All published articles of this journal are available on ScienceDirect.
Complications and Predictors of Need for Return to the Operating Room in the Treatment of Supracondylar Humerus Fractures in Children
Abstract
Supracondylar humerus fractures are common pediatric injuries. Little is known about the risk factors for repeat operative procedures. A retrospective chart review of 709 patients treated for a displaced supracondylar humerus fracture was performed to identify risk factors for return to the operating room during the initial post-operative period. Deviations of routine fracture care were recorded and complication rates were compared between Gartland type 2 and 3 fractures using logistic regression. Type 3 fractures were found to have a higher complication rate, and, specifically, more peri-operative nerve palsies, more likely to need to return to the operating room for hardware removal, to lose fracture reduction, and require a return to the operating room for any reason. Five risk factors which may require returning to the operating room were identified: younger patient age, left sided fractures, type 3 fractures, peri-operative nerve palsy, and post-operative infection. In conclusion, Gartland type 3 supracondylar humerus fractures are associated with more complications then type 2 fractures. Risk factors for the need to return to the operating room in the post-operative period include: younger patient age, left sided fractures, type 3 fractures, peri-operative nerve palsy, and post-operative infection. Patients with these risk factors should be considered at risk for return to the OR and fracture fixation and follow up protocols should be adjusted for this risk.
Level of Evidence :
Prognostic Study, Level II.
INTRODUCTION
Supracondylar humerus fractures are a common injury in skeletally immature individuals, accounting for the majority of elbow fractures in children [1]. In recent years there has been a trend towards more aggressive treatment of these fractures with some advocating surgical management of all Gartland type 2 and 3 fractures, based on low complications rates and improved radiographic outcome after surgical treatment [2-4]. Multiples studies have documented relatively low complication rates, between 2-8%, with surgical treatment of supracondylar humerus fractures, most commonly consist-ing of pin migration under the skin, pin tract infection, and loss of fracture reduction [2, 5-8]. Despite the relatively low complication rate overall, some supracondylar humerus frac-tures do require repeat operative procedures early in the post operative period; however, risk factors for these repeat procedures are largely unknown. Sankar and colleagues reported technical errors in pin placement in type 3 fractures which were associated with those fractures in which loss of fixation was identified, but the contribution of patient, fracture, and injury factors to the need for repeat surgery has not been investigated [9].
The intention of this study was to present a large series of operatively treated supracondylar humerus fractures at a single institution to evaluate the predictors of return to theOR after operative treatment of supracondylar humerus fractures.
METHODS
A retrospective chart and radiograph review was performed on all patients who underwent operative fixation of a supracondylar humerus fracture between January 2006 and December 2010 at our institution. During this time period 752 patients were treated for fixation of a displaced Gartland type 2 or 3 supracondylar humerus fracture by one of eleven fellowship trained pediatric orthopaedic surgeons. All of those patients included in the study had a minimum of 6 weeks follow up and were followed until fracture healing and pin removal. All patients underwent attempted closed reduction and percutaneous pinning of the fracture in the operating room with the pins left out of the skin. No patients had pins intentionally buried underneath the skin during their initial procedure. If a satisfactory closed reduction was unable to be obtained, the fracture was reduced by open reduction and fixed with percutaneous pins by the treating physician. All patients had the entire limb prepped with chlorhexidine gluconate, iodine povacrylex/isopropyl alcohol, or betadine (at the discretion of the treating physician) and the entire extremity was sterilely draped. The base of the c-arm or an arm table was used as the operative field (at the discretion of the treating physician). Peri-operative antibiotics were used at the discretion of the treating physician. All patients were seen within 2 weeks of the initial surgery and then again within 6 weeks of the surgery (defined as the initial post-operative period). Radiographs were taken at each follow up visit and the pins were removed in the clinic when radiographic healing of the fracture was deemed adequate by the treating physician. Patients with pins that migrated underneath the skin during the post-operative period and were unable to be removed in the clinic were taken back to the operating room for removal of pins under anesthesia.
Of the initial 752 patients, 43 were excluded. Exclusion criteria were those patients who did not return to our institution for a post operative visit (n=23), those patients who did not have complete medical records (missing follow up visit office notes, n=11), patients who underwent only closed reduction and casting in the operative room (n=1), and those patients with T-condylar extension of the supracondylar fracture (n=8). The study population consisted of 709 patients.
Information recorded during the chart review included age of the patient, side of fracture, pin construct used for fixation, whether the fracture was open, use of peri-operative antibiotics, occurrence of pin site or deep infection during the follow up period, presence of ipsilateral upper extremity fracture at the time of presentation, nerve injury at presentation or post-op, any return to the operative room during the initial post-op period, and loss of reduction. Need to return to the operative room and loss of reduction were defined by the treating physician and the reason for these complications was recorded based on the clinic notes from the treating physician. The reasons for needing to return to the operating room in the initial post-operative period included loss of fracture reduction or need for implant removal in the operative room.
