All published articles of this journal are available on ScienceDirect.
Eleven Year Results of Total Hip Arthroplasty in Patients with Secondary Osteoarthritis Due to Slipped Capital Femoral Epiphysis
Abstract
Background:
Total hip arthroplasty (THA) in patients with a history of Slipped Capital Femoral Epiphysis (SCFE), is typically indicated to address the consequent deformity of the proximal femur and/or acetabulum. It can be a challenging procedure for the orthopaedic surgeon. Previous studies have focused on prevention of osteoarthritis post-SCFE. However, there is a paucity of data on the outcomes of total hip arthroplasty in patients with osteoarthritis secondary to SCFE. This study was performed to assess the mid-term results of total hip arthroplasty in this patient cohort.
Materials and Methods:
All patients with secondary osteoarthritis due to slipped capital femoral epiphysis, treated with total hip arthroplasty between 1987 and 2005, were included in this retrospective study (n=30). Thirty patients (17 male, 13 female) met the inclusion criteria with one patient lost to follow-up and one unrelated death one year before follow up examination, thereby leaving 28 patients (32 hips) eligible for the study with a mean follow-up time period of 11.2 years. The Harris Hip Score (HHS) and MOS 36 short form health survey (SF36) were determined preoperatively and at most recent follow-up for all patients. Complications were also noted for all cases.
Results:
The mean Harris Hip Score increased significantly from 47 (32-59; SD=8.3) to 92.3 (65-100; SD=8.2) (p<0.0001). The SF-36 health survey showed an improvement of quality-of-life in all sub-scales. Overall, revision surgery was required in six cases (19 %). Aseptic loosening, leading to implant removal, was noted in five cases. A single-stage revision to address infection was performed in one case. The cumulative survival rate at latest follow-up was 81 %. No other complications were encountered during the study.
Conclusions:
Despite a higher failure rate, compared to total hip arthroplasty in the treatment of primary osteoarthritis, total hip arthroplasty can be considered a feasible option for patients with secondary osteoarthritis of the hip due to slipped capital femoral epiphysis. The current study demonstrates good outcomes in patients treated with a cementless column-preserving prosthesis, which is of particular relevance for this young patient cohort. However, further clinical prospective randomized studies are warranted to provide more definitive evidence.
INTRODUCTION
Slipped Capital Femoral Epiphysis (SCFE) is the most common hip problem in adolescence and is characterized by a slippage through the hypertrophic zone of the upper femoral epiphysis such that the femoral head remains in the acetabulum and the neck is displaced anteriorly and externally rotated [1]. Apart from pain in the groin, thigh or knee, limited internal rotation and flexion are typical clinical signs. Mechanical effects include unusual kinematics at the hip and femoro-acetabular impingement resulting in secondary osteoarthritis of the hip [2-4].
Early diagnosis and appropriate treatment are critical to prevent secondary complications of SCFE [5]. Secondary osteoarthritis of the hip, due to SCFE, usually occurs within the fourth to fifth decade [6-10]. Most of the studies have focused on the outcome after primary treatment in patients with SCFE. In-situ fixation has been the treatment of choice in the initial treatment of SCFE [6].
The current investigators report on patients undergoing total hip arthroplasty to address secondary osteoarthritis of the hip due to SCFE with a mean follow-up time of 11.2 years.
MATERIALS AND METHODS
All patients with secondary osteoarthritis of the hip due to SCFE, treated with total hip arthroplasty, in the authors´ institution, between January 1987 and September 2005, were enrolled in this retrospective study. Information about the patients’ medical history, age, and gender was obtained from the patients’ medical records. During this time period, a total of 36 patients (42 hips) with a background of SCFE, underwent THA. There were 20 male and 16 female patients, with a mean age of 43 years (17-58, SD=11.2). Either a cemented or non-cemented THA was performed on 22 right hips and 20 left hips, while six patients underwent bilateral THA. One patient died and another was lost to follow up. At time of follow up six patients had already undergone a revision procedure due to prosthetic failure and had to be excluded from the study. The mean body-mass index (BMI) was 28.8 kg/m2 (19.3- 41.9 kg/m2, SD=28.8). Before admission to the current authors‘ clinic, 24 patients had had a previous surgery performed including corrective osteotomy (n=10), pinning with K-wires (n=10) and fixation of the epiphysis with screws (n=4). In three patients, multiple surgeries were performed, while the remaining patients (n=6) were treated conservatively.
Surgical Technique
All surgeries were performed by experienced attending orthopaedic surgeons. Following appropriate positioning on the operating table in the lateral position, standard preparation and draping was performed. The exposure was achieved through a standard posterior approach in all cases. Either cemented or cementless THA were performed in all cases. Detailed information about the implants used and the postoperative course is given in Table 1.
Implant and Postoperative Course Data
| Implants | Type | Number | Postoperative Course |
|---|---|---|---|
| Cemented | SPII stem Mark III cup | 13 | Full weight bearing |
| Hybrid | SPII stem, T.O.P. cup | 11 | Full weight bearing |
| Uncemented | C.F.P stem, T.O.P. cup | 7 | Partial weight bearing 30 kg for 3 weeks postoperative |
The implants specified (SPII stem, CFP stem, TOP cup) are manufactured by Link (Waldemar Link, Hamburg, Germany).
