RESEARCH ARTICLE
Double Axis Cephalocondylic Fixation of Stable and Unstable Intertrochanteric Fractures: Early Results in 60 Cases with the Veronail System
Α. Kouzelis, A. Kravvas, S. Mylonas, D. Giannikas, A. Panagopoulos*
Article Information
Identifiers and Pagination:
Year: 2014Volume: 8
First Page: 60
Last Page: 68
Publisher ID: TOORTHJ-8-60
DOI: 10.2174/1874325001408010060
Article History:
Received Date: 5/9/2013Revision Received Date: 1/4/2014
Acceptance Date: 6/4/2014
Electronic publication date: 24/4/2014
Collection year: 2014

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.5/) which permits unrestrictive use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction:
This prospective case-series, without control group, study presents our early experience in the treatment of both stable and unstable peri-trochanteric fractures with a new cephalocondylic implant; the Veronail system.
Materials & Methods:
Enrolment in our study was from January 2008 through September 2009, with follow-up until October 2011 (at least 1 year). During this period 65 consecutively patients with a fracture in the trochanteric region of the femur (31.A1, A2 and A3 according to AO classification) were surgically managed and prospectively followed up for at least one year. Average age was 78 years old (range 42 to 93) with 40 female and 25 male patients. All patients were surgically treated using the Veronail system. Demographic and nursery data such as pre-existing illness, previous ambulatory status, type of anaesthesia, duration of surgery, volume of blood loss, transfusions, length of hospital stay, time to union and overall complications were systematically recorded and analysed.
Results:
Mean follow up was 17 months (range, 12 to 23 months). Radiological evaluation was performed at 1, 3, 6 and 12 months postoperatively, as well as at the last follow up visit. Clinical outcome was assessed using the parameters of Harris Hip score. Solid union was achieved in 57/60 patients (95%) at a mean time of 12.5 weeks. Two fractures did not progress to union. There were 3 superficial infections and 1 deep infection; all were successfully managed with appropriate antibiotic treatment. The Harris hip score at the last follow up visit was excellent or good in 46 (77%) of the patients.
Conclusions:
In the face of the good clinical and radiological results we consider the Veronail system to be of particular interest and perfectly adapted in primary surgery for both elderly and young patients.
INTRODUCTION
The need for internal fixation and early mobilisation of patients with trochanteric fractures of the femur is generally accepted, not only to reduce the morbidity/mortality rates associated with prolonged immobilisation, but also to improve the functional result in terms of malunion and mobility [1]. Over the last fifteen years, there has been a great deal of controversy over the optimum treatment of intertrochanteric fractures regarding extramedullary or intramedullary fixation. Although both implants are currently employed, intramedullary nailing systems are more preferable in unstable trochanteric femoral fractures due to their biomechanical and technical characteristics [2-4]. The most widely used extramedullary implant - the dynamic hip screw - seems to have a biomechanical disadvantage when compared with intramedullary devices because the load bearing in the proximal femur is predominantly shared through the calcar. Intramedullary devices are more stable under loading with a shorter lever arm, so the distance between the hip joint and the nail is reduced compared with that for a plate, so diminishing the deforming forces acrossthe implant [5]. For unstable trochanteric and subtrochanteric fractures the failure rate for the sliding hip screw has been reported as high as 20% [6].
An intramedullary device that can offer either a double-axis sliding or locked converging pattern of screws into the femoral neck may be adapted to the full range of intertrochanteric fractures. The Veronail (Veronail Trochanteric System, Orthofix, Bussolengo, Italy) is a new intramedullary device that combines the advantages of intramedullary nailing with high cephalic stability due to double axis fixation [7-9]. The device has 2 cephalic screws that can be inserted either in a parallel sliding configuration or in a convergent fixed configuration, hence providing a theoretically more stable fixation even in the most unstable fracture patterns. A multi-centre study has recently evaluated the feasibility of Veronail in various patterns of proximal femoral fractures and showed compatible clinical and radiological results [10].
This prospective analysis evaluated the effectiveness of this new intramedullary nailing system for the treatment of stable and unstable proximal femoral fractures in 60 consecutive patients and prospectively followed them up for a minimum of 12 months.
