All published articles of this journal are available on ScienceDirect.
Navigated Cementless Total Knee Arthroplasty - Medium-Term Clinical and Radiological Results§
Abstract
Purpose:
The objective of this prospective study was to evaluate the medium-term clinical and radiological results after navigated cementless implantation, without patella resurfacing, of a total knee endoprosthesis with tibial and femoral press-fit components, with a focus on survival rate and clinical outcome. The innovation is the non-cemented fixation together with the use of a navigation system.
Scope and Methods:
Sixty patients with gonarthrosis were included consecutively in this study. In all cases, the cementless Columbus total knee endoprosthesis with a coating out of pure titanium was implanted, using a navigation system. The Knee Society Score showed a statistically significant increase from 75 (± 21.26) before surgery to 180 (± 16.15) after a mean follow-up of 5.6 (± 0.25) years. The last radiological examination revealed no osteolysis. No radiolucent lines were seen at any time in the area of the femoral prosthetic components. In the tibial area, radiolucent lines were seen in 24.4 % of the cases, mostly in the distal uncoated part of the stem. During follow-up, no prosthesis had to be replaced because of aseptic loosening while in 2 cases revision surgery was necessary due to septic loosening and in 1 case due to unexplainable pain.
Results and Conclusions:
Navigated cementless implantation of the Columbus total knee endoprosthesis yielded good clinical and radiological results in the medium term. The excellent radiological osteointegration of the prosthetic components, coated with a microporous pure titanium layer and implanted with a press-fit technique, should be emphasized.
INTRODUCTION
Implantation of a total knee arthroplasty has become a standard procedure in orthopaedic surgery. In various studies, the cemented fixation of the prosthetic components yielded good clinical and radiological long-term results and is thus regarded worldwide as the gold standard [1-4].
However aseptic loosening of the prosthesis accompanied by bone cement fragmentation is an important long-term complication in total knee arthroplasty [5-7]. This aspect should not be forgotten, particularly in view of the current trend to implant a total knee joint endoprosthesis more and more frequently in younger and more physically active patients. Particularly in this patient group, direct osseointegration of the prosthetic components is highly desirable [8].
In spite of this potential advantage, various drawbacks and complications following cementless fixation of prostheses of older designs were described in the literature [8]. Nevertheless excellent clinical and radiological long-term results were achieved using more modern cementless prostheses [9-11].
In addition to aseptic loosening of the implant, malalignment of the prosthetic components is another frequent reason for revision [7]. In several studies, a high failure rate was correlated with malalignment of the prosthetic components [12-14]. Computer-assisted navigation was shown to improve positioning of the prosthesis [15-19], but also has disadvantages such as preoperative registration prolonging surgery time, which, on the other hand, could be reduced with experience in a process optimization [20]. The surgical procedure is described in detail by Walde et al. (2005) [20].
The objective of this prospective study was to evaluate the medium-term clinical and radiological results after navigated cementless implantation, without patella resurfacing, of a total knee endoprosthesis with tibial and femoral press-fit components.
PATIENTS AND METHODS
Sixty patients with gonarthritis were included consecutively in this prospective study. Before the start of the study, severe knee deformity (varus/valgus >15°) or distinct ligament instability were defined as exclusion criteria. In addition, patients with advanced osteoporosis were treated with a cemented endoprosthesis and therefore excluded. Fifty-eight (97%) patients had primary and two (3%) secondary osteoarthritis due to a tibial plateau fracture. Mean age of the patients was 68 (min 44 and max 83) years with the majority of patients being female (55%). In all cases, a cementless total knee endoprosthesis without patella resurfacing was implanted using a navigation system (Columbus, Aesculap, Tuttlingen, Germany). Direct bone integration of the prosthetic components was to be achieved through a rough surface coating out of titanium with a pore size between 50 and 200µm (Plasmapore®, Aesculap, Tuttlingen, Germany, Fig. 1). In all cases, the OrthoPilot (software version 4.0) was used to position the tibial and femoral cuts (Aesculap, Tuttlingen, Germany). In a previous study, we evaluated the early postoperative clinical and radiological results and documented the optimized postoperative mechanical leg axis [20].

Dorso-lateral view of the Columbus total knee endoprothesis. The rough surface coating out of titanium (Plasmapore®) covers the backside of the prosthesis except for the distal part of the tibial stem.
For evaluation of the clinical results, the Knee Society Score (KSS) was recorded before surgery and at the last follow-up examination [21]. In the radiological analysis, the radiographs obtained immediately after surgery (anteroposterior and lateral view) were compared to the radiographs from the last follow-up examination (Fig. 2) and examined for osteolysis or radiolucent lines and evaluated in terms of location [22].

