All published articles of this journal are available on ScienceDirect.
Update on the Management of Open Lower Limb Fractures
Abstract
Open lower limb fractures pose a significant challenging pathology for orthopaedic and plastic surgeons to manage due to the combined soft tissue damage, bone loss and potential vascular compromise. These fracture require extensive team-work and expertise between several surgical specialties and the advice of non-surgical specialties to ensure good clinical outcomes. Extensive research has improved the outcomes of open lower limb fractures and current recommendation on the optimal management is always being updated to enhance patient outcomes. This review serves to provide an overview of the management of open tibial fractures using current evidence and recently updated UK guidelines. The optimal time for surgical debridement, surgical intervention, providing antibiotics and soft tissue coverage will be outlined as well as the indications for amputation.
INTRODUCTION
Open lower limb fractures are often complicated injuries to manage and require joint surgical experience and expertise from plastic, orthopedic and vascular specialists due to the associated soft-tissue damage and musculoskeletal injuries. Open fractures of the lower limb require immediate examination, stabilization, systemic antibiotics, debridement and irrigation followed by timed soft tissue coverage and extensive rehabilitation. This review aims to explain the new guidelines regarding open lower limb fractures highlighting a number of important issues including examination of fractures, use of antibiotics and timing of debridement and surgical intervention.
There have been several classification systems used to grade open tibial fractures to guide severity to ensure appropriate management. The most widely used system is the Gustilo and Anderson score which is based on three factors (1) size of the open wound (2) degree of contamination (3) extent of soft tissue injury as shown in Table 1 [1]. The Gustilo and Anderson system has found to have poor interobserver reliability especially among inexperienced surgeons [2] However, due to its simplicity the Gustilo and Anderson Score is still recommended for daily use to grade the severity of open fractures [2]. Other systems such as the AO system though more comprehensive are found not to be user friendly and therefore recommended only for audit purposes [3].
Gustilo and Anderson Classification of Open Fractures
| Grade | Criteria |
|---|---|
| I | Open fracture, minimal contamination, comminution and soft tissue damage, wound <1 cm in length. |
| II | Open fracture, moderate contamination, comminution and soft tissue damage, wound >1 cm in length. |
| III | Open fracture extensive contamination, comminution and soft tissue damage. |
| IIIA | Type III fracture with adequate periosteal coverage of the fracture bone despite the extensive soft-tissue laceration or damage. |
| IIIB | Type III fracture with extensive soft-tissue loss and periosteal stripping and bone damage. Will need further soft-tissue coverage procedure. |
| IIIC | Type III fracture associated with an arterial injury-requiring repair, irrespective of degree of soft-tissue injury. |
The management of open lower limb fractures is important to standardize as much as possible as district hospitals manage an average of 250, 000 open tibial fractures a year of which 25% of these will be open [4, 5]. Therefore, the British Orthopaedic Association (BOA) and the British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS) have worked together to create guidelines to ensure the management of open lower limb fractures is standardized in the UK to improve patient outcomes [3]. In 2007 the two parties met together to increase the awareness of these injuries and to update the management of such fractures [3]. The British Infection Society and the Association of Medical Microbiologists were also asked to attend to ensure antibiotic prophylaxis for open fractures is adequate [3].
The literature highlights that surgical experience coupled with good multidisciplinary team working leads to good outcomes for patients in many conditions including polytrauma and complex lower trauma [6]. The treatment of open fractures must therefore involve a multidisciplinary team involving a teamwork of orthopaedic and plastic surgeons [3]. A hospital that cannot provide this level of expertise for their patients should ensure they are transferred to another hospital so the surgical treatment can take place in the specialist centre [3]. The UK guidelines have illustrated certain characteristics of open injuries that require patients to be transferred to specialist centers which include; (1) fracture patterns with transverse or short oblique tibial fractures with fibular fractures at a similar level (2) tibial fracture with comminution/butterfly fragments with fibular fractures (3) segmental tibial fractures (4) fractures with bone loss (5) soft tissue injury with skin loss that direct tension free closure is not possible following wound excision (6) degloving (7) injury to more than one arteries of the leg (8) injury to muscles which require excision of devitalized muscle via wound extensions [3].
