All published articles of this journal are available on ScienceDirect.
Patient-Based Outcomes After Tibia Fracture in Children and Adolescents
Abstract
Introduction :
Tibia fractures are common in pediatric patients and time necessary to return to normal function may be underappreciated. The purpose of this study was to assess functional recovery in pediatric patients who sustain tibia fractures, utilizing the Pediatrics Outcome Data Collection Instrument (PODCI), in order to provide evidence-based information on post-injury functional limitations and anticipated recovery times.
Methods :
84patients (out of 264 eligible patients, response rate 32%) age 1.5-18 years treated for a tibia fracture at a large children's hospital between 1/07 and 4/08 completed a PODCI questionnaire at 6 and 12 months post-injury. PODCI questionnaires were compared to previously reportednormal controls using Student's t-test in six categories.
Results :
At 6 months after injury, the Sports functioning PODCI score was significantly less than healthy controls in both the parent reports for adolescent (mean 88.71 versus 95.4) and adolescent self-report (mean 90.44 versus 97.1); these showed no difference at 12 months.
Discussion :
For adolescents who sustain fractures of the tibia, there remains a negative impact on their sports functioning after 6 months that resolves by 12 months. Physicians can counsel their patients that although they may be limited in their sports function for some time after injury, it is anticipated that this will resolve by one year from the time of injury.
Level of Evidence :
Level II.
INTRODUCTION
Fractures of the tibia and ankle are common in the pediatric population, accounting for approximately 15% of long-bone fractures among children and adolescents [1]. Despite their incidence, the orthopedic literature contains only a few studies that have explored post-injury function utilizing patient-based outcomes for young patients who have sustained these injuries [2-5], and a few that report return to sports outcomes in adults [6, 7]. With this study, we sought to gain a better understanding of the impact these fractures have on pediatric and adolescent patients, both functionally and temporally, so we can better inform our patients about reasonable expectations, particularly with returning to sports activities.
The Pediatric Outcomes Data Collection Instrument (PODCI) is a functional health outcome measure for children and adolescents that focus on musculoskeletal health and quality of life. It is comprised of several dimensions that assess upper extremity function, transfers and mobility, physical function and sports, comfort/pain (pain-free), and happiness. There is also a scale for global functioning, which is a combination of the three function subscales and comfort. The PODCI has been shown to be reliable, valid and sensitive to change [8].
Utilizing the PODCI, we sought to understand the impact of tibia fractures on pediatric patients and what functional outcomes could be expected after six and twelve months post-injury. By determining the functional status of patients after this injury at two time points post-injury, we hope to provide Orthopedic surgeons treating these injuries with information that will help guide treatment of patients, education of parents and patients, and to provide realistic expectations to them with regard to quality of life and return to sports and physical activities.
MATERIALS AND METHODS
The study was approved by the Institutional Review Board of the hospital. All pediatric patients who presented to our large pediatric hospital between January 2007 and April of 2008 with a fracture of the tibia were asked to participate in the study. Patients with neuromuscular conditions, metabolic bone disease, insufficiency fractures, or fractures resulting in amputation, were excluded from the study. Two hundred and sixty-four patients who met the inclusion criteria were invited to participate. Data was collected retrospectively on each patient to determine patient’s age, gender, date of fracture, and anatomic area/type of fracture. See Table 1.
Percent Distribution of Patient and Injury Characteristics
| N | % | ||
|---|---|---|---|
| Age | 2-5 | 25 | 29.8% |
| 6-10 | 27 | 32.1% | |
| 11-18 | 30 | 35.7% | |
| Anonymous | 2 | 2.4% | |
| Gender | Male | 54 | 64.3% |
| Female | 28 | 33.3% | |
| Anonymous | 2 | 2.4% | |
| Primary Fracture | Proximal Metaphyseal | 2 | 2.4% |
| Diaphyseal/Shaft | 55 | 65.5% | |
| Salter Harris I/II Tibia | 14 | 16.7 | |
| Salter Harris III/IV Tibia | 4 | 4.8% | |
| Tillaux / Triplane | 3 | 3.6% | |
| Medial malleolus | 2 | 2.4% | |
| Salter Harris I/II fibula | 2 | 2.4% | |
| Anonymous | 2 | 2.4% | |
| TOTAL | 84 |
For each eligible patient, a PODCI questionnaire was mailed to their home six months after their original injury and a second questionnaire sent at twelve months after injury. All three versions of the Outcomes Instrument were utilized for this study: pediatric (parent reported) questionnaire, adolescent (parent reported)questionnaire and adolescent (self reported)questionnaire. As defined by the PODCI guidelines, a pediatric patient is between the ages of 2 and 10 years and an adolescent is between the ages of 11 and 18 years. For our study, we used the patient’s age at the six-month and twelve-month time from injuryto determine if they were a child or adolescent for the purposes of our study. For children less than eleven years of age, a Pediatric questionnaire was provided to their parent to complete. For adolescents, both the patient and their parent were asked to fill out a study questionnaire. To increase response rates a web-based version of the questionnaire was also made available for those who preferred to respond via the internet.
