All published articles of this journal are available on ScienceDirect.
Reproducibility of Newly Developed Spinal Topography Measurements for Scoliosis
Abstract
Objective:
In an effort to limit exposure to ionizing radiation and fully characterize three dimensional changes in the spine of patients with scoliosis reliable non-invasive methods of spinal back contour analysis (Milwaukee Topographic Scanner) (MTS) have been developed.
Study Design:
The current study compares spinal topography measurements among different subject positions and evaluates the reproducibility of the system for both inter-rater and intra-rater reliability.
Methods:
A dummy cast (plastic cast) of one patient with adolescent idiopathic scoliosis was created in order to test the reliability of the MTS. The dummy cast was positioned and rotated in 3D while scanned by two investigators using the MTS. A total of twelve parameters including Q-angle (an analog to X-ray’s Cobb angle) were extracted.
Results:
All measurements of intra-rater and inter-rater reliability were excellent (Intraclass Correlation Coefficients ranging from 0.89 to 0.99) with the exception of Pelvic Tilt (intra-rater ICC is 0.61) and lordosis angle (inter-rater ICC is 0.82). No significant variability among investigators was observed for all tested metrics. No significant variability due to position was observed for the majority of back contour measurements but there were significant changes in the T1-S1 angle, T1-S1 deviation, T1-NC angle, T1-NC deviation, and Back Height metric (p< 0.05).
Conclusions:
The MTS is a reliable method of raster stereography in the measurement of the back contour, which will help monitor the progression of children with idiopathic scoliosis and reduce the use of X-rays.
INTRODUCTION
Children with Idiopathic Scoliosis present with three dimensional deformities which are assessed by radiographic evaluation. This method of assessment does not account for three dimensional changes in the spine and exposes patients to ionizing radiation which has been shown to increase the risk of developing several types of cancers, including breast and thyroid cancers [1-3]. In order to address these issues, noninvasive methods of spinal curve analysis such as Moiré photography [4, 5], ultrasound-guided spine analysis (Zebris) [6], Integrated Shape Imaging System (ISIS) [7, 8], and the Quantec Spinal Imaging System (QSIS) [9-15] were developed. Although QSIS has been repeatedly studied and found to be a reliable and accurate measurement of spinal deformity, its use remains limited among practitioners [12-18].
The current Quantec system can be operated by nonspecialized personnel but data acquisition is tedious and time consuming; especially because the operating system is antiquated. To address these issues, we have developed a new user-friendly raster stereography system (Milwaukee Topographic Scanner, MTS) composed of a new software system, handheld light source, and hardware which can be easily transported among clinic rooms. The goal of the current study is to compare MTS measurements among different subject positions and to evaluate the reproducibility of MTS for both inter-rater and intra-rater.
MATERIALS AND METHODS