IMMEDIATE MANAGEMENT ON PRESENTATION TO ACCIDENT AND EMERGENCY DEPARTMENT
Patients with these injuries must be assessed and managed appropriately based on the Advanced Trauma Life Support (ATLS) principles [7]. Having such major musculoskeletal injuries suggest that these patients have undergone significant amount of force during trauma, hence appropriate assessment and management are very important to identify any other potential threats to life or limb as well as to prevent complications [7]. The priorities of resuscitation remain the same with both primary (ABCDEs) followed by secondary survey [7]. After life threatening injuries have been ruled out careful examination of the wound can be carried out as shown in Fig. (1) [3]. It is important to obtain the maximum amount of information regarding the mechanism of injury to obtain an idea about the amount of energy transferred. A high index of suspicion of tibial fractures includes history of motor vehicle injuries, pedestrian injuries, a fall from a height, missile injuries, entrapment injuries as well as lower limb ischemia [7]. History regarding environmental exposure to foreign material or farmyard soil is important to recognize any potential pathogens for example clostridium perfringens [8]. Examination should include starting to examine the skin for crush or burst wounds, imprints, large or multiple wounds and closed de-gloving injuries [7]. Signs of compartment syndrome should be investigated as well as signs of vascular injury and nerve injury.
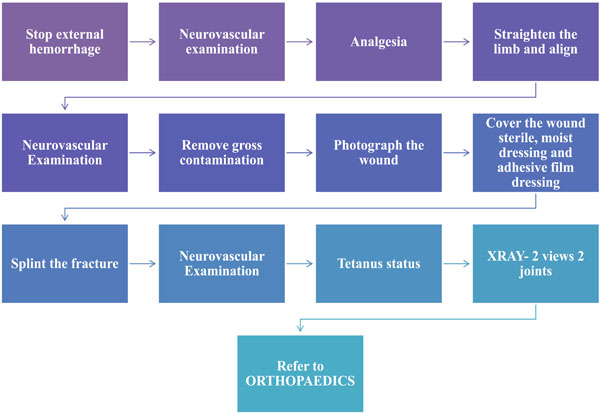
Method of managing open fractures in the accident and Emergency Department [3].
ANTIBIOTIC PROPHYLAXIS
Open lower limb fractures are often complicated by microbial contamination [1, 9]. The potential risk of infection and type of microorganisms often depends on the severity of associated soft tissue damage [10]. Many studies have been published on the correct surgical antimicrobial prophylaxis for lower limb fractures. A recent Cochrane review highlighted that antibiotic prophylaxis is vital to be initiated immediately but the exact type and duration of antibiotics is not so clear [11]. The administration of antibiotics was found to reduce the risk of infection by 59% [11]. Jaeger et al., 2006 assessed the national Scottish and Swedish-Norwegian guidelines and the proposed German recommendations [12]. After reviewing the guidelines the authors recommended 24 hours of antibiotics following type I and II gustillo fractures but 72 hours for grade III or not more than 24 hours for soft tissue injuries [12].
Blood cultures have not found to be useful as Lee showed that only 8% of 226 organisms grown on culture caused the infection in a series of tibial injuries [13]. Therefore, the overall opinion is that cultures offer unneeded contamination and likely show skin flora [13]. It has been found that most open fractures infections are caused by gram-negative rods and gram-positive staphylococci and so antibiotics should cover both species [13, 14]. However, recently MRSA has found to be associated with open lower limb fractures in some series. The optimal antibiotic regime to combat the infection rate with open fracture is not clear from the literature. Patzakis et al., showed that first generation cephalosporin, cephalothin has a lower infection rate compared to those receiving penicillin and streptomycin (2.3% compared to 9.7%) [15]. Many studies have shown all open fractures should be treated with combination of a first-generation cephalosporin and an aminoglycoside [16]. However, other studies have advocated only adding aminoglycoside for type III fractures [17]. The literature also states that penicillin or ampicillin should be used if there is considered to be a high risk of anaerobic infection [18].