For each patient, there are five scales and one global functioning scale calculated from their PODCI: Upper Extremity and Physical Functioning, Transfer and Basic Mobility, Sports and Physical Functioning, Pain/Comfort, andHappiness (with their physical condition). The Global Functioning scale consists of the means of the four scales: Upper Extremity and Physical Function, Transfer and Basic Mobility, Sports and Physical Functioning, and Pain/Comfort. Per the scoring algorithms, any question left blank or answered as “Too young for this activity” is considered missing and is not factored into the scale. For the PODCI, zero is the lowest possible score, representing a poor outcome/worse health and 100 is the highest, representing best possible outcome/best health. Version 2.0 of the AAOS/COMSS/COSS Outcomes Data Collection Instruments scoring algorithms were utilized.
Results from our study were compared to previously published normal controls [9]. This dataset includes PODCI results for all domains and age groups and reports the number of patients included, mean, standard deviation and skew for a series of normal children in Texas. Because this was the only data for our control group available, we compared these statistical parameters to our own data. However, this limited the analysis to a comparison of means scores. A non-parametric analysis could not be used even when the data distribution was non-normal and skewed.
Data Analysis
Statistical significance was set a priori at p<0.05.
For scores in each of the three categories (Parent of child, Parent of Adolescent, and Adolescent Self-Report) and for each of the six scales (Upper Extremity, Transfers, Sports, Pain, Happiness and Global), mean, minimum value, maximum value, skewness and standard deviation were calculated using SPSS (Chicago, IL). These were then compared to previously published normal controls [9] using Student’s t-test in Graph Pad version 3.06 (InStat, San Diego, CA). Our data was assessed for normalcy; despite elevated skew in some data, we were not able to compare using non-parametric tests because the original data set from Haynes et al. [9] was not available to us. The populations from our study and Haynes et al. had different standard deviations; thus the comparison through Graph Pad was done using unpaired, Welch corrected t-test.
For the patients who completed both 6 and 12 month questionnaires, we conducted non-parametric Wilcoxon Matched Pairs test (2-tailed) to determine if there were significant differences between 6 and 12 months for this small group of patients. This was done using Excel and StatPlus.
A non-responder analysis was also performed using Chi-Square in SPSS to ensure that there was no significant difference between the responders and non-responders. Age at injury, gender, primary fracture type, open versus closed injuries, mechanism of injury, need for reduction and the method of surgical fixation were all evaluated.
RESULTS
Of the 264 patients that met inclusion criteria and were invited to participate, 91 responded. Eighty-four agreed to participate in the study and completed at least one (66 patients) if not both (18 patients) of the PODCI questionnaires; this yielded a response rate of 31.8%. Many of the non-responsive patients did not have a current mailing address on file and their questionnaires were returned without a forwarding address.
Of the 84 patients whose parents agreed to participate, 54 were boys (64.3%) and 28 were girls (33.3%) and two (2.4%) chose to remain anonymous. Age at time of injury ranged from 1.5 to 16.3 years. This demographic information and specific incidence rates by fracture type and location are shown in Table 1. Fractures of the tibial shaft accounted for the majority of fractures in our study population (65.5%).
Forty-nine patients returned completed 6-month questionnaires; 23 of these were Pediatric and 26 were Adolescent. See Tables 2a and 2b for the patient characteristics of each group. For the 26 responding families of adolescent patients, 26 filled out Adolescent-parent reported questionnaires and 25 of the 26 adolescents completed self-reported questionnaires. For the fifty-two that responded to the 12-month questionnaire, 31 were Pediatric and 21 were Adolescent-parent reported. Twenty Adolescents completed their self-reported questionnaires as well. There were 17 patients for whom both a six- month and a twelve- month PODCI were completed. See Table 3 for the PODCI results, including assessment of normalcy of the data (mean, minimum, maximum, standard deviation and skewness).
