All published articles of this journal are available on ScienceDirect.
A Rare Periosteal Diaphyseal Lesion of the Ulna
Abstract
Periosteal lesions of the ulna diaphysis are rare, include a wide spectrum of tumors, and may cause considerable diagnostic problems. Surgical treatment may vary widely, based on an accurate diagnosis. We present the case of a periosteal, extraskeletal low grade myxoid chondrosarcoma of the ulna diaphysis. The surgical therapy included an en-bloc resection with allograft reconstruction. The patient showed a favorable outcome. Careful preoperative evaluation and planning are imperative to obtain a satisfactory oncological and functional outcome, especially with uncommon tumor presentations at rare locations.
INTRODUCTION
A large variety of tumors and tumor-like lesions originate from the outer surface of the cortex. Periosteal (or juxtacortical) tumors as primary surface lesions arise from the periosteum or the soft tissue in the immediate proximity of the cortex of the bone. Any of the mesenchymal elements present along the bone surface or the pluripotent cells found in the periosteum may give rise to these surface lesions. The most common types are those producing cartilage or bone; however, metastasis, tumors originating from blood vessels, fibrous or fat tissue can also be found [1]. In most cases, it is difficult to determine whether the lesion is of sole periosteal origin or arose from other connective tissue with secondary involvement of the periosteum [2]. Diagnosis might be difficult, as surface lesions of the bone are an uncommon entity and show different characteristics as compared to their intramedullary counterpart [2]. Besides a thorough patient history, imaging together with a biopsy is needed to establish a correct diagnosis. Patients often present with a long history of swelling and pain. If present, pain may result from mechanical irritation, bursitis, compression of nerves and vessels or fracture of the bone [3-5].
The ulna is an unusual site for primary tumor involvement. Primary lesions of this bone account for less than 1% of all skeletal tumors and less than 2% of all long bones, with malignant tumors being even rarer [1, 5, 6]. In our series of more than 2500 neoplasms and tumor-like lesions, the ulna is the primary site in 27 cases. Out of these, three cases were localized periosteally, in the diaphysis of the ulna. Few reports about periosteal ulna lesions are described in the literature, involving most commonly the distal part of the ulna.
We report the case of a rare diaphyseal periosteal ulna lesion with emphasis on clinical, radiological and histopathological aspects, as well as surgical treatment. For satisfactory oncological outcome, treatment must be individualized for each patient.
CASE PRESEANTATION
A 61-year-old woman presented with a 1 month history of intermittent paraesthesia of the left hand and painless swelling of the left forearm, painful only upon pressure. There was no history of trauma at that site. A portocaval shunt was established due to cryptogenic liver cirrhosis decades ago. The patient had been on the transplantation list but was subsequently removed due to stabilization of her liver function at a sufficient level. She had a history of an esophageal bleeding, a gallbladder operation, an appendectomy and ovariectomy, and a hysterectomy due to leiomyomas (in her twenties and thirties). A family history of liver disease was noted.
She denied fever, chills, night sweats and weight loss. Physical examination revealed an 8x5x3cm prominence over the palmar aspect of the ulna. Arterial pulses were present, and no motor or sensory deficits were elicited on examination. The range of motion of the wrist and elbow joints was normal. Plain radiographs of the left forearm showed a diffuse osteolytic lesion with a broad zone of transition and adjacent cortical thickening in the diaphysis of the ulna (Fig. 1A). Magnetic resonance imaging (MRI) revealed a soft tissue tumor with an intraosseous expansion into the ulna (Fig. 1B). A central signal enhancement suggested liquid or a myxoid substance. Chest-CT was normal. Percutaneous core biopsy specimens were histologically and immunohistochemically processed and the diagnosis of a low grade myxoid chondrosarcoma was established. The patient underwent en-bloc resection of the tumor (Fig. 1C) with segmental resection of the ulna and allograft reconstruction (freeze dried fibula) of the ulna defect which was spanned with a LC-DC plate (Fig. 1D). The histopathological examination revealed marginal resection with no tumor tissue in the soft tissue and bone resection margins. One day postoperatively a revision operation due to developing compartment syndrome had to be performed. The patient recovered immediately after the operation without any neurological and motor deficits. Histologically, the periosteal tumor showed a predominance of myxoid substance consisting of cords, nests and clusters of monomorphic small cells (Fig. 1E). Cortical erosion as well as focal extension into the adjacent bone marrow was demonstrated. Cytogenetically a complex abnormal clone was detected, containing at (9;22) translocation typical of myxoid chondrosarcoma among other structural aberrations [7]. The diagnosis of a periosteal, extraskeletal low grade myxoid chondrosarcoma was established. At a 4 month follow-up the patient complained of dysaesthesia of the wrist and across the diaphyses of the ulna. A plain radiograph showed ulna plate loosening. A MRI of the forearm showed no signs of recurrence. A re-osteosynthesis with cement augmentation of the three most distal screws and compression of the proximal allograft to bone transition was performed. At 24 months follow-up, the patient remained free of symptoms and on plain x-rays there were no signs of recurrent or metastatic disease. Radiologically the allograft was incorporated and remodelled, no plate loosening was evident.
