All published articles of this journal are available on ScienceDirect.
Do We Need Radiological Guidance for Intra-Articular Hip Injections?
Abstract
There is still a debate as to whether radiological guidance is needed for intra-articular hip injections. The aim of this study was to evaluate correct needle positioning for the hip joint performed with a non-radiological method and confirmed on arthrogram under image intensifier.
Patients listed for diagnostic and therapeutic hip joint injections were included in our study. Eighty seven patients (100 hips) underwent injections with the non-radiological method using anatomical landmarks. Fluoroscopy and arthrogram were then used to confirm the needle position. The primary outcome measure was the success rate of correct positioning of the needle in hip joint by the non-radiological method, as confirmed on arthrogram under image intensifier. The secondary outcome measures were relationship between the grade of the surgeon and patient BMI to success rate of hip injections by the non-radiological method.
Overall success rate with the non-radiological method was 67%. Consultants were 77.1% successful and registrars 57.7% (P = 0.039). The average body mass index (BMI) in the successful group was 28.45 (SD = 5.21) and 32.03 (SD = 4.84) in the unsuccessful group (p=0.001). Success was further improved to 88% when performed by a consultant in low BMI (< 30) patients.
This prospective study shows that hip injections can be performed with reasonable success without radiological guidance. Experienced surgeons may be able to perform this procedure in outpatient clinics in normal BMI patients; thereby reducing costs and the need for bed space.
INTRODUCTION
Intra-articular injections of hip joint are widely performed both for diagnostic and therapeutic purposes [1-4]. Hip joint injections are performed by various techniques and although some recommend fluoroscopy or USS guided technique [1, 2, 4], others claim that injections can be performed without imaging guidance [3, 5, 6]. The advantage of the non-radiological method is that it is inexpensive and avoids radiation, risk of contrast reaction and inpatient admission. The purpose of our study was to assess the accuracy of hip joint injection by the non-radiological method. This study tests the hypotheses that the hip joint can be injected safely and reliably, using anatomic landmarks, without fluoroscopic guidance.
METHODOLOGY
Patients listed for diagnostic and therapeutic hip joint injections were included in our study. Eighty seven patients (100 hips) with symptomatic hip osteoarthritis were given intra-articular Chirocaine (Levobupivacaine hydrochloride 2.5 mg, 10 mls) and corticosteroid injections (Depomedrone 80 mg) following informed consent. Patients underwent a standard anatomically referenced anterior injection technique. Patients were positioned supine on a radiolucent table and procedure was performed using an aseptic technique under sedation using intravenous Fentanyl (1-1.5 mcg/kg) and Midazolam (0.025-0.03 mg/kg), with a Propofol bolus (upto 50 mg) and oxygen and nitrous oxide by face mask if required. A 22 gauge spinal needle is inserted approximately 2.5-3.5 cm lateral to the intersection of the femoral artery and the inguinal ligament. The needle was directed posteromedially at an angle of 20° until bone was reached as shown in Figs. (1, 2). An x-ray image intensifier was used to confirm the position of the needle and injection of a radio opaque contrast (Omnipaque 250) as shown in Fig. (3).

Anatomical landmarks: Anterior Superior Iliac Spine and Femoral artery (X).
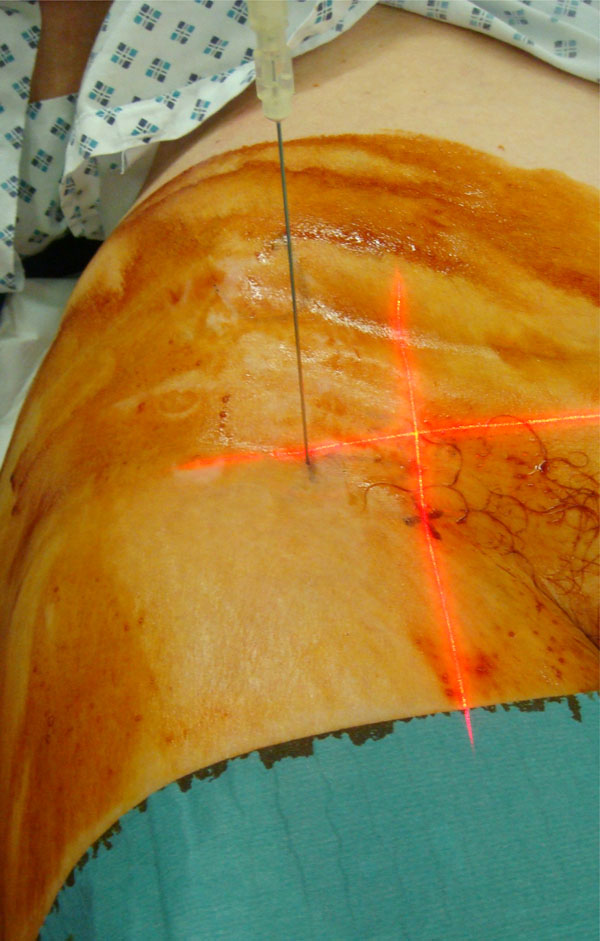
Needle placement 3 cm lateral to the intersection of the femoral artery and the inguinal ligament. The needle is directed posteromedially at an angle of 20° until bone was reached.

