All published articles of this journal are available on ScienceDirect.
Comparing Functional Outcome of Triangle Tilt Surgery Performed Before Versus After Two Years of Age
Abstract
Background:
Many patients each year who are born with obstetric brachial plexus injuries eventually do not achieve complete recovery. As a result of the primary nerve injuries, these patients will often develop bony deformities involving the shoulder joint as a secondary consequence. The triangle tilt surgery has been shown to be an effective procedure to correct these deformities and has been performed on patients ranging in age from less than a year old to adolescence. The purpose of this retrospective study is to compare outcomes of triangle tilt surgery performed on patients before the age of 2 years versus after 2 years of age to determine an optimal age to operate on these children.
Methods:
36 patients with deformities developed secondarily from the initial obstetric brachial plexus injury in this study were divided into 2 groups. Group 1, those who had undergone triangle tilt surgery at < 2 yrs of age (16 patients). Group 2, those who were operated at > 2 yrs of age (20 patients). Group 1 age range: 9 months to 23 months, average: 18 months. Group 2 age range: 26 months to 9 years, average: 6 years.
Results:
Significant differences were found between the 2 groups (0-2 yrs vs > 2yrs) in regards to overall changes (pre- to post-op) in Mallet score, external rotation score, hand-to-mouth score, and supination angle.
Discussion:
This study demonstrates that triangle tilt surgery had better outcomes on clinical functioning if performed before the age of 2 years, however, improvement in clinical functioning can still be achieved if the triangle tilt surgery is performed after the age of 2 years as well. A possible mechanism to explain this phenomenon is the increased potential for anatomical remodeling if the triangle tilt surgery is performed at a younger age, thereby leading to significant functional improvement.
BACKGROUND
Obstetric brachial plexus injuries (OBPI) most commonly involve the C5 and C6 nerve roots although it can affect any or all of C5-T1 nerve roots. Several patients recover spontaneously within the first three months after birth. Secondary muscular imbalances and bony deformities at the shoulder joint due to inadequate recovery of neurological function are the major cause of long-term morbidity in this patient population [1-4].
Characteristic anatomic changes of the shoulder joint include glenohumeral dysplasia, dislocation and posterior subluxation of the humeral head, and medial rotation contracture. Although considerable efforts have been made to characterize and correct these deformities in OBPI patients, relatively less emphasis has been placed on the optimal age for surgical correction. The triangle tilt (TT) surgical procedure developed and performed by the lead author was shown to have successful outcomes in 9 months to adolescence OBPI patients [5-11]. The TT surgical technique includes osteotomies of the clavicle and the neck of the acromion, allowing the distal acromioclavicular triangle to tilt back to a more neutral position and allowing the humeral head to improve congruency. The purpose of this retrospective study is to compare functional outcomes for OBPI patients undergoing TT surgery before the age of 2 years versus after two years of age to determine an optimal time to operate on these children.
METHODS
36 patients with deformities developed secondarily from the initial OBPI were included in this study. Patients were divided into 2 groups: those who had triangle tilt at < 2 yrs of age (Group 1, 16 patients) and those who were operated at > 2 yrs of age (Group 2, 20 patients). Group 1 age ranged between 9 months and 23 months with an average age of 18 months. Group 2 age ranged between 26 months and 9 years with an average age of 6 years. All clinical evaluations were performed by trained research scientists, independent of the surgeon and senior author. These scientists were trained in assessing clinical function through viewing pre- and post-operative video recordings of clinical examinations and scoring functional levels using a modified Mallet scale [11] (Fig. 1). A retrospective study was conducted in which data was collected in order to compare the effect of the procedure on clinical functioning of the patients. The average follow-up time from TT surgery to post-operative Mallet scoring was 2.5 years. The Mann Whitney test was conducted to determine the significant difference between these 2 groups of patients for the change-in (pre- to post-op) parameter values. In addition, we analyzed the pre-operative values to determine if there were any significant differences in terms of pre-operative values between these these 2 groups of patients using Mann Whitney test (Table 2). Results were considered statistically significant at p < 0.05 level. All statistical analyses were performed using the Analyse-It plugin for Microsoft Excel 2003 software (Leeds, UK).
Comparison of pre-operative Differences in Modified Mallet Score between 2 Age Groups of OBPI Patients
| Parameter | Group 1 (< 2 yrs) Pre-op Mean | Group 2 (> 2 yrs) Pre-op Mean | Difference in Means | P Value Mann Whitney Test |
|---|---|---|---|---|
| External Rotation Score (0-5) | 2.3 | 2.5 | 0.2 | 0.19 |
| Hand-to-Mouth Score (0-5) | 1.9 | 2.1 | 0.1 | 0.80 |
| Supination Angle (°) | -18.4 | 8.5 | -26.9 | 0.02 |
| Total Mallet Score | 12.1 | 13.8 | 1.7 | 0.003 |
Angle of apparent active supination was recorded as follows: 0° = neutral position, 90° = full apparent supination, -90° = full apparent pronation.