MATERIALS AND METHODS
Study Characteristics and Inclusion Criteria
We conducted a prospective study to evaluate the Veronail System for the treatment of stable and unstable trochanteric femoral fractures in a University Level 1 Trauma Center. Our unit is quite familiar with the use of the Proximal Femoral Nail-Antirotation (PFN-A) and Trochanteric Gamma Nail (TGN), which are the implants of choice for the treatment of extracapsular hip fractures. Enrolment in our study was from January 2008 through September 2009. We included extracapsular hip fractures classified as AO Type 31-A1 (21 cases), Type 31-A2 (15 cases) or Type 31-A3 (24 cases). We excluded those patients that were unable to walk before injury, those presenting with a pathologic fracture, any patient with previous ipsilateral hip or femur surgery, or any fracture with extension 5 cm distal to the inferior border of the lesser trochanter. Five patients died from reasons unrelated to the implant leaving a cohort of 60 patients who prospectively followed up for at least one year (mean follow up 17 months, range, 12 to 23 months).
All patients signed up the informed consent form before inclusion in the study. The study was authorized and approved by the local ethical committee and was performed in accordance to the ethical standards mentioned on the 1964 Declaration of Helsinki as revised in 2000.
Pre-Operative Data
The pre-operative variables (Table 1) included age, sex, mode of injury and type of fracture. Pre-fracture mobility was assessed with the Salvati and Wilson hip function scoring system [11] that considers four specific parameters; pain, walking ability, muscle power-motion and overall function. Pre-operative health status was assessed by obtaining a history of any comorbid diseases and medication, as well as by determining the American Society of Anaesthesiologists status of physical health.
Preoperative Data (60 Patients)
| Number of patients | 60 |
| Mean age (years) | 78 (42-93) |
| Sex Male Female |
25 40 |
| Mode of injury Fall at home Fall from height Traffic accident |
50 6 4 |
| Mean functional status* > 30 20-29 < 20 |
41 (68%) 10 (17)% 9 (15%) |
| ASA classification§ 1 2 3 |
18 (30%) 16 (27%) 26 (43%) |
| Fracture type (AO classification) A1 A2 A3 |
21 15 24 |
* Salvati and Wilson score.
§ American Society of Anesthesiologists status of physical health.
Intra-Operative Variables
Intra-operatively, we recorded the type of anaesthesia, the duration of the procedure, the amount of fluoroscopy, and the mean number of blood units transfused to the patients. Post-operative reduction of the fracture was assessed and characterised as anatomical, accepted or poor while the consultant surgeon considered the nature of the procedure as easy, moderate of difficult (Table 2). Less than 40 min operative time, successful closed reduction, minimal soft tissue dissection and uncomplicated application of the nail and screws were the characteristics of an “easy” operation whereas a non-anatomical closed reduction requiring opening at the fracture site or additional adjuvants measures, prolonged operative time (more than 60-70 min) and technical difficulties in nailing or screws application where the characteristics of a “difficult” operation. “Moderate” operations were somewhere between these two, although scoring was based mainly to the subjective opinion of the treating consultant. Intraoperative technical and mechanical complications related to the implant or the surgeon was registered as well.
Perioperative Variables
| Type of anesthesia General Spinal |
10 50 |
| Mean operating time (min) | 45 (24-90) |
| Mean fluoroscopy time (min) | 0,24 (0,1-0,3) |
| Kind of reduction Anatomical Acceptable Poor |
55 (91,6%) 3 (5%) 2 (3,4%) |
| Nature of the procedure Easy Moderate Difficult |
24 (40%) 31 (52%) 5 (8%) |
| Mean blood loss (units) | 0,625 per patient |
| Average hospitalization (d) | 7,3 days |
| Died in hospital | 2 |
Hospital Course and Stay
All patients received one dose of a 2nd generation cephalosporin intraoperative and 2 doses postoperatively except from allergic patients, who received vancomycin. All patients received thromboprophylaxis with subcutaneous low molecular heparin starting on the day of admission until the 3rd to 4th postoperative week. The rehabilitation protocol was identical, including withdrawal of drainage and mobilization out of bed on the second postoperative day and subsequent ambulation from the third or fourth day. In patients with 31.A1 fractures and 31.A2 fractures with adequate fixation, partial weight bearing was started from the third postoperative day while in cases of unstable fractures 31.A3, only non-ambulatory mobilization such as free bed movements and chair sitting till the third postoperative week and then partial weight bearing until the third postoperative month were permitted. We also recorded perioperative medical complications and overall duration of hospitalization.