Characteristics of Pediatric Patients with Tibia Fractures who Completed the PODCI 6 and 12 Months After Injury
| Pediatric Population | ||
|---|---|---|
| 6 Month Follow-Up (N=23) | 12 Month Follow-Up (N=31) | |
| Mean Age (at time of survey) (years) | 5.31 (SD 3.04) (N=22) |
5.51 (SD 2.56) (N=31) |
| Gender | 17 Male 5 Female (N=22) |
18 Male 13 Female (N=31) |
| Mean Height (cm) | 117.12 (N=14) |
114.78 (N=25) |
| Mean Weight (kg) | 23.5 (N=17) |
21.2 (N=27) |
| Mean BMI | 16.78 (N=13) |
15.88 (N=25) |
| Number Needing Reduction | 5 (26.3%) (N=19) |
8 (28.6%) (N=28) |
| Number Open Fractures | 0 (0.0%) (N=22) |
1 (3.2%) (N=31) |
| Primary Fracture Location | Shaft Fx = 15 (68.2%) Intra-Articular Fx = 1 (4.5%) (N=22) |
Shaft Fx = 25 (80.6%) Intra-Articular Fx = 1 (3.2%) (N=31) |
Characteristics of Adolescent Patients with Tibia Fractures who Completed the PODCI 6 and 12 Months After Injury
| Adolescent Population | ||
|---|---|---|
| 6 Month Follow-Up (N=26) | 12 Month Follow-Up (N=21) | |
| Mean Age (at time of survey) (years) | 12.96 (SD = 1.50) (N=25) |
12.22 (SD 1.39) (N=21) |
| Gender | 16 Male 9 Female (N=25) |
13 Male 8 Female (N=21) |
| Mean Height (cm) | 164.18 (N=24) |
159.31 (N=19) |
| Mean Weight (kg) | 58.9 (N=24) |
55.94 (N=19) |
| Mean BMI | 21.85 (N=24) |
21.88 (N=19) |
| Number Needing Reduction | 19 (79.2%) (N=24) |
17 (81.0%) (N=21) |
| Number Open Fractures | 0 (0.0%) (N=24) |
1 (3.2%) (N=21) |
| Primary Fracture Location | Shaft Fx = 12 (48.0%) Intra-Articular Fx = 7 (28.0%) (N=25) |
Shaft Fx = 12 (57.1%) Intra-Articular Fx = 2 (9.5%) (N=21) |
PODCI Results at 6- and 12-Months
| 6 Month PODCI | 12 Month PODCI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Min | Max | Mean | Std. Deviation | Skewness | N | Min | Max | Mean | Std. Deviation | Skewness | |
| Upper Extremity Functioning | ||||||||||||
| Parent of Pediatric Parent of Adolescent Adolescent |
20 26 25 |
83.00 91.67 95.83 |
100 100 100 |
97.27 99.52 99.83 |
5.80 1.80 0.83 |
-1.87 -3.96 -5.00 |
30 21 20 |
41.67 100 100 |
100 100 100 |
93.72 100 100 |
12.90 0.00 0.00 |
-2.77 0 0 |
| Transfer & Basic Mobility | ||||||||||||
| Parent of Pediatric Parent of Adolescent Adolescent |
23 25 24 |
93.00 90.91 96.97 |
100 100 100 |
98.83 99.42 99.75 |
2.37 1.92 0.86 |
-1.71 -4.03 -3.22 |
30 21 20 |
87.88 93.94 93.94 |
100 100 100 |
98.70 99.71 99.70 |
3.04 1.32 1.36 |
-2.52 -4.58 -4.47 |
| Sports and Physical Functioning | ||||||||||||
| Parent of Pediatric Parent of Adolescent Adolescent |
23 25 24 |
65.00 52.08 58.33 |
100 100 100 |
90.68 88.71 90.44 |
10.03 13.91 11.33 |
-1.22 -1.37 -1.37 |
30 21 20 |
71.67 66.67 73.48 |
100 100 100 |
94.20 94.85 96.48 |
6.86 8.32 6.75 |
-1.58 -2.27 -2.66 |
| Pain/Comfort | ||||||||||||
| Parent of Pediatric Parent of Adolescent Adolescent |
23 26 25 |
67.00 66.67 60.56 |
100 100 100 |
97.78 90.79 91.49 |
7.22 12.25 13.83 |
-3.94 -0.96 -1.28 |
31 21 20 |