Outcome Measures
Radiographic and clinical evaluations were performed preoperatively and at latest follow up (Figs. 1, 2). In all patients, the Harris Hip Score (HHS) and MOS 36 short-form health survey (SF36) was calculated on admission and at latest follow-up examination [11]. The SF-36 is a survey of patient health and consists of eight scaled scores including vitality, pain, general health perceptions, physical functioning, emotional functioning, social functioning, mental health and energy level.
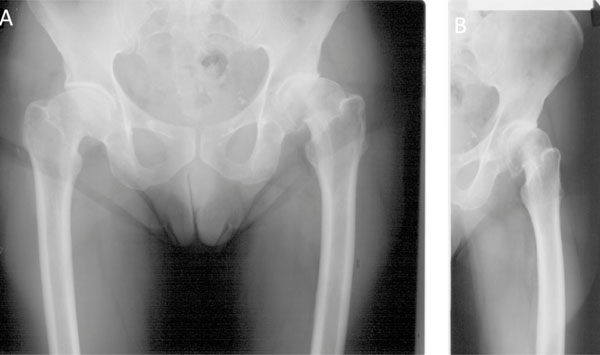
Pre-operative anteroposterior radiograph of the pelvis showing a severe slipping angle.
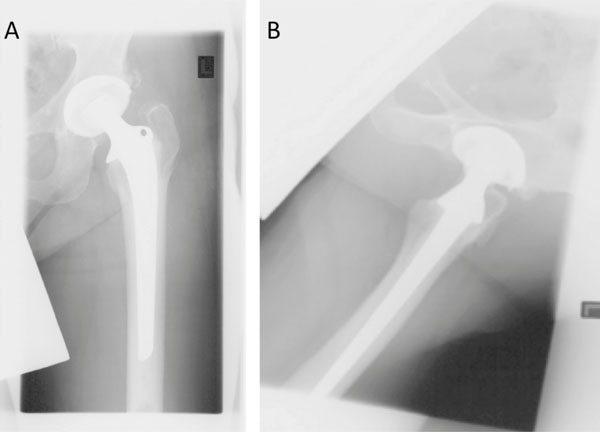
Anteroposterior radiograph at 9.6 years follow-up with no signs of loosening evident
Standard radiographs were analyzed based on cup position and inclination, osteolysis, radiolucent areas and limb-length discrepancy at latest follow-up. Limb-length discrepancy was measured on the anteroposterior radiographs of the pelvis as the distance between the inter-teardrop line and the tip of the lesser trochanter. Cup orientation was measured on the anteroposterior pelvic radiographs as the angle between the interteardrop line and the edge of the cup [12]. A femoral stem was considered to be in varus or valgus if the angle described by the intersection of the axis of the stem and the axis of the femoral shaft was >5°. Osteolysis around the cup was defined as a scalloped erosion exceeding 2 mm in diameter at the bone-prosthesis interface; the progressive widening of radiolucent lines >2 mm, migration of >2 mm, or 5° of cup tilting were defined as cup loosening [13]. Osteolysis around the cementless stems was evaluated according to the criteria of Engh et al. [14]. Osteolysis around the cemented stems was assessed according to the method described by Gruen et al. [15]. Subsidence of +/- 2 mm and/or varus or valgus tilting were considered signs of stem failure [13]. All complications related to the prosthesis such as aseptic and septic loosening, infection, dislocation and operative revision were documented in all cases.
Statistical Analysis
All variables were expressed in terms of mean and ± standard deviation (SD) of the mean. A Student’s t test was performed when the data had a normal Gaussian distribution; otherwise the Mann-Whitney test was employed for non-parametric data. The Shapiro-Wilk normality test was performed to ascertain whether the data were normally distributed. The Kaplan-Meier method was used to calculate prosthetic survival, with revision for any reason as the end point. Statistical analyses were carried out using a statistical software package (GraphPad Prism, Version 5.0d for Mac OS X, GraphPad Software Inc., La Jolla, CA).
RESULTS
Thirty-six patients (20 male, 16 female) were included in this retrospective study, with one patient dying prior to follow-up, one patient lost to follow-up and six patients with failure, leaving 28 patients (32 hips, 16 male, 12 female) available for follow-up examination with a mean follow-up time of 11.2 years (8-24 years; SD=3,6).
At the time of latest follow-up, the average HHS increased, in a statistically significant fashion, from 47.0 (32-59; SD=8.3) to 92.3 (65-100; SD=8.2) (p<0.0001). SF 36 health survey showed improvements in all sub-scales. A significant improvement in quality-of-life was noted post-operatively.
A total of six failures (3 male, 3 female) were noted at latest follow-up examination. In one case, revision surgery was required nine months after THA due to infection. The remaining five patients underwent revision surgery due to aseptic loosening (Table 2). The cumulative survival rate at latest follow-up was 81% (Fig. 3). Three of the six failed cases had been treated conservatively prior to THA and the remaining three had had a previous THA performed.

