All published articles of this journal are available on ScienceDirect.
Comparative Study of Clinical and Radiological Outcomes of Unconstrained Bicondylar Total Knee Endoprostheses with Anti-allergic Coating
Abstract
Background:
Hypersensitivity reactions to implant materials have become more important in total knee replacement (TKR). The purpose of this retrospective comparative study was to evaluate the clinical and radiological outcomes of unconstrained bicondylar total knee prostheses with and without anti-allergic titanium(niobium)nitrite (Ti(Nb)N) coating.
Methods:
Twenty-four patients (25 TKRs) underwent a preoperative clinical evaluation and then a postoperative evaluation after 26.2 months in the allergy group treated with coated implants (n=13 implants) and after 24.5 months in the control group treated with uncoated implants but identical geometry (n=12) using HSS, WOMAC and SF-36 scores. Radiological evaluations were performed using standard anterior-posterior (a.p.) and lateral X-rays.
Results:
During follow-up two patients of the allergy group had to undergo revision surgery due to non-implant-related reasons. A comparative analysis of both study groups showed a significant difference in the HSS scores at both evaluation time points (MW test p≤0.050); these findings are remarkable since the control group had a significantly lower score preoperatively (54.0 vs 65.0 points) and a significantly higher score (82.5 vs 75.0 points) postoperatively. The preoperative and postoperative WOMAC and SF-36 scores were comparable in both groups (MW test p≥0.052), although the postoperative increase in the score for the allergy group was lower. The radiological results were comparable in both groups and were unlikely to influence the results.
Conclusions:
This clinical study demonstrates the restricted outcome in postoperative function and quality of life in the allergy group compared to the control group.
INTRODUCTION
Total knee replacement (TKR) is one of the most successful surgical techniques in orthopaedic surgery [1-3]. However, possible reasons for limited survival rates of total knee endoprostheses include mal-positioning, maldimension and particle-induced aseptic loosening, and also hypersensitivity reactions to the implant materials [2-5]. Therefore, an increasing sensitization of the overall population to contact allergens such as nickel, chromium or cobalt results in an increasing demand for alternative implant materials [3, 4, 6-8].
Clinical Significance
According to Thomas [5], chromium-cobalt-nickel alloys have the greatest potential for triggering allergic reactions, where the incidence of allergic reactions on the skin was found to be up to 20% [5]. The average contact allergy rate in the general population is 13.1% for nickel (women 20.4%, men 5.8%), 3% for cobalt and 1% for chromium [7]. A large-scale study [8] showed that allergic reactions to nickel and cobalt vary considerably depending on age and sex. It was found that nickel hypersensitivity occurred at rates of 32.5% in females <40 years of age and 13.2% in females aged >40 years. In male patients, however, the percentages of individuals who exhibited contact allergy to nickel were only 6.2% (<40 years) and 4.6% (>40 years) [8]. Furthermore, allergies to bone cement components were also described [9].
The insertion of foreign material into the body, for example in artificial joint replacement, induces an immune response that depends on the properties of the material and the sensitivity of the patient [6]. In case of specific sensitization to the components of the implant, hypersensitivity reactions can occur, with either localized or generalized exanthems, urticaria and swellings, or even with aseptic implant loosening [5, 6, 8]. The latter is a hypersensitivity reaction of the delayed type, according to Coombs and Gell (type IV reaction) [6]. Although this reaction has not yet been sufficiently clarified, histological findings support the assumption that it represents an excessive lymphoplasmacellular fibrinous infiltration as part of type I or IV neosynovialitis, in accordance with the consensus classification, depending on the amount of wear particles, as is the case in particle-induced aseptic loosening, but without wear particles (Fig. 1) [10].
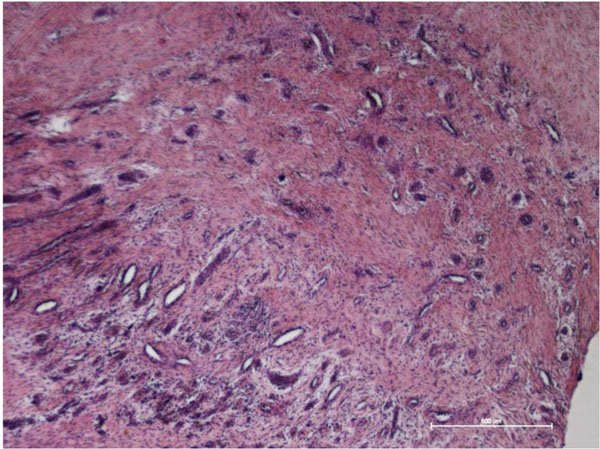
Histological analysis (haematoxylin and eosin staining) of adhesion tissue in a proximal recess obtained from the knee joint three months after implantation of a total knee endoprosthesis made of a cobalt-chromium alloy with a proven sensitization to nickel(II)- sulphate. Excessive lymphoplasmacellular fibrinous infiltration was found as part of type IV neosynovialitis, according to the consensus classification [10] (courtesy of the Department of Pathology, University of Rostock).