A dummy cast was created using a plastic model of one patient with adolescent idiopathic scoliosis. Optical color-coded markers were placed on each of the cast’s spinous process landmarks from T1 to L5 and at each posterior superior iliac spine (PSIS). The MTS is composed of measurement software, a sensor, a laser light, two cameras in one handle and hardware. Two investigators completed a series of three MTS scans of the dummy cast in each of four different positions (conditions): flexed 10° forward in the sagittal plane (10°F), flexed 20° forward in the sagittal plane (20°F), rotated 10° in the transverse plane (10T°), and “shaking” (SH) back and forth in the coronal plane for a total of 24 scans (12 scans per investigator). After each measurement was taken the dummy cast was rotated using a goniometer according to the aforementioned degrees. After scanning, 14 clinically relevant metrics and 3D back contour image were extrapolated from the MTS 3D data (Fig. 1A, B):
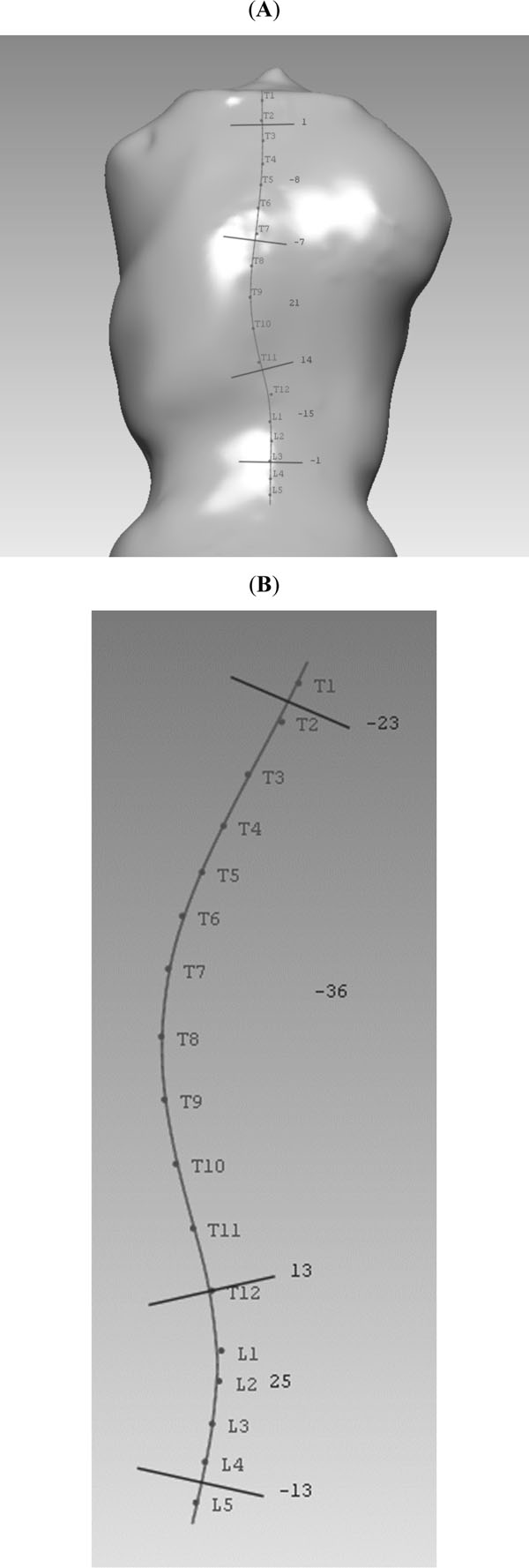
(A) A dummy cast with markers on the spinal process from T1 to L5 was scanned by the MTS system: three Q angles (8°, 21°, and 15°) are analogous to Cobb angles in the coronal plane; (B) Kyphosis (36°) and lordosis (25°) are analogous to Cobb angles in the sagittal plane.
- Q angle: maximum angle of tilt in the coronal plane, analogous to Cobb angle in the coronal plane (Fig. 1A);
- Area of Back: total back area between the T1 and T12;
- Area Percentage in left and right (%): Area of left or right side of back divided by a line from T1 to T12 vs total area of back then multiplied by 100;
- Area of Back ratio: area on the left vs on the right;
- Kyphosis/ Lordosis: maximum angle of tilt in the sagittal plane (T1-T12 for Kyphosis and L1-S1 for Lordosis), analogous to Cobb angle in the sagittal plane (Fig. 1B);
- Suzuki Hump Sum: Measurement of rib hump asymmetry based on three lateral cross sections. This measurement is indicative of transverse rotation [19];
- POTSI (posterior trunk symmetry index): Coronal plane measurement calculated by measurement of several variables including waist creases and shoulder heights [20];
- Volume of Interest (VOI): a measurement in the transverse (axial) plane from the most posterior point on each vertebral body perpendicular to a coronal vertical plane made by the shoulders;
- T1-S1 angle: the angle between the laboratory vertical and the anteroposterior projection of the line passing through T1 and S1[11];
- T1-S1 Deviation: the horizontal distance (mm) at S1 between the laboratory vertical and the anteroposterior projection of the line passing through T1 and S1 [11];
- T1-NC angle: the angle between the laboratory vertical and the anteroposterior projection of a line passing through the top of the natal cleft [11];
- T1-NC deviation: the horizontal distance at the natal cleft between the laboratory vertical and a line passing through the top of the natal cleft [11];
- Back Height: the distance between T1 and the bisector of the posterior superior iliac spines [11];
- Pelvic Tilt: the angle between the laboratory horizontal and the posterior superior iliac spines in the coronal plane (pelvic obliquity) [11];
Fixed effects repeated analysis of variance measurements (ANOVAs) were calculated for each of the 14 metrics. A separate ANOVA procedure was performed for each metric in order to assess variability due to each individual position condition (10°F, 20°F, 10T°, and SH) as well as trial and investigator variables. A statistical model was designed: where β0 defines overall intercept for the measured parameter, is a vector of 3 parameters adjusting our model for POSITION effect, β2 is INVESTIGATOR effect, β3 is the effect of replicating the measurement of the same INVESTIGATOR at the same POSITION, εijk is a measurement error following a normal distribution with a zero mean and an unknown variance σ2.
Intraclass correlation coefficients (ICC’s) were also calculated to assess contribution of intra-rater and inter-rater variability to total variability. The ICC value (1.0) is considered as highest reproducibility. P <0.05 was considered as significant difference.
