
CASE 2
A 60 year old female fell on her left wrist and suffered an intra-articular distal radius fracture that was treated with open reduction and internal fixation. Hardware was removed from the distal radius approximately 3 years later.
Long-term radioulnar joint congruency (11 years following injury) is not symmetric between the injured and non-injured wrist (Fig. 3B). Inferred high contact regions on the injured wrist revealed an increased surface area (27.7% of the overall surface area) and more central location on the distal radius compared to the non-injured side (16.9% of the overall surface area) indicating that the injured wrist is more reduced at the DRUJ compared to the non-injured wrist. Radio-scaphoid and radio-lunate joint congruency are also not symmetric in the amount (surface area) of the high contacting regions when comparing the injured and non-injured wrists although the location is similar.
At baseline, this patient had average amounts of baseline pain and disability (PRWE: 88) but had a PRWE score which was 13 points higher than the cohort comparison. However, by 1 year, her pain and disability scores decreased and fell within the average range (PRWE: 15). Approxi-mately 11 years later, this patient’s PRWE score was 12 having decreased 3 points from her 1 year score (Table 1). Overall at her long term follow-up visit, this patient was considered to have average amount of pain and disability. This patient’s ROM at 1 year showed a deficit in radial and ulnar deviation however, these values were restored compared to the non-injured side approximately 11 years later (Fig. 2B). Radiographically, this patient had a moderately distorted distal radius (Table 2, Fig. 3B). Her short-term follow-up radiographs indicate that she has healed in a slightly ulnar positive (+2.48mm) position (non-injured wrist: 0mm), but falls within the acceptable range for ulnar variance. Eleven years later, she remains in this slightly ulnar positive alignment. Her other radiographic characteristics are similar to her contralateral side (long term follow-up x-ray) and are also within the acceptable range. Based on x-ray, the Kellgren-Lawrence OA grade was 1 for the distal radioulnar joint grade 1 for the radio-carpal joint on the injured with no degenerative changes seen on the non-injured wrist (Table 2).
CASE 3
A 48 year old woman fell on her right wrist and suffered from a partial articular fracture which was treated using percutaneous pins.
Long-term radioulnar joint congruency (9 years following injury) was not symmetric between the injured and non-injured wrist as shown on the proximity maps (Figure 3C). Inferred high contact regions on the injured wrist revealed a decreased surface area (10.7% of the overall surface area) on the distal radius compared to the non-injured side (16.6% of the overall surface area) indicating that the injured wrist is less reduced at the DRUJ compared to the non-injured wrist. The articular surface of the injured distal radius is irregular and can be seen in the 3D reconstruction. This irregularity in the surface morphology is also seen in the scaphoid and lunate fossa of the distal radius resulting in a non-symmetric and irregular joint congruency pattern in the injured wrist.
Her baseline PRWE (69) scores indicated that she had average symptoms compared to the average patient with a DRF at baseline and continued to have average symptoms 1 year following treatment(PRWE: 15). Approximately 9 years later (PRWE: 4) she is still within the average range of PRWE scores (Table 1). This patient’s ROM was excellent and continued to be at her long term follow-up visit with the exception of a 35° reduction in supination on her injured wrist (Fig. 2C). Radiographically this patient had high radial inclination at baseline and healed in this alignment as seen in long term follow-up radiographs and appears to be approximately 10° more inclined than the non-injured wrist (but still in the acceptable range according to ASSH standards) (Table 2, Fig. 3C). Volar tilt was restored as well as ulnar variance. The Kellgren-Lawrence OA grade was 2 for the distal radioulnar joint and grade 1 on the radio-carpal joint on the injured with no degenerative changes seen on the non-injured wrist distal radioulnar joint and grade 1 on the radio-carpal joint.
CASE 4
A 64 year old woman fell on her left wrist and suffered from a full articular fracture which was treated with external fixation and percutaneous pins.
Long-term radioulnar joint congruency (6 years following injury) was not symmetric between the injured and non-injured wrist as shown on the proximity maps (Figure 3C). Inferred high contact regions on the injured wrist revealed a decreased surface area (3.5% of the overall surface area) on the distal radius compared to the non-injured side (16.8% of the overall surface area) indicating that the injured wrist is less reduced at the DRUJ compared to the non-injured wrist (Figure 3D). This region of high contact area is also located more distal-central in the uninjured wrist. . Radio-scaphoid and radio-lunate joint congruency has similar locations for the high contacting regions when comparing the injured and non-injured wrists as well as similar amounts of inferred high contacting regions. There are some pitting and irregularities in the surface morphology of the scaphoid and lunate fossa which is consistent with some degenerative changes in the wrist articulation.
Her baseline PRWE scores (85) indicated that average amounts of pain and disability at baseline but was experiencing no pain/disability 1 year following injury (PRWE: 0). Approximately 6 years later she had very high pain and disability (a score of 100 is the worst possible pain and disability) (PRWE: 60). At 1 year following injury this patient had reduced radial deviation (70%), wrist extension (28%) and decreased grip strength of 74% compared to her non-injured side. At her long term follow-up visit she had reduced wrist flexion and extension however her grip strength had increased to 88%. Radiographically this patient had acceptable radiographic parameters at baseline, following treatment and at her short-term follow-up (according the ASSH standards) (Table 2, Fig. 3D). However, radiographs show a loss of volar tilt following treatment (Fig. 3D). At her long term follow-up this patient appears to be in almost neutral alignment in the sagittal plane with slight dorsal tilt of the distal radius. Her non-injured wrist also appears to be in the neutral alignment in the sagittal plane (Fig. 3D). The Kellgren-Lawrence OA was grade 1 on the radio-carpal joint on the injured with no degenerative changes seen on the distal radioulnar joint with no degenerative changes in the non-injured wrist (radio-carpal/DRUJ). Although not graded, this patient does have mid-carpal degenerative changes occurring in her non-injured wrist.