Radiographic Parameters
Anteroposterior and lateral views of the affected hip were obtained preoperatively, postoperatively and at each follow-up visit. We noted any change in the position of the implants and the progress of fracture union. Union was defined when radiological callus formation was seen in 3 cortices in anteroposterior and lateral projections. Non-union of fracture was defined as the absence of visible callus in 3 cortices in both projections, 8 weeks postoperatively and the persistence of pain at the fracture site. Non-union, malunion, avascular necrosis, loss of reduction, breakage of screws or implant were recorded and evaluated.
Last Follow Up Evaluation
Radiological control, overall time of consolidation, the need of reoperation and the overall function according to Harris Hip scoring system [12] was evaluated at the last follow up assessment.
Surgical Technique and Implant Design
The Veronail implant has a length of 200 mm long and a 15 mm proximal diameter (10 mm distally), hence minimizing trochanteric entry damage and allows for percutaneous insertion even without reaming. It offers double axis proximal fixation with 7 mm cephalic screws that preserve the lateral wall of the femur providing rotational stability. The screws can be inserted in 2 different configurations: parallel sliding or convergent fixed (Fig. 1). The sliding screws are telescopic with a sleeve, which is firmly screwed into the nail. Sleeve and screw are integrated, allowing 10 to 40 mm of sliding (depending on the screw length), without the possibility of the screw disengaging from the sleeve. In the fixed (convergent) configuration both screws are screwed into the nail, with an angle of 120° (proximal cephalic screw) and 128° (distal cephalic screw). Both types of cephalic screws are self drilling and have a tapping thread. Distal locking can be static or dynamic and is achieved with partially threaded pegs. All implantable components of the system are made of titanium which allows for MRI investigations.
 |
Fig. (1). The Veronail system. |
A fracture table and an image intensifier were used in all cases. A skin incision of about 2-3 cm was made proximal to the tip of the greater trochanter, angled posteriorly at its proximal end. Insertion of the nail was done with the special handle supplied with the system. This handle can also be used for insertion of both types of cephalic screws as well as the distal pegs. The entry point can be created with either a cannulated drill bit or a cannulated awl.
Distal locking was either static or dynamic according to the bone quality and fracture type. In cases of subtrochantheric fractures (31.A3) the proximal screws were convergent and distal locking was dynamic (Fig. 2). In intertrochanteric (31.A1 and 31.A2) fractures, the proximal screws were parallel and distal locking was static (Fig. 3). The procedure for proximal locking is the same for both types of configuration and was performed by the insertion of two 4 mm cephalic threaded guides for the cephalic screws. With both guides in place, the proximal cephalic screw was inserted, followed by the distal cephalic screw. In this way, rotation of the femoral head, as described by Mills [13], is avoided. After insertion of both cephalic screws, guided distal locking was performed with the same handle.
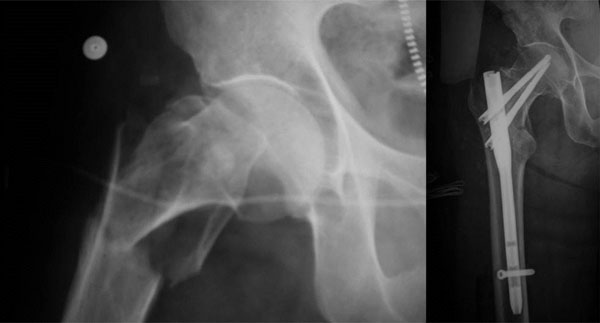 |
Fig. (2). Diverted configuration of cephalic screws and static distal locking. |
 |
Fig. (3). Parallel configuration of cephalic screws and dynamic distal locking. |
Statistical Analysis
Descriptive and inferential statistics were performed on all the data collected. All statistical analysis was performed using SPSS version 16.0 software. Overall differences between the groups were evaluated by analysis of variance, and individual paired comparisons were analyzed post-hoc with Sheffe’s test. When appropriate, unpaired t-test was performed to find any statistical differences between two groups. Results were considered significant at p<0.05.