Over the last ten years, interest has grown in the use of local antibiotic therapy to prevent infection after open fracture [19]. Local therapy has shown to keep the optimal antibiotic therapy within the wound but reduce the risk of systemic side effects [19]. One way of performing this is by incorporating a heat resistant antibiotic in polymethyl-methacrylate cement, which is then placed in the wound cavity covered by a semi-permeable membrane [3]. Recently, aminoglycoside-eluting polymethyl-methacrylate beads have been studied by Ostermann et al., showing that 1085 open fractures treated with tobramycin-eluting beads had a significantly lower rate of infection compared to those not treated with the beads [20]. A recent study compared local and systemic antibiotic therapy in the management of type-II, IIIA, and IIIB open fractures [21]. The findings illustrated similar rates of infection between local therapy with tobramycin-eluting beads and systemic therapy with a first-generation cephalosporin [21]. Antibiotic bead pouches have been advocated by the British guidelines when there is a segmental bone loss, gross contamination or established infection to decrease infection rates [3].
Due to the overwhelming evidence, antibiotics have been advised to be administered as soon as possible after the injury, and certainly within three hours [3]. The evidence to date supports the use of first generation cephalosporins [3]. However, within the UK this group of antibiotics is avoided due to the associated Clostridium difficile related diarrhoea [3]. Unfortunately, evidence is limited with regards to non-cephalosporin activity and therefore guidelines are based on microbiological principles and the likelihood the patients will be exposed to hospital organisms including staphylococci, coliforms and pseudomonads as shown in Table 2 [3].
Antibiotic Classification from BAPRAS Guidelines [3]
| Indication | Antibiotic |
|---|---|
| Until first Debridement | Amoxiclav (1.2g 8 hourly) Cephalosporin (1.5g 8 hourly) |
| At first debridement continued until soft tissue closure or max of 72 hrs | Co-amoxiclav (1.2g) or a cephalosporin (such as cefuroxime 1.5 g) and gentamicin (1.5 mg/kg) |
| Induction of anaesthesia at the time of skeletal stabilisation and definitive soft tissue closure. | Gentamicin 1.5 mg/kg and either vancomycin 1g or teicoplanin 800mg. Not be continued post-operatively. |
| Anaphylaxis to penicillin | Clindamycin (600mg iv pre-op/qds) in place of co-amoxiclav/cephalosporin |
OPERATIVE TIMING GUIDELINES
Historical management and two studies favoured wound debridement within 6 hours of the injury [22, 23]. Kreder and Armstrong studied 56 open fractures, which illustrated that debridement of less than 6 hours decreases the infection rate from 25% to 12%. [24]. The second study by Kindsfater and Jonasse showed operative treatment within 5 hours was associated with a lower risk of infection [25]. However, many studies have recently brought the ‘6 hour’ window into question and found no association between rate of infection and timing of debridement [26-29]. Harley et al., found no increase in infection rate or non-union rate when debridement took place up to 13 hours [26]. The study also highlighted that the strongest predictor for risk of deep infection rate was the grade of the fracture [26]. Patkins and Wilkins further confirmed that the greatest determinant was the timing of antibiotics and not delay to debridement of greater than 12 hours [27]. Naique et al., compared debridement for open fractures up to 6 hour and then between 6 and 24 hour and illustrated no difference in infection rates [28]. Lastly an extensive review of the literature by Crowley investigating the timing to intervention showed the 6 hour rule needs to be re-evaluated [29]. Due to the immense literature the new British guidelines have shown that debridement should be performed by senior orthopaedic and plastic surgeons and should be on a routine trauma emergency list within 24 hours of injury [3]. Although there are exceptions where immediate surgery should be undertaken including if there is gross contamination, devascularisation or compartment syndrome [3].