DISCUSSION
An increased incidence of arthritis at the DRUJ has been reported with healed mal-aligned distal radius fractures [19]. Three dimensional modeling of joints obtained from CT imaging can potentially help us better understand the pathomechanics which are thought to occur following joint trauma, the potential disruption in joint contact mechanics and the eventual development of arthritis. This series demonstrates the clinical application of a 3D joint congruency algorithm recently developed through in vitro biomechanical studies. This current study employs this algorithm to examine 3D joint space and alignment of patients who have previously suffered from a unilateral distal radius fracture in a long term follow-up study. A multiple case study is an appropriate approach to provide proof of principle of this technique and to explore, at an individual level, the way that joint changes evolve over a long interval. These illustrative cases show what information can be gained from using proximity mapping that enhances our understanding of factors potentially leading to the development of post-traumatic arthritis. This is also the first study in which the application of this previously developed joint congruency algorithm has been applied to the radiocarpal joints. This study also examined pain and disability, range of motion and grip strength longitudinally to examine the symptomatic side effects, if present, in patients who have suffered from a distal radius fracture 10 years previously and to examine these measures over time.
What Happens to Well Aligned Distal Radius Fractures in the Long Term?
These cases illustrate a range of short and long term outcomes and suggest that currently defined levels of ‘acceptable reduction’ and radiographic parameters used to monitor fracture alignment may not capture patients at risk of developing post-traumatic arthritis over the long term. Table 3 compares radiographic values from short-term follow-up x-rays and long term clinical outcomes and relates these measures to degenerative changes that have occurred approximately 10 years following injury. In all four cases, acceptable post-reduction radiographic was achieved based on current standards for acceptable range. This was associated with good outcomes in self-reported pain and disability as well as ROM. Even with slight irregularities, (Case 1: loss of volar tilt, Case 2: ulnar positive alignment, Case 3: high radial inclination, Case 4: loss of volar tilt) 3 out of 4 patients were experiencing little pain and disability and have good function approx. 10 years following injury. However, 10 years following injury, 3 out of 4 these patients have some signs of radiographic degenerative changes occurring either in the radio-carpal or DRUJ of their injured wrist which was not present on their injured side. Three out of four patients had some degenerative changes in the radiocarpal joint in the injured wrist (one patient had degenerative changes bilaterally). This warrants further investigation into the effects of distal radius fractures on the surrounding joint mechanics (radiocarpal, midcarpal) as these articulations are highly integrated within the wrist joint.
The long-term prospective follow-up and lack of arthritis on the non-injured side allows us to attribute the arthritis to the initial injury although further investigation in a larger sample is necessary to examine this causative and associative relationships. However, in this pilot study, given that 1 of 4 cases had symptoms of pain, limited range of motion and weakness perhaps consistent with arthritis, and given that follow-up imaging and clinical findings were not consistently associated, a long-term quantitative study with high quality imaging is needed to define rates and predictors. This indicates that perhaps good 1-year outcomes cannot be considered ‘protective’ against future post-traumatic arthritis.
What Information Can Be Gained from Using Proximity Mapping that Enhances Our Understanding of the Development of Degenerative Changes?
Joint congruency was measured using CT reconstructions of the non-injured and injured distal radius and ulna, scaphoid and luante. In all patients who have developed degenerative changes in the injured wrists, the overall proximity map appears asymmetrical in both the location and size of the surface area in high proximity (orange-yellow). These proximity maps reveal a departure from the non-injured wrist alignment which could potentially explain why these patients develop degenerative changes approximately 10 years following injury. Previous studies have noted that changes in joint alignment and therefore contact mechanics may have deleterious effects on articular cartilage [20, 21].
Standard planar radiographs are used extensively clinically as visibility of fracture fragments can be readily seen in the majority of cases and currently help to guide clinical decision making. Planar radiographs however can only be interpreted on the basis of 2D indictors. Conversely, using 3D CT, deformities can be visualized in three-dimensions and using reconstructions, the implications of these deformities on the surroundings joints can be fully appreciated. Proximity mapping as shown in this study allows the viewer to gain additional information regarding 3D joint space and overall joint congruency which can, as shown in these illustrative cases in this study, provide information about potential degenerative changes that might occur following residual deformity.
This pilot study was limited in the number of patients examined but did provide justification for a large cohort study to be performed using this technique. This was also the first application of the previously developed inter-bone distance technique to the radiocarpal joints and also to compare these biomechanical indicators of joint morphology with clinical outcomes. Future work is needed to examine associative and correlative properties of these joint congruency measurements (DRUJ and radio-carpal joint alignment) with patient outcomes in a larger cohort of patients to ultimately develop biomechanical algorithms to establish a safe zone for fracture alignment following distal radius fracture.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the assistance of Gloria Watson for organizing patients’ clinical visits and scanning appointments. Thank you also to Joshua Vincent and Kate Kelly for their assistance in patient reported and functional outcome measures. We would like to acknowledge the Canadian Institutes of Health Research for their financial support (FRN: 122070).