RESULTS
Demographic and Baseline Characteristics
Sixty patients, 25 male and 35 female, with a mean age of 78 years old were available for the outcome analysis. There were 38 patients (63%) over 75 years old. A fall at home was the commonest mode of injury (83%). According to the AO/ASIF classification, there were 21 31-A1, 15 31-A2 and 24 31-A3 fractures. Fifty-five percent of the patients had significant comorbidity, mainly cardiopulmonary inefficiency, diabetes mellitus and a history of stroke or deep vein thrombosis, with 60% of them scored as ASA 2 or 3. The average time from injury to surgery was 3.5 days (range: 1 to 10 days) and the average duration of surgery 45 min. The main reason for the delay of the operation was the associated clinical status of the patients or the previous intake of anticoagulants. Ten patients were operated under general and 50 under spinal anesthesia. Fifteen procedures were performed by experienced residents and the rest by senior consultants. Anatomical fracture reduction was achieved in the operating theatre in 53 patients (88%) while the operating surgeon considered the operation as easy or of moderate difficulty in 55 patients (92%). There was no statistical difference in the quality of postoperative reduction between surgeons of different skill level. There were statistically significant differences in hospital stay and Harris Hip Score (HHS) between patients younger than 75 years old (n=22) in comparison with older patients (n=38). The younger patients had a shorter hospital stay (6.2±1.2 vs 7.8±2.0, p=0.002) and higher HHS values (89.1±3.1 vs 85.25±2.6, p<0.001).
Patients presented with an average haemoglobin level of 12, which dropped to 8.2, after surgery. Transfusion of packed erythrocytes was necessary in 25 patients (40%), with an average of 1.5 units. Overall transfusion requirement for the whole sample was 0,625 units per patient.
No serious intra-operative complications were reported. No difficulties were encountered with the surgical technique, probably due to the previous experience of the operating surgeons in intramedullary nailing. Application of the Veronail does not require any specific knowledge with respect to other nailing systems.
Five patients died within 2 months of the operation. Early and late fracture complications are listed in Table 3. There were 3 superficial (5%) infections, all successfully treated with broad spectrum intravenous antibiotics. One patient developed deep infection 17 days postoperatively and she successfully treated with surgical debridement and intravenous antibiotics for 4 weeks.
General Health and Fracture Complications
| General Complications | No. of Patients |
|---|---|
| Respiratory distress Decubitus ulcers Acute post-operative mental confusion Urinary infection Pulmonary embolism Deep venus thrombosis |
4 7 5 3 1 2 |
| Early Local Complications: | |
| Superficial infection Deep infection |
3 1 |
| Late Fracture Complications: | |
| Malunion in varus Nail breakage Nonunion |
5 1 2 |
Clinical and Radiological Outcome
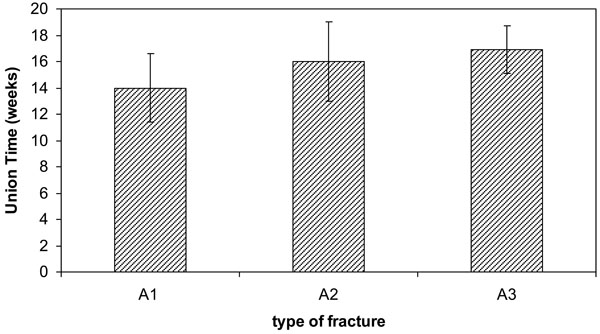
All survived patients were available for the last follow up evaluation. The mean follow-up period was 17 months (range, 12 to 23). Solid union was achieved in 57/60 (95%) patients (Fig. 4). Average healing time was 12.5 weeks (range: 11 to 20). Functional outcome according to the parameters of HHS was excellent or good in 46/60 (77%) patients. There were no statistically significant differences between men and women in union time (UT) or HHS. Patients with 31.A1 fractures had significantly shorter mean time to union compared to patients with A2 and A3 fractures (Table 4). No other variables (age, hospital days or HHS) were statistically different regarding fracture type. Female patients with A1 fractures (n=18) showed statistically significant higher HHS values than female patients with A3 fractures (n=22) [88.1±3.3 vs 85±3, p<0.05]. Accordingly, UT was lower in women with A1 fracture compared to those with A3 fracture (14.0±2.6 vs 17.1±1.7, p<0.05). There were no such statistical differences between fracture groups in men.