PRINCIPLES OF WOUND DEBRIDEMENT
Early accurate debridement is the most important surgical procedure for open lower limb fractures [1, 8, 10]. Debridement involves excision of all devitalized tissue apart from the neurovascular bundles [1, 8, 10]. After the limb is cleansed with soap solution the tissue must be assessed form superficial to deep structures [30]. It is important that the areas, which are not apparent from external view, are inspected carefully, via appropriate wound excisions to find hidden damage [31]. Devitalized muscle is assessed by looking for the four C’s: colour, contraction, consistency and capacity to bleed [31]. A secondary wound debridement should only be carried out if the soft tissue damage is unable to be assessed [32]. Serial multiple debridements have shown to be associated with poor outcomes [32]. The wound should be left in a condition that elective surgical procedures is possible including internal fixation or flap closure [3]. The wound must be extended along its nearest fasciotomy incision to gain an adequate view [3]. Dirt and debris should be removed with periodic irrigation and suction [30]. Loose fragments of bone, which are avascular do not contribute to fracture union and serve as a source of infection and should be removed [32]. Lavage entails the removal of meticulous foreign material, non-viable bone and soft tissue [30]. It is recommended to use warm saline to complete the debridement of the bone with no added advantage of using antiseptics or antibiotics [33].
If soft tissue debridement is not carried out immediately with debridement then the wound should be covered with a temporary dressing, this aims to prevent bacterial inflow and desiccation [34]. Negative pressure dressings offer an ideal dressing in form of the Vacuum Assisted Closure (VAC) device to prevent bacterial inflow [34]. De Franzo et al., demonstrated in 75 patients with open fractures that VAC dressings prevented the desiccation of the cortical bone [35]. Negative pressures dressing have shown to decrease the infection rate in closed open fracture when applied before closure of the elective surgical incision after internal fracture fixation [36]. It is advised that the VAC device is useful and safe in open management until definitive cover is needed [3].
SURGICAL STABILIZATION OF OPEN TIBIAL FRACTURES
The optimal surgical fixation technique for open tibial and femur fractures remains an ongoing controversy. There are many ways of stabilizing the fracture which include external fixation, plates and screws and reamed and undreamed locking nails.
Provisional Stabilization
It is important that external fixation is applied despite a more stable form of definitive stabilization being substituted at a later date [37, 38]. Early stabilization is important to restore alignment of the limb, limit the extent of soft tissue damage and reduce gross movement at the site of the fracture [37]. This will enable better blood flow, and reduce postoperative pain and stiffness [38]. Traction or long plaster slabs are not recommended for provisional stabilization [3]. Spanning external fixation is advised when stabilization has not been carried out at the time of primary debridement [3]. The placement of pins in the tibia must take into account the fracture pattern, the prospective plastic surgical procedure and the necessity to span the ankle and knee [39].
Definitive Stabilization
Many factors determine whether stabilization should be carried out with internal or external fixation but internal fixation should be considered as soon as possible [37, 38]. The anatomy of the fracture determines the type of internal fixation [3]. Diaphyseal injuries with minimal bone loss are suited to intramedullary nails (IM) but articular fracture have a better outcome with plates [3]. Injuries with significant bone loss including articular fractures, complex multilevel fracture or those with ankle or knee joint instability all do better with external fixation [3]. If internal fixation is used than definite cover should be carried out at the same time as delayed cover with internal fixation lead to increased infection rates [40]. The timing of conversion to internal fixation is trial under debate [40]. Overall external fixation is better when there is significant amount of bone loss with smaller losses being managed by internal or external fixation procedures [3]. Internal fixation should not be used in highly contaminated injuries [3]. The creation of dead space from either the debridement procedures or the injury itself will create dead spaces, which will determine the type of internal stabilization procedure that it used [3].
TYPES OF INTERNAL FIXATION
Early management is advised for femur fractures to improve patient outcomes [41]. Bone et al., illustrated with a prospective randomized controlled still comparing early and late stabilizing of 178 open and closed femoral fractures [41]. When stabilization was performed within 24 hours there was decreased pulmonary complications, shorter hospital stay and less time in intensive care unit [41]. Most surgeons advocate early intramedullary nailing with reaming with literature supporting this approach. Immediate and delayed intramedullary nailing has been compared in one prospective study of 27 primary and 15 delayed intrameduallary nailing patients which found no difference in incidence of infection, malunion, nonunion, or the time to union [42]. The authors advised primary reamed intramedullary nailing is an effective treatment alternative for the patient with multiple injuries, regardless of soft tissue injury, including Grade III wounds [42]. Few other papers support that primary intramedullary nailing provides good outcomes with no added risk of infection but further study is needed [43, 44]. Few papers describe the advantage of external fixation for definitive treatment of open fractures of the femur [43]. Dabezies et al., showed that in 20 femoral fractures the overall rate of union was 100% with the required use of bone grafts in 15% of cases and deep infection complications were seen in 13.3% of cases and pin track infection only in 15% [43]. Malunion was seen in 23.3% and reoperation was found to be 17% [43]. These outcomes are not as good as intrameduallary nailing [43]. Plating for open femoral fractures is even less clear but some evidence has shown their use in grade-IIIC open fractures and unstable pelvic or spinal injuries [44].