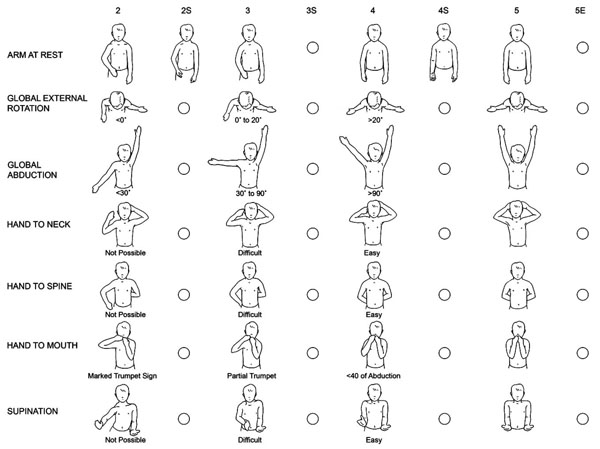
The Nath Modification of Mallet’s System [11]: Clinical Scoring of Function. In addition to assessing the classical functions of the Modified Mallet system, supination and the resting position are evaluated. To further define deformity, fixed forearm supination (positions 2S, 3S, and 4S) as well as external rotation position (5E) are scored.
RESULTS
The pre- and post-operative means, difference in means, and p values for each measurement parameter are shown in Table 1. Significant differences were found between Group 1 (0-2 yrs) and Group 2 ( > 2yrs) for change-in (pre- to post-op) values of the following functional parameters: external rotation score, hand-to-mouth score, supination angle, and total Mallet score. Group 1 (0-2 yrs) showed improved outcomes in each of these categories when compared to Group 2 (> 2 yrs).
Comparison of Total Change (Pre- to Post-TT) in Modified Mallet Score Between 2 Age Groups of OBPI Patients
| Parameter | Group 1 (< 2 Yrs) Mean | Group 2 (> 2 yrs) Mean | Difference in Means | P Value* Mann Whitney Test |
|---|---|---|---|---|
| External Rotation Score (0-5) | 1.5 | 0.69 | 0.81 | 0.0029 |
| Hand-to-Mouth Score (0-5) | 2.0 | 1.0 | 1.0 | 0.0035 |
| Supination Angle (°) | 78 | 20 | 58 | 0.0061 |
| Total Mallet Score | 6.6 | 3.8 | 2.8 | 0.0002 |
Angle of apparent active supination was recorded as follows: 0° = neutral position, 90° = full apparent supination, -90° = full apparent pronation.
Statistically significant difference in means (p < 0.05).
The pre- to post-operative change in the external rotation score (scored on a scale of 0-5) was significantly higher (2 fold) for Group 1 compared to Group 2 values (mean: 1.5 vs 0.69; difference in means: 0.81, p < 0.0072). Hand-to-Mouth Score, also scored on a scale of 0-5 had a significantly higher pre- to post-operative change value for Group 1 compared to Group 2 (mean: 2.0 vs 1.0; difference in means: 1.0, p < 0.0208).
Supination Angle was measured as follows: 0° = neutral position, 90° = full apparent supination, -90° = full apparent pronation. Change in supination angle was also significantly higher (4 fold) for Group 1 compared to Group 2 (mean: 78° vs 20°; difference in means: 58°, p < 0.0093). Total Mallet Score also had a significantly higher change for Group 1 than Group 2 (mean: 6.6 vs 3.8; difference in means: 2.8, p < 0.0047). Pre-operative Mallet scores were not statistically different in these 2 groups in regards to external rotation and hand-to-mouth functions, but the supination angle and the total Mallete scores were statistically lower in children, who were operated at < 2 years of age (Group 1). Although, the children in group1 had pre-operative Mallet scores lower than the children in group 2 (> 2 years), the children who were operated below 2 years of age (Group 1) had better functional outcomes.
DISCUSSION
We scored clinical functioning parameters pre- and post-operatively on 2 groups of patients: those who had the TT surgery before the age of 2 years (Group 1) versus those who had the surgery over 2 years old (Group 2). We chose 2 years as cut off age because the infancy ends at this age. The pre- to post-operative change values were compared between the two groups. Significant differences for external rotation score, hand-to-mouth score, supination angle, and total Mallet score were found between the 2 groups, with Group 1 having better functional outcomes compared to Group 2.
These results indicate that there are significant differences in functional improvement of OBPI patients if the TT surgery is performed before the age of 2 years versus after 2 years of age. A possible mechanism to explain this phenomenon is the increased potential for anatomical remodeling if the triangle tilt surgery is performed at a younger age, thereby leading to significant functional improvement. Because ossification is still occurring in younger age groups [12], the scapula, glenohumeral joint, and the associated bony anatomy and structures are still modifiable in terms of remodeling. The greater the change in remodeling that occurs, the greater are the outcomes in terms of clinical functioning. Our study demonstrates that the optimal time to perform the TT surgery is before the age of 2 years. However, our results also indicate that improvement in clinical functioning can still be achieved if the TT surgery is performed after the age of 2 years as well. This is further supported by the results of another study conducted by Nath et al. 2010 [9].
We recommend that the TT surgery be performed before the age of 2 years for optimal improvements in outcomes of clinical functioning. The triangle tilt can be performed as early as nine months and can be performed up until late adolescence (16-17 years). This upper age is limited by the declining ability of the glenohumeral joint to remodel [6]. The triangle tilt surgery allows for repositioning and remodeling of the glenohumeral joint [8] and improves functional outcomes in OBPI patients. Optimal clinical outcomes are achieved if TT surgery is performed before the age of 2 years but improvements in functioning are observed if the surgery is performed after this age as well.
AUTHORS' CONTRIBUTIONS
RKN conceived and participated in the design of the study and revision of the manuscript. FM participated in the design of the study, collection of data, and drafting the manuscript. CS participated in collection of data, data analysis and revision of the manuscript. All authors have read and approved the final manuscript.