Fluoroscopic image showing needle placement and intraarticular cntrast uptake.
Patients who had accurate placement of needle by the non-radiological method, as confirmed by intra-articular contrast were classified as successful. Patients who did not have accurate placement of needle by the non-radiological method, as confirmed by inadequate positioning of needle or no intra-articuar uptake of contrast were classified as unsuccessful. The injections were all performed by general consultant orthopaedic surgeons and orthopaedic trainee surgeons. The grade of the injecting surgeon (consultant or trainee), patient body mass index (BMI), success rate was recorded. The primary outcome measure of the study was success rate of the hip joint injection by the blind method, as confirmed by successful arthrogram. The secondary outcome measures were relationship between the grade of the surgeon and success rate of hip injections performed by blind method and relationship between BMI and success rate with the blind method. SPSS 17 was used for statistical analyses. Data were expressed by descriptive statistics and percentages.
RESULTS
The results are summarized in Table 1. Eighty seven patients had 100 hip injections. The average age of the patients was 69 years (Range 43-96 years). The average patient BMI was 30.24 Kg/m2 (Range 19.2–43.2 Kg/m2). The success rate with the non-radiological method was 67%; the success rate for consultants was 77.1%, and for trainees was 57.7% (P=0.039). The average BMI was 28.45 (SD=5.21) in the group that had successful hip injection by the non-radiological method, and 32.03 (SD=4.84) in the group where the injection was unsuccessful (P=0.001). Forty-nine patients (56%) were non-obese group (BMI <30). The success rate by non-radiological method in the non-obese group was 82.1%, with consultants having a success rate of 87.9% and trainees having a success rate of 73.9% respectively (P=0.179 Chi – square test).
Success rate of the non-radiological method of hip injections.
| All Patients N=87 (100%) |
Non-Obese Patients N=49 (56%) |
||
|---|---|---|---|
| Success Rate | Overall | 67% | 82.1% |
| Consultant | 77.1% | 87.9% | |
| Trainee | 57.7% | 73.9% | |
None of the patients in our study population developed tenderness, hematoma, allergic reaction or Infection.
DISCUSSION
Hip injections are performed by orthopaedic surgeons, radiologists, rheumatologists and pain specialists. Most orthopaedic surgeons and radiologists do this under radiological guidance whereas the latter two tend to perform it blindly using anatomical landmarks without radiological interventions [1]. Studies in the literature [1, 2, 4, 7] have suggested that non-radiological hip injection can be inaccurate and pose danger to the nearby neurovascular structures, and should be performed under image intensifier especially in patients with high BMIs, severe arthritis and flexion deformities. However these studies did not take into account the level of experience of the surgeon or physician; this is an important factor, as shown in our study.
Karup & Ward [1] and Demirhan et al. [4] suggest that non-radiological injections of the hip joint can be inaccurate even with careful technique and have recommended the use of image guidance. However, in both of these studies, injections were carried out by lateral approach. Mauffrey & Pobbaley [3] reported a success rate of 19 out of 20 patients by non-radiological methods using the lateral approach. They did not however comment on patient BMI and, based on our study, their results may be biased. In our study all the injections were carried out by the anterior approach using anatomical landmarks. Recently Mei-Dan et al. [5] have shown a 93% success rate with the anterior approach for non-radiological intra-articular injection of the hip using anatomic landmarks. This study on 55 patients concluded that the non-radiological technique is safe and easily reproducible, however they have reiterated that patient BMI and surgeon experience could be limiting factors.
All previous studies have limited patient numbers and our study is the largest series to look at this issue. Ours is the largest study (N=87), comparing the results of successful hip injections by non-radiological methods with the grade of surgeon and also patient BMI. All the injections in our study were carried out by anterior approach and we used fluoroscopy and gold standard arthrogram to confirm needle placement.
There is still an ongoing debate with regards to the various techniques of hip injection with most authors recommending the lateral and anterior approaches [1, 2].Leopold et al. [2] in their study on 15 cadavers had an 80% success rate and suggested that the lateral approach is safer than anterior approach with regards to neurovascular injury. The authors recommend the lateral approach along with fluoroscopy or ultrasound. We believe that the risk of neurovascular injury is negligible with careful palpation and utilizing anatomical landmarks. None of the patients in our study and in the study by Mei-Dan et al. [5], using anterior approach recorded any evidence of neurovascular injury.
Hip Injections have been tried in the outpatient setting [5] and cost about £35. In our practice, all hip injections are performed as elective day case procedures costing around £1,234. The main concerns with performing hip injection as an outpatient procedure are pain and accuracy of needle placement. The pain threshold of patients varies and we appreciate that accurate needle placement is not guaranteed, especially in obese patients, without imaging, There are significant implications of a false positive and false negative result when the injection is performed for diagnostic indications. On the other hand, outpatient injections are an attractive option in high risk anesthetic patients, and in view of the low costs.
CONCLUSION
We believe that some hip injections can be performed in outpatient setting in a selected group of patients with the correct indication and appropriate BMI, and by experienced surgeons. This would result in cost saving and bed days, which is particularly pertinent in current health service climate of efficiency savings.
CONFLICT OF INTEREST
None of the authors received any financial contributions for this study and none of the authors have any potential conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