Comparison of Union Time (Weeks) Between Patients Suffering from Different Type of Fracture. (Values are Mean ± SD.* A1 vs A2: p<0.05 and † A1vs A3: p<0.01)
 |
 |
Fig. (4). A 82 years old woman suffered an AO-A2 trochanteric fracture. Healing of the fracture in 2 months and excellent radiological result at 2 years (HHS 90) |
Two cases with initial poor reduction and 5 cases that developed varus malunion had no severe functional impairment at the last follow up visit. Interestingly, all cases with varus malunion were of 31.A2 fracture type. In four of them the deformity was detected during the first postoperative month and was attributed to the very poor bone quality and the unrestricted weight bearing due to low compliance of the patients (Alzheimer disease). Although rare, we had 2 cases with non-union. Both cases were of 31.A3.1 type, with no comminution in the subtrochanteric region, and both patients had very restricted mobilization due to systemic problems in the contralateral extremity (hemiplegia and serious knee arthritis). As they both managed with proximal screws in converge configuration and dynamic distal locking, the fractures had no opportunity to heal through the dynamization process. A 68 years old female patient with 31.A3.1 fracture and Parkinson disease fell on the ground one month post operatively and the nail broke at the level of static locking. Revision of the fixation was carried out with a Trochanteric Gamma Nail. There were no cases of screw breakage, screw protrusion, cut-out or Z-effect [14].
DISCUSSION
Trochanteric fracture fixation, despite being one of the most commonly performed operation, is still prone to complications, either intra- or post-operatively. Evidence clearly supports the sliding hip screw (SHS) as the gold standard for fixation of a stable intertrochanteric fracture [15, 16], but it is less clear for unstable fracture patterns especially in the presence of posteromedial comminution [17-20]. Problems with SHS not only include delayed weight bearing, but also the need for extensive dissection for placing the side plate, opening of the fracture site and excessive blood loss. Introduction of intramedullary nails in the management of these fractures has enabled patients to walk with early weight bearing. Indeed, the cephalo-medullary devices minimise the surgical trauma, allow guided impaction of the fracture and decrease the lever arm of the loading force by virtue of medialised femoral fixation [21, 22]. In unstable fracture patterns, nails offer greater rigidity and resist varus deformity more effectively than sliding hip-screws [23, 24]. The conventional intramedullary nails for femoral trochanteric fractures have in common a bulky proximal part and a short nail length that can result in post-operative fractures under the tip of the nail. Newer generation nails (Trochanteric Fixation Nail-TFN, Proximal Femoral Nail Antirotation, PFN-A, Acer nail, TrochantericTM nail) have addressed the initial design shortcomings, thus reducing the incidence of secondary fractures [25, 26]. Bhandary et al. [27] showed in a recent meta-analysis of 25 prospective randomised trials that the relative risk for secondary fracture with 3rd generation cephalo-medullary implants has been eliminated.
In addition, whether the use of 1 or 2 lag screws offers better rotational control of the head fragment is still debated. Wang et al. [28] concluded that two lag-screw configurations should be avoided in patients who have a high risk of osteoporotic cut-out. Conversely, where bone appears sound but there is a possibility of greater load being transferred to the nail, two-screw configurations (with the upper screw slightly larger than the lower) was found to be a better option. A finite element study by Seral et al. [29] comparing the stresses produced by Gamma and proximal femoral nails in the treatment of trochanteric fractures showed increased stress shielding of the proximal femur with the stiffer Gamma nail. Vidyadhara and Rao [30] in a randomized clinico-radiological study of single and two femoral neck screw construct in the management of unstable trochanteric fractures in the elderly found no significant difference in the clinical outcome in the two groups, but there was less sliding of the femoral neck screws with the two-femoral neck screw configuration. Our experience with the older PFN implant [14] was disappointing as we have addressed technical complications and failures up to 30% of patients, especially Z-effect, reverse Z-effect and nail breakage.