Lateral view with a follow-up of 4.9 years and a complete direct bone integration of the prosthetic components.
Statistical analysis was carried out using one-way ANOVA. The differences between the groups were analyzed with a Tukey-Kramer post-hoc test with a significance level of p ≤ 0.05. Survival probability of the prosthesis was estimated with the Kaplan-Meier method (GraphPad PRISM 4.0).
RESULTS
Patients
Fifty-two patients with a functioning knee joint endoprosthesis were evaluated after a mean follow-up of 5.6 (± 0.25) years. For reasons of distance or age, 3 patients were not willing to come to a follow-up examination. Contacted by telephone, these patients reported being subjectively satisfied with their knee endoprosthesis. These 3 cases were included in the calculation of the survival rate (52/60). One patient could not be reached. Altogether 8 patients did not attend the follow-up examination. At the time of the follow-up examination, 4 patients had died of causes unrelated to the implantation of the knee prosthesis. Until their death, no further operation had been carried out on the affected knee. In 2 patients, the prosthesis had to be replaced because of septic loosening after 8 and 12 months. Because of indeterminate chronic pain, but without radiological evidence of loosening or evidence of periprosthetic infection, one prosthesis was replaced after 15 months. The operation revealed bony ingrowth into the femoral and tibial components and an absolute stable situation without any bacteria.
Clinical Results
The KSS of 49 of the 60 patients was available for evaluation. The Functional Score improved from 50 (± 14.62) to 87 (± 7.28) points on average. The Knee Score increased from 25 (± 14.62) to 93 (± 7.28) points. Thus, altogether, there was an improvement from 75 (± 21.26) before surgery to 180 (± 16.15) points at the last follow-up examination. These differences were statistically significant (Table 1).
Clinical Results (n=49, *p ≤0.05)
| Preoperative Evaluation | Last Follow-Up Evaluation | p-Values | |
|---|---|---|---|
| KSS – functional | 50 (±14.62) | 87* (± 7.28) | p < 0.0001 |
| KSS – knee | 25 (±14.62) | 93* (± 7.28) | p < 0.0001 |
| KSS – total score | 75 (± 21.26) | 180* (± 16.15) | p < 0.0001 |
| Range of motion (ROM) | 101° (±14) | 116°* (±10) | p < 0.0001 |
In terms of range of motion, the mobility of the operated knee had improved to 116° (± 10) at the last follow-up examination, compared with 101° (± 14) before surgery. This difference was statistically significant (Table 1). None of the patients reported retropatellar pain at the last follow-up examination.
Radiological Results
At the last follow-up examination, 49 patients were subjected to a radiological evaluation. No radiolucent lines were observed on the tibia or femur on the postoperative radiographs. No osteolysis was found on the radiographs taken at the last follow-up examination. No radiolucent lines were seen around the cementless implanted femoral component at the last follow-up examination. In contrast, radiolucent lines were found in 12 (24.4%) patients at the prosthesis-bone interface of the tibial components (Fig. 3). In 10 of these patients, the radiolucent lines appeared around the non-coated distal part of the stem of the tibial components. In one patient, an isolated radiolucent line was seen on the proximal part of the tibial stem, and in one patient, on the ventral bearing surface of the tibial component. In all cases, the radiolucent lines were surrounded by a sclerotic margin.
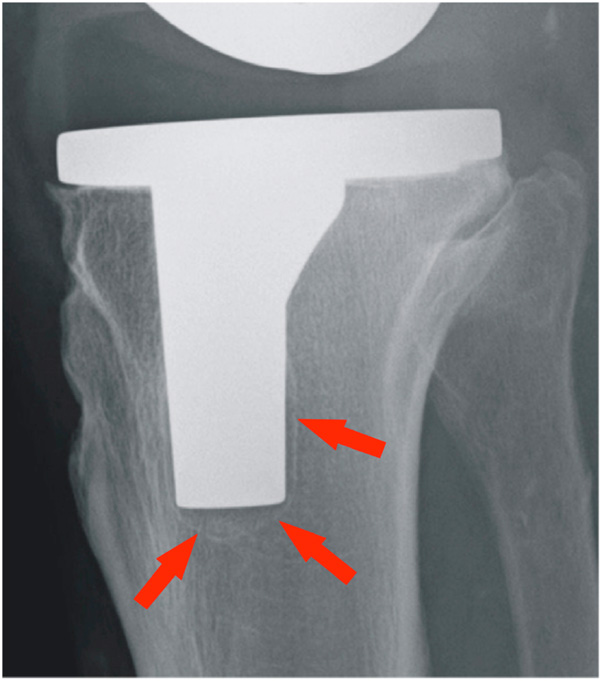
Lateral view of an asymptomatic patient with a follow-up of 5.1 years. Radiolucent lines are visible around the non-coated distal part of the tibial stem (arrows).