66.67 49.44 49.44 |
100 100 100 |
96.94 95.57 87.65 |
9.00 11.89 16.58 |
-2.94 -3.39 -1.25 |
| Happiness | ||||||||||||
| Parent of Pediatric Parent of Adolescent Adolescent |
16 26 25 |
90.00 20.00 50.00 |
100 100 100 |
98.06 84.23 86.60 |
3.66 22.79 15.19 |
-1.64 -1.73 -1.03 |
29 21 20 |
60.00 70.00 75.00 |
100 100 100 |
96.03 93.57 95.50 |
8.70 8.54 6.86 |
-3.05 -1.31 -1.69 |
| Global Functioning | ||||||||||||
| Parent of Pediatric Parent of Adolescent Adolescent |
20 25 24 |
88.64 82.36 83.33 |
100 100 100 |
96.06 94.52 95.29 |
3.94 5.34 5.15 |
-0.57 -0.59 -0.90 |
29 21 20 |
80.05 79.03 80.73 |
100 100 100 |
95.72 97.53 95.96 |
5.54 5.02 5.39 |
-1.65 -3.03 -1.58 |
Patients who Filled Out Both 6 Month and 12 Month Questionnaires
There were 18patients who filled out both the 6 and 12 month questionnaires. Of these, 7were Pediatric patients and 9 were Adolescent patients; one patient completed both questionnaires but fell into the Pediatric category for the 6-month follow-up and the Adolescent category for the 12-month follow-up, thus he was not included in this analysis and therefore 17 patient were included in the analysis. For the adolescent population, there was a significant improvement in parent-reported Sports and Physical Functioning (p= 0.018) and Global Functioning (p= 0.018) scales from 6 to 12 months. For adolescents self-reporting there was a significant improvement in Sports and Physical Functioning scale from 6 to 12 months (p = 0.018). For the Pediatric patients, there were no statistically significant differences for the seven patients between 6 and 12 months.
Patients who Filled Out the 6 Month and/or 12 Month Questionnaire
We then compared our study population to the normal control data published by Haynes and Sullivan [9] at both 6 months and 12 months after injury. See Fig. (1a-1c). At six months after injury, the Sports and Physical Functioning PODCI score was significantly less than normal controls in both the Adolescent parent-reported (mean 88.71 versus 95.4; p=0.043) and Adolescent self-reported (mean 90.44 versus 97.1; p=0.011). By twelve months, there was no significant difference in Sports and Physical Functioning between our study population and the published normal controls. There were also significantly higher scores for our Pediatric patients compared to controls in Happiness at both 6 (mean 98.06 versus 86.8) and 12 (mean 96.03 versus 86.8) months after injury and Adolescent self-report at 12 months (mean 95.5 versus 86.3).

Parent report of pediatric patient (ages 2-10 years) for PODCI scores comparing data from Haynes and Sullivan to our 6 month and 12 month after injury scores. * denotes p<0.05 significance.
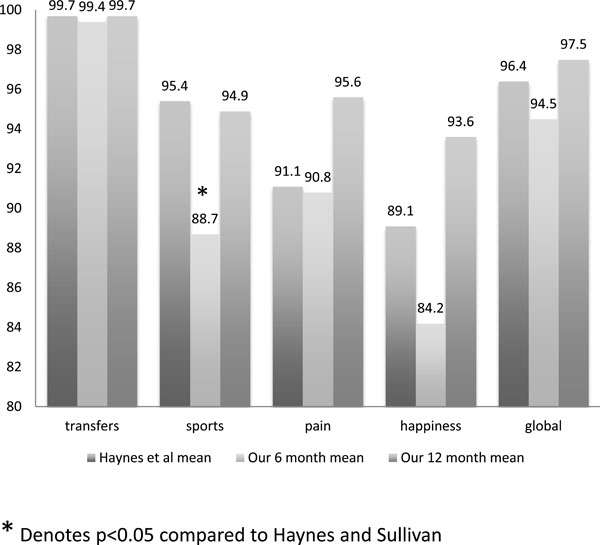
Parent report of adolescent patient (ages 11-18 years) for PODCI scores comparing data from Haynes and Sullivan to our 6 month and 12 month after injury scores. * denotes p<0.05 significance.