The optimal treatment of open fracture of the tibia is less obvious from the literature. Intramedullary (IM) nailing remains to be a popular choice amongst surgeons in the treatment of open tibial shaft fractures. Bhandari et al., favoured unreamed nails in their systematic review article involving five randomized trials [45]. They investigated the rates of reoperation, nonunion and deep infection and concluded that the risk of reoperation was as high as 18% implying that one reoperation would be avoided with every six patients treated with IM nailing instead of EF [45]. They have also shown that there was a significant reduction in the risk of superficial infection comparing both groups, with one superficial infection avoided for every three patients threatened with IM nailing, without increasing the risk of nonunion and deep infection [45].
There is also a dilemma with regards to reamed or unreamed IM Nail. Theoretically, reaming of medullary canal with a placement of a larger nail has a result which will ensure better biomechanical stability [45-48]. Benefits of reaming also include increase in surrounding muscle and soft tissue blood flow, which has been demonstrated in multiple animal fractures model [46-48]. However, there is an ongoing concern with regards to destruction of endosteal blood supply as a result of reaming and it’s impact on bone healing in a background of already precarious blood supply due to traumatic soft tissue disruption [49]. Keating et al., compared reamed and unreamed nails and found no statistically difference between the two groups in terms of time to union, rate of union, infection and frequency of breakage of the nail [50]. There was no difference in terms of functional outcome in terms of return to work and recreational activity [50]. However, they did observe a significantly larger amount of broken screws in unreamed nails but no increased number of broken nails [50].
External Fixation (EF) has been very popular in the treatment of open tibial fractures [51]. It is relatively easy to use as has a much shorter operating time with limited effect on blood supply to tibia [51]. However, there have been concerns due to the high incidence rate of pin site infection and the potential risk of malunion [51]. Sarmiento et al., has reported a rate of as high as 33% of patients with malunion following treatment of tibial fractures with EFs and functional brace with a combination of shortening and angulations [52]. These patients were later offered an operation to correct the deformities [52]. There were also 2.5% patients who went on to nonunion [52].
External fixation has been compared to unreamed nailing in the literature. A recent meta-analysis showed no statistically significant difference between these two methods of stabilization with respect to union, delayed union, deep infection and chronic osteomyelitis [51]. External fixation was found to have a significant higher need for autologous bone grafting with an increased rate of malunion and further surgery [53]. Bhandari compared reamed versus external fixation from a number of prospective studies and found reamed nails significantly reduced the risk of re-operation when compared with external fixators but not that of deep infection or nonunion [45]. Few studies have looked at external fixation and delayed reamed intramedullary nailing with the idea that immediate intramedullary nailing posing an increased risk of septic complications [52-55]. Overall, the studies have shown that rate of deep infection was 17% and 2.5% developed chronic osteomyelitis with delayed union in 14% and malunion in 11% [54-57]. Inan et al., investigated the use of Ilizarov external fixator (IEF) in 61 patients and demonstrated a shorter time to union at 19 weeks for IEF and 21 weeks for IM nailing group [56]. They also reported complications such as pin tract infection, joint contracture in IEF group and osteomyelitis in the IM nailing group. There were four patients with malunion in both groups [56].
Plating of open tibia fractures are rarely used but is useful when secondary soft tissue procedures are needed [57]. One study compared external fixation and plate and screws [57]. Bach et al., showed in their randomized trial that 50% of patients treated by tibial plate required further operations as opposed to 6.7% in EF group [57]. They concluded that these fractures are better treated with external fixators than plating due to higher rate of failures of plate fixation such as deep infection, non-union and failures of fixations [57].