Cumulative Survival Rate
Over a survival period of 4.85 years, the cumulative survival rate of all replaced implants is 95%, and of implants replaced because of aseptic loosening 98.3%, the one patient with indeterminate chronic pain being included as “worst case scenario” as aseptic loosening may have played a role in the failure of the implant.
DISCUSSION
In this prospective study, we report the medium-term results after navigation-assisted cementless implantation of a total knee endoprosthesis without patella resurfacing at a mean follow-up of 5.6 years. The cumulative survival rate in form of a Kaplan-Meier curve was 94.4% for all replaced implants. No implant had to be replaced because of aseptic loosening. These survival rates are comparable to those reported in the literature [23, 24]. Our clinical results are in keeping with the meta-analysis of Hetamish et al. (2012), which compares navigated and conventional total knee arthroplasty [19].
Cementless retropatellar replacement is currently viewed critically in the literature. Several studies report complications requiring revision surgery particularly in connection with metal-backed components implanted without cement [25, 26]. In this study, no retropatellar resurfacing was carried out. None of the patients complained of parapatellar or retropatellar pain at the last follow-up examination.
Callaghan et al. (2004) identified malalignment of the prosthetic components as a major cause of failure of total knee joint endoprosthesis [7]. Computer-assisted navigation was repeatedly shown to improve the alignment of the prosthetic components and thus the resulting mechanical leg axis compared with a manual technique [15-19]. In a previously published study on the same group of patients, we achieved an optimized postoperative mechanical leg axis in all patients using computer-assisted navigation, thus excluding malalignment as cause for revision [20]. In the literature, the cementless implantation of the tibial component in particular is viewed as unfavourable [26-28]. In addition to failing osseointegration and development of osteolysis around the screws, radiolucent lines were frequently observed around the tibial components [26, 29, 30]. The radiological incidence of radiolucent lines depends on the quality of the images [31]. In this study, the radiographs were taken by an experienced radiologist. Particular attention was paid to the correct representation of the tibial plateau (antero-posterior view) and of the femoral component (lateral view). In contrast to other studies, no gaps were seen at the prosthesis-bone interface immediately after the operation [23]. In about ¼ of the cases, radiolucent lines with an osteosclerotic margin were present on the tibial component at the last follow-up examination. These results are in agreement with those reported in the literature [29, 30]. In this study, the radiolucent lines were seen at the distal part of the tibial stem in most cases. This part of the prosthesis is not covered by an additional surface coating (Plasmapore®). Presumably, this hindered a direct bone integration of the prosthesis in this area. In only 2 patients, a radiolucent line was seen in a direct connection to the rough titanium-coated surface of the tibial component. No radiolucent lines were observed in the area of the femoral component on the last radiographs. All of these patients achieved a good clinical result with a mean Knee Society Score of 184 points. The radiographs show that the microporous coating out of pure titanium used here allows for excellent bone integration of the prosthetic components.
The findings of the present study may be limited by the absence of a control group and the relatively small sample size, but it included the largest number to date of cementless and navigated total knee arthroplasties studied in the literature.
To summarize, navigated cementless implantation of this total knee joint endoprosthesis without patella resurfacing yielded good clinical and radiological results at medium-term follow-up. An excellent radiological osteointegration of the components implanted with a press-fit technique was achieved, confirming the benefit of the microporous coating out of pure titanium. We plan to continue to follow-up these patients to obtain long-term results.
CONFLICT OF INTEREST
The physicians involved in the study declare that they have no conflict of interest within the meaning of the Guidelines of the International Committee of Medical Editors. The study was partially sponsored by the company B. Braun-Aesculap.
ACKNOWLEDGEMENTS
J.P. Schüttrumpf: author, primary investigator, data interpretation. P. Balcarek, S. Frosch, M.M. Wachowski: data interpretation, radiographic grading. S. Sehmisch: statistical analysis. K.M. Stürmer: revising the manuscript critically for important intellectual content. H.-J. Walde: surgeries, data collection. T.A. Walde: chief medical supervisor. All authors have seen and approved the final version of the report.