Deviations of routine fracture care was defined as both complications associated with the surgical management of the fracture (pin tract or deep wound infection, post-op nerve palsies, need to return to the operating room for removal of buried pins, and loss of reduction of the fracture as indicated by the treating physician in their office notes) and complications associated with the injury (presence of an open fracture, presence of an ipsilateral fracture, and pre-op nerve palsies).
Categorical data were compared for type 2 and type 3 fractures using either the Fisher’s exact test or Chi squared analysis. Multivariate stepwise logistic regression analysis was used to determine the association of patient variables, fixation variables, and deviations of routine fracture care with need to return to the operating room in the initial post-operative period for any reason. Significance for the comparative statistics as well as the inclusion of a variable in the logistic regression model was defined as p<0.05.
IRB approval was obtained for this study. No external source of funding was obtained for this study.
RESULTS
Of the 709 supracondylar fractures evaluated, 264 were Gartland type 2 and 445 were Gartland type 3 fractures. The percentage of patients with right sided injuries in the two groups was the same. The patients with type 2 fractures were younger and less likely to be treated with a medial pin (Table 1).
Demographic and treatment data.
| Type 2 | Type 3 | P Value | |
|---|---|---|---|
| # right sided injury | 113 (42%) | 189 (42%) | 0.912 |
| Age (yrs) | 4.84 | 5.76 | <0.0001 |
| # with medial pin | 19 (7.2%) | 118 (26%) | <0.0001 |
Complications associated with type 2 and type 3 fractures.
| Type 2 (n=264) |
Type 3 (n=445) |
P Value | |
|---|---|---|---|
| Open Fracture | 0 | 4 | 0.303 |
| Infection | 0 | 3 | 0.298 |
| Ipsilateral Fracture | 10 | 20 | 0.651 |
| Nerve Palsy | 4 | 54 | <0.0001 |
| ROH in OR | 1 | 10 | 0.05 |
| Loss of Reduction | 1 | 18 | 0.003 |
| Return to OR | 2 | 26 | 0.001 |
| Patients with a complication | 15 | 88 | <0.0001 |
Results of logistic regression for need to return to operating room for any reason
| Variable | Odds Ratio |
95% Confidence Interval |
P Value |
|---|---|---|---|
| Age (per 1 yr increase) | 0.73 | 0.5977 - 0.8827 | 0.0013 |
| Right sided fracture | 0.28 | 0.1043 - 0.7440 | 0.0108 |
| Type 2 fracture | 0.12 | 0.0270 - 0.5204 | 0.0047 |
| Nerve Palsy | 4.47 | 1.6677 - 11.9593 | 0.0029 |
| Infection | 36.20 | 2.3620 - 554.9983 | 0.0100 |
In comparing type 2 and 3 fractures, patients with type 3 fractures had more open fractures, post-operative infections, and ipsilateral forearm fractures, although these differences were not statistically significant due to the overall low incidence of these issues. (Table 2).
Patients with type 3 supracondylar fractures were found to have significantly more peri-operative nerve palsies, were more likely to need to return to the operating room for implant removal, to lose fracture reduction in the follow up period, as well as require a return to the operating room for any reason. A significantly higher percentage of patients with type 3 fractures were found to have at least one deviation of routine fracture care associated with their injury (Table 2).
Stepwise logistic regression identified five significant risk factors which may require returning to the operating room in the initial post-operative period after pinning of supracondylar humerus fractures: younger patient age, left sided fractures, type 3 fractures, presence of peri-operative nerve palsy, and post-operative infection (Table 3). Use of medial pins, lateral only pin constructs, presence of ipsilateral forearm fracture, and open fractures were not found to be significant variables for inclusion in the logistic regression model.
We further examined age as a risk factor which requirse return to the operating room. Due to our finding of age as a significant contributing variable in our logistic regression model of return to the operating room we attempted to find a specific age cut-off at which the risk of return to the OR increased. The frequency of return to the operating room was examined compared to age of patient. As can be seen in Fig. (1) the majority of patients who required return to the operating room were younger then age 8. A total of 28 patients required a return to the OR in the initial post-operative period, 26 of these patients were younger then 8 (4.5% of all patients < age 8), while only 2 were older than 8 years old (2% of all patients > age 8). Although more patients required return to the OR who were younger than age 8, there was no statistical difference in frequency of patients returning to the OR using a cut off age of 8 years old (p=0.41).