A unique feature that differentiates Veronail from other double-axis systems is the alternative configuration of the cephalic screws, with either two parallel sliding screws or two convergent screws locked to the nail. This design allows the surgeon to select, depending on post-reduction fracture stability, the configuration of screws to use. The Veronail has the additional advantage of having a sleeve that guides the screw and aids sliding of the screws without becoming disengaged. Kubiak et al. [31]conducted a biomechanical study comparing trochanteric antegrade nails (Smith & Nephew, Memphis, TN) with a proximal diameter of 13 mm and an intramedullary hip screw. The devices were similar with respect to screw sliding or femoral head displacement under cyclical loading. However, the trochanteric antegrade nails were better with regards to load to failure because the bulky intramedullary hip screw could cause more bone destruction. The clinical trial [8] with a double screw hip nail reported complications rates similar to those of other methods of treatment. The intramedullary nail used were similar in dimensions, but were made of stainless steel, and without the interlocking mechanism with a sleeve that can be firmly screwed onto the nail. The double screw nail (Veronail) used in the study is a titanium, MRI compatible nail that has a small proximal diameter (15 mm) and a slight longer length (200 mm) than most of the one lag screw trochanteric antegrade nails. The small proximal part can be easily inserted into the proximal femur even without reaming in the proximal part of intertrochanteric fractures thus decreasing the risk of disruption of hip abductors [32]. The nail can also be manually inserted to place the lag screw at the proper position due to the small diameter (10mm) of the distal part. Another advantage of the Veronail is that placing the screws in the convergent way allows treating patients with a narrow femur neck achieving a strong and stable fixation.
Several reports have addressed the risk of head cutting-out with the use of cephalo-condylic implants which is estimated between 4-20% [1, 2, 5, 14, 16, 33]. It is strongly recommended that the best position of the lag screw is at the lower part of the femoral neck because the compression and tensile trabeculae of the proximal femur intersect at the lower part of the femoral neck and constitute the strongest architecture [34]. Furthermore, the lower the lag screw is, the more the bone can resist cutting out. In the Veronail, the 2 lag screws are firmly locked to the nail so that they offer a stronger fixation of the fracture even in fractures with slight varus reduction. In the current study, the inferior lag screws were tried to be inserted right above the inferior cortex of the femoral neck, thus preventing the so-called Z or reversed Z effectand avoiding cut out (Fig. 5). In our series there were only 8 patients (13.3%) less than 60 years old whereas the majority (64%) were osteoporotic fractures in elderly patients (> 75 years old) which are the common population in similar studies.
 |
Fig. (5). A 92 years old woman suffered an AO-A1 trochanteric fracture. Initial postoperative face and profile radiographs showed excellent reduction. The fracture was healed after 2 months. |
Mortality rates after a hip fracture have been estimated between 11% to 23% at 6 months and 22% to 29% at 1 year post injury [35]. Our study showed a low mortality rate of only 8%, which could be explained by the small number of the patients. Another reason would be the fact that most of the patients (60%) suffered from a quite stable trochanteric fracture (31.A1, 31.A2), which is a favourable prognostic factor as has been recently reported by Cornwall et al. [36] in large series of patients.
Hospital stay, blood loss, early mobilization, time of union, systemic and local complications and final functional outcome were comparable to that of similar reports of the newest cefalo-condylic implants [8-10, 25-30, 37].
Limitations of the present study include the small number of patients, the relatively short follow up period, the lack of randomization in terms of implant selection and the absence of control group. Having already great experience with intramedullary nailing in all types of throchanteric fractures we ascertained Veronail system as a reasonable alternative to TGN and PFN-A which are currently used in our clinic. We think that its main advantages are a) the ability to choose either the sliding parallel or fixed diverged configuration of femoral neck screws thus adapted to various patterns of proximal femoral fractures, b) its small proximal diameter that is not violate the lateral cortex and c) the special designed sleeve which is firmly screwed into the nail without the possibility of the proximal screw to disengage from the sleeve. Additional investigation and larger series of patients will prove its biomechanical superiority and minimal invasiveness. Prospective randomized studies comparing the Veronail with sliding hip screw and other cephalo-condylic nails are still required.
CONFLICT OF INTEREST
The author confirms that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.