SOFT TISSUE RECONSTRUCTION
Adequate soft tissue cover is vital to ensuring an infection-free fracture union [58]. Caudle and Stern reviewed the outcomes of open tibial fractures and demonstrated muscle coverage within 5 days had lower rates of infection and increased rate of fracture union [58]. Small and Mollan et al., showed that early coverage within 72 hours had lower complications and infection rate to those reconstructed after 72 hours [59]. Sinclair et al., further supported early soft tissue reconstruction reporting a lower infection rate with definitive skeletal fixation and soft tissue reconstruction within 72 hours [60]. Hertel et al., compared the outcomes of patients who were reconstructed on the day of injury to patient who went reconstruction on average 4.4 days post injury [61]. Fracture union was greater and infection rate lower in the group that was treated on earlier [61]. It is clear the evidence highlights that soft tissue coverage should be carried out as soon as possible [58-61]. The terminology of ‘fix and flap’ is being recommended for specialist hospitals where the expertise is available but likely to be suited to the local flaps [3]. Complex reconstruction should only be undertaken when the patient has been prepared and examined and the specialist teams are able to work together [3]. However, definite soft tissue reconstruction should not be delayed beyond 7 days after injury [3].
ASSOCIATED VASCULAR INJURY MANAGEMENT
Devascularized limbs require urgent surgical exploration with the aim to restore circulation within 3-4 h of the injury to prevent muscle death [62]. This pattern of management was supported by Howard and Makin et al., who showed a 50% amputation rate in those revascularized after 8 hours [63]. Devascularisation is common in displaced fractures of the femur and posterior fracture dislocations [3]. Absent peripheral pulses and reduced capillary refill are indicators for vascular compromise and a senior surgical opinion must be sought [3]. Once the site of injury has been identified during surgical exploration, vascular shunts are used to restore vascularisation [62]. Angiography has found to cause unnecessary delay when managing such injuries [62]. If the limb is salvageable then the fracture can be stabilized with an external fixator before replacing the shunts with reversed vein grafts [64]. The presence of vascular injuries has shown to be predictive of the outcome of the tibial fractures in terms of fracture healing, infection and swelling [65].
INDICATIONS FOR PRIMARY AMPUTATION
The indications for primary amputation have decreased since the increase of modern surgical techniques [3]. The UK guidelines advocates very strict indications for amputation for example, avascular limbs which exceed 4-6 hours of warm ischaemia, for incomplete amputations where the limb is completely severed and when the distal portion is itself subject to significant trauma and extensive crush injuries [3]. Furthermore, amputation is advised to be considered only for limbs with segmental muscle loss with more than two compartments, segmental bone loss greater than one-third of the length of the tibia and open foot injuries with tibia fractures [3]. The literature has shown that the greater the ischaemic time the more likely that there will be significant muscle loss from necrosis [66] and therefore is it crucial to determine this information from the history [62]. Several other factors may be taken into account to determine the need for amputation. Recovery of normal plantar sensation is possible in over half of patients and cannot be assumed to be caused by nerve disruption so it not an absolute indication for Amputation [67]. The presence of soft tissue damage and loss needs to be considered as if muscle action spans several compartments then the likelihood of needing orthotics is needed [3]. The pattern and degree of severe bone loss may affect the decision to amputate with the need to consider the need for bone grafting or distraction osteogenesis [3]. When amputation is thought to appropriate transtibial or transfemoral are considered to be better options than above the knee in terms of energy expenditure [68]. Furthermore, long-term follow up has shown good outcomes in below the knee amputation in term of quality of life and the ability of patients to adapt to their new situation [69].
CONCLUSION
It is clear that open fractures still remain a challenging pathology for specialists to manage. However, with the extensive research that has and is being carried out and standardized guidelines now available, management is improving with the decreased need for damage control surgery. The literature clearly shows that antibiotics should be administered as soon as possible to improve clinical outcome [11]. The six-hour rule is no longer supported by current literature [26-29]. Early stabilization is advocated with the type of fixation depending on soft tissue management, degree of bone involvement and other factors [37, 38]. The most ideal method of definite stabilization is still under debate and further study to address this is needed.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