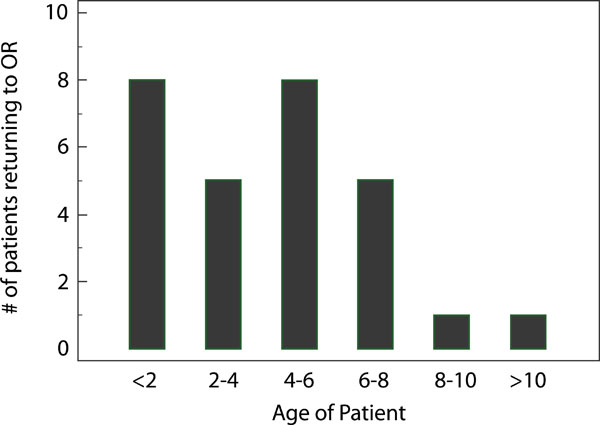
Total number of patients requiring return to the operating room for each patient age group.
DISCUSSION
Supracondylar humerus fractures are common injuries in children which often require operative fixation for optimal outcome [1, 3]. Previous studies have demonstrated relatively low rates of complications with surgical management of these fractures, leading some authors to suggest routine surgical management of these fractures presenting with any fracture displacement [2, 8]. Although need for repeat surgery in the early post operative period is rare, it is occasionally needed and currently there is no data on which factors may play a role in predicting fractures at risk for return to the operating room after initial surgical treatment.
As might be expected we found a significantly higher complication rate in Gartland type 3 fractures, with a significantly higher rate of nerve palsies, loss of fracture reduction, need for implant removal in the operating room, and need to return to the operating room in the initial follow up period. We speculate the higher energy of injury and the greater soft tissue disruption in type 3 fractures likely lead to less inherent fracture stability due to the increased periosteal disruption, more soft tissue trauma and swelling, and thus increased complications. We found a significant increase in the number of nerve palsies associated with Gartland type 3 fractures compared to type 2. The majority of these were nerve palsies identified pre-operatively in both groups. There were no post-operative nerve palsies in the type 2 group and three post-operative nerve palsies in the type 3 group. All of these post-operative nerve palsies were new ulnar nerve palsies associated with medial pins. Once the ulnar nerve palsy was identified, they were treated with immediate removal of the medial pin at the bedside with ultimate resolution of the ulnar nerve palsy. All of these patients had a secondary complication, in addition to the nerve palsy, leading to a return to the operating room with two of these patients requiring return to the operating room due to loss of fracture reduction and the other patient requiring a return to the operating room for removal of the remaining pins. None of the type 2 fractures with an associated nerve palsy required a return to the operating room.
In this study five factors were identified which were associated with an increased likelihood of need to return to the operating room. Specifically younger age of injury, type 3 fractures, and associated nerve palsies all were associated with need to return to the operating room. Patients with these factors should be considered as having “fractures at risk” and treating physicians should take extra precaution to avoid a need to return to the operating room, such as leaving pins longer outside the skin and closer follow up in the early post-operative period. As discussed above we postulate that type 3 fractures are associated with a higher energy of injury and more soft tissue injury and nerve palsies which may lead to less stable fracture fixation and more swelling in the post-operative period and this may lead to a higher incidence of need to return to the OR. Younger age of injury was also found to be a risk factor in need to return to the operating room. Due to the gradual ossification of the distal humerus, younger patients with a larger percentage of cartilaginous distal humerus may have less stable fixation with percutaneous pins leading to subsequent loss of fracture reduction. We were unable to determine an exact age at which the risk of return to the OR was decreased; however, the majority of patients requiring return to the OR were less then 8 years old. This apparent protective effect of increasing age has not been previously reported. Infection was also included as a significant variable in our logistic regression equation, however, the low number of total infections in our population (n=3 with only one requiring a return to the OR) limits our evaluation of this risk factor. Finally it is likely the inclusion of left sided fractures as a predictive variable was due to the higher overall percentage of left sided injuries in this cohort, thus making it more likely a patient with a left sided injury would need a return to the operating room.
The limitations of this study are its retrospective design. Due to the retrospective nature of the study we relied on the reporting of complications by the treating physician, thus introducing the possibility of under identification of complications. Additionally we did not review each radiograph to independently determine loss of fracture reduction in the follow up period. Variations in quality of post-operative radiographs can make assessment of fracture alignment and loss of fracture reduction difficult in supracondylar fractures. Due to this issue we chose to rely on the determination of the treating physician as to whether a patient required a return to the operating room due to loss of fracture reduction, a methodology used previously in the literature [9].
This large review of operatively treated supracondylar humerus fractures found Gartland type 2 fractures to be associated with a lower complication rate and decreased need to return to the operating room in the immediate post-operative period as compared to type 3 fractures. Additionally, we found type 3 fractures, fractures in younger patients, those associated with concomitant nerve palsies or infection to have an increased risk of need for return to the operating room. Treatment of patients with these risk factors may require additional pins for more secure fixation, extra length of pins left outside the skin to avoid need for removal of hardware in the operating room, more secure post-operative immobilization, or more frequent or earlier follow up in an attempt to avoid complications requiring a return to the operating room.
ETHICAL STANDARD
The authors declare they conformed with the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning Human and Animal Rights.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