RESULTS
No significant variability due to position, investigator, or trial was observed in the following metrics: Area of Back, Area%, Area Ratio, Kyphosis, Lordosis, Suzuki Hump Sum, POTSI, Volume of Interest, or Q-angle (Table 1). Q angle for the dummy cast curve (i.e., thoracic curve) was measured with the mean value of 19.3° (ranging from 16° to 22°). Differences of Q angles between the investigators was 1.5° (ranging from 0 to 3°) and differences of Q angles among trials was 1.4° (ranging from 0 to 6°) (Fig. 2). Significant variability due to position was observed in the T1-S1 angle, T1-S1 deviation, T1-NC angle, T1-NC deviation, and Back Height (p < 0.01, p = 0.03, p <0.01, p < 0.01, p < 0.001, respectively). Standard error (SE) for trial variability ranged from 0.1 (Area ratio) to 8.1 (POTSI).
Determinants of Significance (p Values) and Standard Error (SE) for Each Metric
| Metric | Determinants of Significance (P Values) | Standard Error (SE) **** | |||
|---|---|---|---|---|---|
| Position | Investigator | Trial | SE -Investigator | SE- Trial | |
| Q angle- thoracic curve | 0.55 | 0.94 | 0.76 | 0.93 | 0.93 |
| Q angle- thoraco-lumbar curve | 0.97 | 0.92 | 0.61 | 1.2 | 1.3 |
| Kyphosis | 0.06 | 0.07 | 0.69 | 1.9 | 1.9 |
| Lordosis | 0.31 | 0.09 | 0.36 | 0.9 | 0.9 |
| SuSzuki Hump Sum | 0.7 | 0.37 | 0.56 | 0.27 | 0.27 |
| POTSI | 0.24 | 0.4 | 0.37 | 8.1 | 8.1 |
| Volume of Interest | 0.03* | 0.25 | 0.84 | 0.6 | 0.6 |
| T1-S1 angle | <0.01** | 0.77 | 0.25 | 0.2 | 0.2 |
| T1-S1 deviation | 0.03* | 0.99 | 0.48 | 2.1 | 2.1 |
| T1-NC angle | <0.01** | 0.45 | 0.63 | 0.3 | 0.3 |
| T1- deviation | <0.01** | 0.45 | 0.7 | 2.4 | 2.4 |
| Back Height | <0.001*** | 0.87 | 0.56 | 0.82 | 0.82 |
| Pelvic Tilt | 0.39 | 0.92 | 0.03* | 3.35 | 3.35 |
* Indicates p< 0.05.
** Indicates p< 0.01.
*** Indicates p< 0.001.
**** SE for overall position is not reported as SE was determined for each tested position condition (10°F, 10°T, 20°F, and SH) separately.
Intraclass Correlation Coefficients for Intra-Observer and Inter-Observer in 14 Metrics
| Metric | Inter-Rater ICC | Intra-Rater ICC |
|---|---|---|
|
Q
angle-thoracic curve Q angle-lumbar curve |
0.99 0.99 |
0.99 0.99 |
| Area of Back | 0.90 | 0.99 |
| Area Ratio | 0.89 | 0.99 |
| Kyphosis | 0.99 | 0.99 |
| Lordosis | 0.82 | 0.99 |
| Suzuki Hump Sum | 0.99 | 0.99 |
| POTSI | 0.99 | 0.99 |
| Volume of Interest (VOI) | 0.99 | 0.99 |
| T1-S1 angle | 0.99 | 0.99 |
| T1-S1 deviation | 0.99 | 0.99 |
| T1-NC angle | 0.99 | 0.99 |
| T1-NC deviation | 0.99 | 0.99 |
| Back Height | 0.99 | 0.99 |
| Pelvic Tilt | 0.99 | 0.61 |

Changes of analogous to Cobb angle between investigators, trials, and different positions (mean value in degrees) (NEU = neutral position; I1T1/I1T2: investigator: for trial 1 or 2; I2T1/I2T2: investigator 2 for trial 1 or 2).
Significant variability was observed in the 20°F condition for the T1-S1 angle (p=0.002), T1-S1 deviation (p=0.01), T1-NC angle (p=0.02), and T1-NC deviation (p=0.02) metrics. Variability due to 10°F condition, the 10°T condition, and the SH condition were not significant in any of these metrics. With respect to the Back Height metric, all position variables (10°F, 20°F, 10°T, and SH) resulted in significant variability (p<0.0001 p<0.001, p<0.0001, p<0.001 respectively). Significant variability was also observed in the trial variable for the Pelvic Tilt metric (p=0.03). For the VOI metric, no significant variability was observed in the overall position variable but significant variability was observed in the shaking condition (p=0.03).