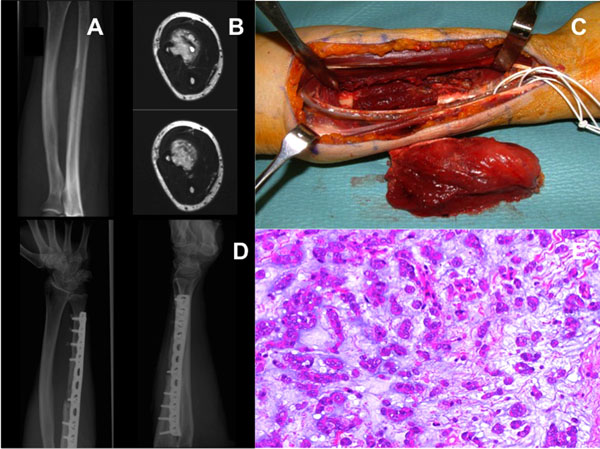
(A-E) This radiograph was taken at initial presentation. The patient complained about a swelling which was tender to palpation, as well as paresthesia of the hand. It revealed a diffuse erosion in the ulna diaphysis with a broad zone of transition and adjacent cortical thickening (A). The MRI showed a soft tissue tumor with central signal enhancement (liquid or myxoid) and an intraosseous expansion (B). This shows the intraoperative situation with a segmental en-bloc resection of the ulna, before the allograft (fibula) and plate reconstruction was performed (C). Postoperative radiograph shows allograft incorporation and plate stabilization (D). The histological specimen revealed a low grademyxoidchondrosarcoma consisting of myxoid extracellular matrix with embedded cords and clusters of monomorph neoplastic cells (hematoxylin and eosin staining; original magnification 200x) (E).
DISCUSSION
We present a patient with a rare periosteal, extraskeletal low grade myxoid chondrosarcoma of the ulna diaphysis. This location is exceedingly rare for a primary tumor site, and this biological entity has never been described for this anatomical location.
Radiologically, lesions that arise within the cortex have to be distinguished from lesions that affect the cortex. Medullary processes that expand slowly may cause scalloping at the inner border of the cortex or lead to considerable ballooning of the bone. More aggressive lesions generally grow faster than the periosteum's ability to lay down new bone. The periosteal reaction will then be laminated or disrupted. Even more aggressive lesions are characterized by a sunburst pattern or even amorphous osteolysis without any periosteal reaction. The type of periosteal reaction is an indicator of the speed of growth and infiltration of a lesion. Therefore, it is an indicator of the aggressiveness of the lesion. It is, however, not possible to decide whether a lesion is benign or malignant based upon the periosteal reaction. Lesions arising outside the bone in the periosteum or in the surrounding soft tissue are characterized by erosions of the outer aspect of the cortex. Thus, in case of any doubt, a biopsy for histological diagnosis is obtained to plan and adjust the treatment.
The resection and reconstruction of diaphyseal lesions spares the proximal and distal joints and allows excellent long-term results whereas the reconstruction of a large defect with a significant bone loss can leave the surgeon with greater choice of materials and techniques.
For our patient, we had to resect and reconstruct a segmental part of the ulna. Vascularized bone grafts allow a quicker union and greater cell preservation and are indicated for large defects or irradiated tissues [8]. For the reconstruction of the upper extremity, vascularized fibulas are generally recommended. Despite obvious advantages, vascularized grafts are technically more difficult and require a relatively long operative time, a risk of postoperative complications, including thrombosis of the anastomosed vessels, fracture or delayed union of the graft, and the possibility of infection. Additionally one has to consider the disadvantage of donor-site morbidity in a patient who is often already significantly impaired [9, 10]. Non-vascularized autografts are another reconstructive option that can successfully be used to reconstruct large bone defects. Allografts provide a permanent biological solution without donor-site morbidity but can incite an immune response and may transmit infection [11, 12]. Freeze dried allograft reduces the immunogenic response but also decreases strength. Therefore, one has to consider an additional osteosynthesis to decrease the risk of graft fracture. For our patient, we have chosen an en-bloc resection of the tumor with segmental resection of the ulna and allograft reconstruction using a freeze dried fibula allograft.
This is the first case of extra skeletal myxoid chondro sarcoma of the ulna. Only careful radiological and histological evaluation allowed accurate preoperative planning. Malignant tumors should be considered also for rare locations with “ atypical” presentation.
CONFLICT OF INTEREST
Declared none.
ACKNOWLEDGEMENT
Declared none.