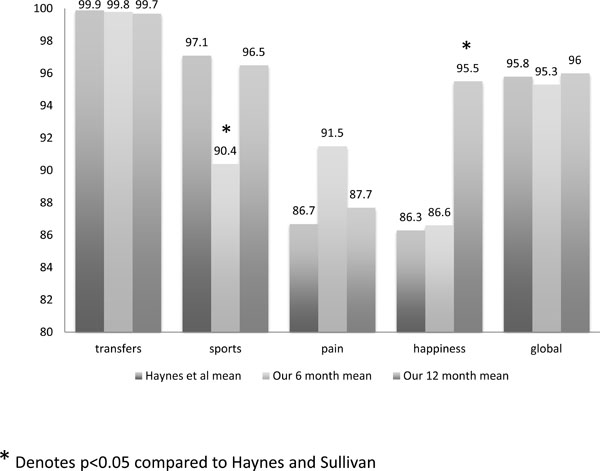
Self report of adolescent patient (ages 11-18 years) for PODCI scores comparing data from Haynes and Sullivan to our 6 month and 12 month after injury scores. * denotes p<0.05 significance.
Non-Responder Analysis
The non-responder analysis showed no statistically significant differences between the responders and non-responders across all parameters tested. There was no statistically significant difference between these groups when compared for age at time of injury, gender, primary fracture type, open versus closed injury, mechanism of injury, need for reduction and surgical fixation method utilized for those fractures that were treated surgically.
DISCUSSION
There is little available in the literature to help physicians guide patient and family expectations on the functional return after tibia or ankle fractures in the pediatric population. Patients and their families often want to know immediately after an injury about the expected return of function so advanced planning of future activities such as sports camps and after school activities can be anticipated. Utilizing the PODCI, we found a full return of all patient-based outcomes was achieved by 6 months after tibia or ankle fracture in the pediatric population. However in the adolescent population, both the patient and the parent responses demonstrated a Sports and Physical Functioning score which was still significantly impaired at 6 months and improved and normalized by 12 months. We found in this group of older kids, it takes over 6 months to fully return to normal athletic activity after a fracture of the tibia and/or ankle.
Other authors have also found using patient-based outcomes that it can take up to a year to recover from a significant lower extremity injury. Ding et al. [2] utilized the Pediatric Quality of Life Inventory (PedsQL) to evaluate health-related quality of life after an extremity fracture in the pediatric population that was severe enough to warrant hospitalization. Of 100 enrolled children, 52 of them had lower extremity fractures. They showed that children who sustained a tibia and/or fibula fracture had significantly poorer physical health during their first year after injury than did children who had sustained upper extremity fractures.
Additionally, despite significant decline in physical and psychosocial well-being during the first three months post-injury, most of the children in their study had recovered by one-year post-injury [2]. Their study, like ours, was limited by a small sample size that did not allow for evaluation by particular fracture type. Their lower extremity fracture population included both patients with femur fractures and tibia and/or fibula fractures. Also, their study only included patients with injuries severe enough to warrant hospitalization.
Stancin et al. [4] published a prospective study evaluating outcomes following pediatric traumatic fractures at six months and one year after injury for both the patient and their families. Their study population of 57 ranged in age from six to twelve years of age and the patients had injuries severe enough to warrant hospitalization. Sixty-seven percent of their patients had sustained lower extremity trauma (including pelvic, femur and/or tibia fractures). They combined all lower extremity traumas for the purposes of their study. Using various standardized outcomes instruments, including the Vineland Adaptive Behavior Composite, the Child Behavior Checklist, the Child Health Interview (to determine number of functional limitations), the Family Burden of Injury Interview, the Impact on Family Scale (Version G) and the Brief Symptom inventory, they measured pre- and post-injury child and family functioning. They found that outcomes were primarily positive by one year post-injury, but observed that family stress and functional limitations for the child were present up to 6 months after injury [4].
These studies, like ours, demonstrate that children who sustain lower extremity trauma remain functionally limited for several months after their injury, but by one year, these limitations seem to have resolved. Unlike the Ding and Stancin studies, our study population did not include pelvic or femur fractures; we included only fractures of the tibia and/or ankle. These other studiesonly evaluated patients with injuries severe enough to warrant hospitalization; this is only a subset of the pediatric trauma population. Our study included all patients with a tibia fracture - regardless of injury severity, hospitalization, or method of treatment.