Intraclass Correlation Coefficients (ICCs) demonstrated inter-rater reliability of less than 1.0 for the following metrics: Area of Back, Area Ratio, and Lordosis (0.82-0.90) (Table 2). All other metrics of inter-rater ICC were equal to 0.99. With respect to Intra-rater ICCs, only the pelvic tilt metric was less than 1.0 (ICC=0.61). All other Inter-rater ICCs were equal to 0.99.
DISCUSSION
Our data indicate that the MTS is reliable and reproducible for the majority of the tested measurement parameters (Tables 1 and 2). Since the markers on the casting dummy remained in a constant position, variation in the measurements could be traced to differences in dummy position and investigator scanning technique. While several methods of raster sterography have been published, data from this study are most comparable to data reported for Quantec systems. Investigating QSIS measurements in 200 patients with idiopathic scoliosis, Wojcik et al. reported a SE for thoracic Q-angle of 4.8° while the thoracic Q-angle SE in our study was 0.93° [21]. Most notably, thoracic Q-angle SE reported in this study is less than SE in Cobb angle reported in the literature (SE=1.7°) [22]. Mean Q angle difference between the investigators (1.5°) and between trials (1.4°) regardless of position demonstrated that the measurement of curvature by the MTS can be reproduced by difference clinicians and is not limited by patient positioning. Additionally, no other parameters tested with the MTS demonstrated significant variability due to either trial or observer, with the exception of the Pelvic Tilt metric among trials. Variation in the Pelvic Tilt metric may be explained by variation in identification of the PSIS and is a limitation of the technique common to all rasterstereogrpahic technologies. However, identification of the PSIS is used only in this metric and has impact on spinal curve measurements.
Our data support previous research by Stokes and Moreland and by Liu et al. indicating that trunk position has an effect on surface topography measurements [10, 23]. In contrast, Sakka et al. found no variability in QSIS measurements due to trunk position [24], although different metrics were tested in each of these studies. In the current study significant variability due to position was observed in the T1-S1 angle, T1-S1 deviation, T1-NC angle, and T1-NC deviation metrics (p<0.01, p=0.03, p<0.01, p<0.01, p<0.001, respectively). This data supports that of Liu et al., who also reported significant variability in these metrics due to forward rotation [10]. However, this variability was only related to the 20°Foward position. This effect may be a result of the sensors which are placed on the subject’s back which decrease measurement noise and could result in dampening of variability caused by small changes in position.
Our data do not support previous research which indicates significant variability in the Kyphosis metric due to forward bending, indicating that the MTS is more reproducible with respect to this parameter than previous QSIS systems [10, 23]. Significant variability of VOI reported in the SH metric may be due to inconsistent manual movement of the dummy cast during testing and may also indicate the sensitivity of this metric to changes due to postural sway in the coronal plane.
Variability in the Back Height metric due to trunk position (p<0.001) has not been studied previously but variability in this metric with changes in position of the trunk is expected. Because back height is measured vertically and tilting of the dummy cast forward in the 10°F, 10°T, 20°F, and SH conditions results in variation in the back height measurement (i.e., the back height should decrease as the dummy cast is tilted forward). The observed variability in our study is expected but may indicate a limitation of this metric’s utility in patients with abnormal posture.
The use of a dummy cast is a limitation of this study because the cast may not accurately reflect surface marker movement which would be present in a human subject. Surface marker motion is common to all rasterstereography techniques but good correlation between rasterstereographic and radiographic metrics has been reported [15, 24]. The present study presents a confirmation of the technology and our lab will evaluate the system in a human subject in the near future.
Intra-Observer and Inter-observer ICCs indicate that the MTS is highly reliable for all tested metrics excluding Pelvic Tilt. Lyon et al. assessed QSIS reliability using a random effects variance components model in 200 children with a diagnosis of adolescent idiopathic scoliosis and reported the highest reliability when three scans and three measurements were performed [25]. Although our data is not directly comparable to this previous research because only one “subject” was included in our study, we report excellent reliability of the MTS regardless of different investigators, trials, and positions.
CONCLUSION
We conclude that the MTS is a reliable method of newly developed raster stereography in a majority of clinically used parameters. Non-invasive methods of spinal monitoring are necessary to prevent exposure to health risks related to repeated x-rays in patients with scoliosis.
ACKNOWLEDGEMENT
Authors would like to thank Mr. Carlos Marquez, MS of mechanical engineer and Dr. Yu Wang, Ph.D of biomedical engineer for the help of testing.
CONFLICT OF INTEREST
Declared none.