The Kaplan-Meier survivorship graph with revision for any reason as the endpoint. The blue line shows the overall survival rate, while the red line shows the survival rate of uncemented THA, at latest follow-up.
THA Failure Data
| Gender | Age at Diagnosis (y) | Age at Implantation (y) | Primary THA Design | Time to Revision (Months) | Previous Surgery | Reason for Revision | Revision Design |
|---|---|---|---|---|---|---|---|
| m | 9 | 50 | Cemented (SPII, MarkIII) | 47 | N | aseptic loosening stem | ENDO MODULAR |
| w | 14 | 31 | Hybrid (SPII; TOP) | 63 | n | aseptic loosening stem | Zweymüller |
| m | 14 | 47 | cemented (SPII; MarkIII) | 9 | n | prostethic infection | SPII, Mark III |
| w | 14 | 37 | Hybrid (SPII; TOP) | 72 | y | aseptic loosening stem | ENDO MODULAR |
| m | 17 | 48 | cemented (SPII; MarkIII) | 31 | y | aseptic loosening cup | MARK III |
| w | 10 | 19 | cementless (CFP; TOP) | 65 | y | aseptic loosening cup and stem | SPII, Mark III |
Two stems (6.3 %) were aligned in a varus position and five stems (15.6 %) in a valgus position. The remaining 25 stems (78.1 %) were implanted in a neutral position. The average acetabular cup orientation was 44.2° (30-54°; SD=7.1). In three cases, cup abduction was out of the optimal range of 40°±10°. All of the stems were stable without signs of subsidence, tilting or radiolucency. All but one of the cups appeared to be osseointegrated without evidence of osteolysis. This cemented cup showed an radiolucent line <2 mm. No other signs of migration or radiolucency were found in any implant.
The mean preoperative limb-length discrepancy was 13.5 mm (0-30 mm). A mean postoperative limb-length discrepancy of 4.5 mm (0-12 mm) was noted. No complications such as sciatic nerve palsy, fractures or hematoma were found.
DISCUSSION
The aim of the present study was to assess the mid-term results of THA in patients with secondary osteoarthritis of the hip due to SCFE. The data demonstrates that standard THA is a good treatment option for patients with osteoarthritis of the hip secondary to slipped capital femoral epiphysis. The mean survival rate was 81 % after 11.2 years (Fig. 3) which is higher than previous reported studies [16,17]. Nizard et al. reported on the outcomes after THA in younger patients with previous SCFE (n=12) [17]. The survival rate after eight years was 64.9 % less in this patient cohort [17]. Larson et al. described a survival rate of 50 % after 11.6 years in patients with SCFE [16].
Boyle et al. reported on the outcomes of THA in patients with primary osteoarthritis compared to those with secondary osteoarthritis due to SCFE. In this study, there were no siginificant differences for the revision rate nor the Oxford Hip Score (OHS) in both groups. The mean survival rate was approximately 95 % after 4.4 years [10]. A limitation of that study was the short follow-up time period. The current investigators report on patients undergoing total hip arthroplasty to address secondary osteoarthritis of the hip due to SCFE with a mean follow-up time of 11.2 years. Moreover the current study shows similar results in patients treated with a femoral neck preserving prosthesis (CFP prosthesis) with a mean survival rate of 92 % after 9 years (Fig. 3).
The mean age in the current series was 43 years at initial implantation, comparable to previous studies [6-9]. However, the mean interval between initial diagnosis and joint replacement was slightly longer compared to other studies. Larson et al. found that patients with severe displacement of the femoral epiphysis have a higher risk of avascular necrosis of the femoral head resulting in a remarkably shorter time interval between initial diagnosis and treatment of SCFE and/or joint replacement. In the present study, the authors did not encounter a higher incidence of avascular necrosis of the femoral head. The time interval between first diagnosis and treatment of SCFE and joint replacement was higher in the current series compared to the study by Larson et al. [16].
Interestingly, the rate of neurological complications in the current study was lower than historically reported in primary total hip arthroplasty [18]. A higher rate of nerve palsies associated with limb lengthening and extended soft-tissue releases, due to previous surgical treatment, is observed [19]. However, the current investigators believe that the posterior approach to the hip decreases the risk of sciatic nerve injury via direct visualization of the nerve intraoperatively.
Limitations of the current study include the fact that the study was retrospective in design, the patient number enrolled was relatively low and there was significant heterogeneity amongst the patient cohort.
Overall, the current authors believe THA to be a feasible treatment option in young patients with secondary osteoarthritis of the hip due to SCFE. The current study demonstrates satisfying mid-term results after 11.2 years. Some authors recommend hip resurfacing for patients with secondary osteoarthritis of the hip due to childhood hip diseases because of their younger age and the high activity level of these patients [20]. However, hip resurfacing does not restore anatomical hip biomechanics and limb length in patients with SCFE.
In conclusion, the results of the present study support standard THA for the treatment of osteoarthritis of the hip secondary to SCFE.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