This is the first study to our knowledge that utilizes the PODCI to evaluate child and adolescent outcomes after fractures of the tibia. Our study sought to provide the orthopedic community with information on outcomes after these fractures and allow us to provide information to our patients on what they can expect in terms of function and quality of life after injury. Our results show that the level of function in sports or physical activities of adolescents who sustain fractures of the tibia remains negatively impacted six months after injury. This negative impact resolves by 12 months. This difference was seen both in our paired population and in the evaluation of our population compared to the established healthy controls. We also found that for our Adolescent population, their happiness scores were not significantlydifferent than the healthy controls at 6 months from time of injury, but was significantly better by 12 months. We do not think there is any clinical importance to the happiness score being significantly elevated compared to our literature control group, but is more a factor of that control group than our patient series. This has been also seen in another study that compared their results to the Haynes et al. [9] normative data [10]. It is interesting that our patient’s happiness score increased between 6 and 12 months after injury, and our patients happiness score remains higher than the comparison data. We feel that this is likely a result of the depressed values for happiness from the Haynes and Sullivan data more than an elevated happiness of our patients. Other studies that utilized the Haynes and Sullivan data have also found relatively low happiness scores in that data [10, 11]. More importantly, at the same time we also saw significant improvement in their Sports and Physical Functioning scores.
There are several limitations in this study that should be considered when evaluating our results. Unfortunately we had a low response rate, which limited our study numbers. We were not able to control for specific age in the comparisons. Given limited sample size, we combined all fractures of the tibia and/or ankle together instead of evaluating by injury pattern or anatomic area. A larger sample size or greater response rate would have allowed for comparisons to be made within a particular fracture group or anatomic area that may further improve our ability to counsel our patients effectively. Additionally, with a larger population of respondents, we may have been able to stratify the population by treatment rendered to assess differences in outcome based on fracture type, severity, and methods of treatment. Another limitation is the small sample size for patients who returned both 6 and 12 month questionnaires, thereby limiting our paired comparison of outcomes in our study population. As such, we are unable to draw meaningful conclusions from the patients who returned both sets of questionnaires. However, these results did mirror our general results, thus supporting each set of results. While our general patients response for the 6 month and 12 months post-injury groups were a different cohort of patients, we have no reason to suspect any factors that would confound these two groups and make the comparison invalid. Nonetheless it is possible that the non-responder group differed in outcome, which may be why they did not respond to our survey. Similarly, it is possible that the groups in the 6 month and 12 month follow-up were different resulting in the difference in results found comparing these groups.
In comparing our data to the Haynes et al. study [9], we compared averaged data (n, mean, standard deviation) because we did not have the raw data from the Haynes et al. study available to us. This limited our ability to perform non-parametric tests even when the normalcy assessment of our data showed an elevated skewness. We did perform an unpaired Welch-corrected t-test for comparison due to variability in the standard deviation. Other studies have also compared their results to Haynes et al. data in a similar fashion [10,11], although the statistical details of their comparisons were not described. While this may not be statistically the best comparison of the data, given that most of the skew values showed reasonably normal distribution, we feel that our results are not compromised despite not having non-parametric tests available to us.
Both the Ding [2] and Stancin [4] studies had large enough numbers of respondents to their questionnaires at different time periods that they were able to evaluate for improvement within their study population. Although we were able to show statistical significance in some areas within our study populationin our paired analysis, any lack of significance and conclusions drawn from this analysis should be tempered by the limited power in our study. The results of our non-responder analysis revealed that our group of responders reasonably represents the population of tibia and/or ankle fractures treated at our institution during this time. We are not aware of any selection bias in this responder group.
Despite the limitations of the study, we gain from this analysis a better understanding of the impact of these fractures on children and adolescents at 6 and 12 months after injury. For orthopedic surgeons caring for these patients, we can counsel our adolescent patients and their families to anticipate some limitation, particularly sports functioning, for over six months after injury, but that we anticipate that this will resolve by one year after injury.
CONFLICT OF INTEREST
Ms. Curtis has no financial disclosures related to this topic.
Dr. Sabatini has no financial disclosures related to this topic.
Dr. Mahan has no financial disclosures related to this topic; her husband received a salary and stock options from PFIZER.
ACKNOWLEDGEMENTS
Declared none.