Alternative Material Solutions
If patients who require implantation or revision surgery of artificial knee joints show sensitivity to metal implant materials, the following possible solutions must be considered during preoperative planning: implant components without metal elements (e.g. made of ceramics and solid polyethylene), the use of non-sensitive metal implant materials (e.g. titanium alloys and/or zirconium-niobium (ZrNb) alloys) or the use of metal materials after the implant surface has been coated with a suitable anti-allergic layer (e.g. with Ti(Nb)N) [4].
Ceramic implants are now being used all over the world in total hip replacement for various reasons, including their high chemical and mechanical stability and their excellent corrosion resistance due to the lack of electrochemical reactivity and very good tribological properties [11]. A negative characteristic that needs to be mentioned is the high brittleness and low damage tolerance of the oxide ceramics used clinically [12, 13]. New composite ceramics for total knee replacement such as BIOLOX® Delta, with improved material properties, or Oxinium® (ZrNb alloy with a ceramic ZrO2 surface) are currently undergoing clinical follow-up studies [4, 14].
Titanium alloys exhibit very good biocompatibility [4]. However, due to their susceptibility to wear resistance, titanium materials that have not undergone prior treatment cannot be used in areas of the artificial knee joint that are subjected to high tribological stress, for example in articulating surfaces [15]. However, different methods of surface modification and thus for increasing wear resistance are available [16, 17].
In addition to Oxinium, ceramic Ti(Nb)N coatings with a layer depth in the µm range have been used as a surface coating for implants made of titanium or cobalt-chromium alloys [16-18]. Knee simulator wear analyses showed that TiN-coated femur and polyethylene components exhibited lower wear rates than uncoated samples [4].
In spite of the continuously increasing use of allergy-coated implants in total knee replacement, sufficient data on the clinical and radiological outcomes of these implants are still unavailable [3]. The femoral head coatings used in the 1990s exhibited a partial layer failure in clinical settings, particularly under the influence of third bodies [18].
Thus, the aim of the present clinical comparative study was to evaluate the mid-term functional and radiological outcomes of a total knee replacement system made of a cobalt-chromium alloy with and without an anti-allergic coating consisting of Ti(Nb)N.
MATERIALS AND METHODS
Patients who had undergone primary total knee replacement due to primary and secondary osteoarthritis of the knee were included in the study. The local ethical committee approved the study (Reg. Nr. A 2008-63). The Genia® total knee replacement system (ESKA Implants, Luebeck, Germany), with a rotating insert made of standard polyethylene, was used. This posterior stabilized implant system with an ultracongruent insert can be used in cases of partial or total loss of the posterior cruciate ligament. Both the femoral and the tibial components consisted of a cobalt-chromium alloy and in the standard version they were fixed using PMMA cement (Refobacin Bone Cement, Biomet Deutschland, Berlin, Germany). In patients with known allergies to the above mentioned metallic materials or bone cement components, titanium(niobium)nitrite (Ti(Nb)N)-coated implants of an identical geometry were used, which in five cases were fixed to the bone as a cement-free version.
Patients sensitive to the metallic and/or bone cement materials, as documented by preoperative allergy testing or anamnestic data, were allocated to an allergy group; those who were not sensitive were allocated to the control group. No epicutaneous allergy testing was conducted before or after total knee replacement in the control group, where there was no history of allergies. No significant differences were found with respect to indications, gender, age, weight or comorbidities between both groups (Table 1).
Demographic data of the study groups in mean ± SD and ranges. Significant differences were not found
| Allergy Group | Control Group | p-Value | |
|---|---|---|---|
| Patients (n) | 12 | 12 | |
| TKR (n) | 13 | 12 | |
| Gender (female/male) | 9/3 | 11/2 | |
| Age (years) | 70.6 SD 7.7 | 67.2 SD 6.5 | p=0.547 |
| Body height (cm) | 160.0 SD 11.2 | 169.2 SD 29.6 | p=0.649 |
| Body weight (kg) | 86.2 SD 19.0 | 85.3 SD 11.0 | p=0.517 |
| BMI | 33.5 SD 6.0 | 29.6 SD 2.4 | p=0.838 |
| Follow-up | 26.2 SD 4.6 | 24.5 SD 1.0 |
All of patients received the total knee replacement in a standardized manner by experienced orthopaedic surgeons: Payr's approach was used. The TKRs in both groups were performed by two surgeons, but four knee replacements in the allergy group were performed by two other surgeons. Before the exsanguination cuff (300 mmHg) was applied, all patients were given 1.5 g cefuroxime i.v. as perioperative antibiotic prophylaxis. Intraoperatively, smoothening of the lateral patella facet, denervation and soft-tissue balancing were carried out until perfect positioning of the implant components was achieved with respect to the biomechanical aspects. Postoperatively, all patients were given analgesia of the required grade. Thrombo-embolism prophylaxis was conducted daily by a subcutaneous application of low-molecular-weight heparin and by applying compression stockings throughout the hospital stay and follow-up medical treatment. In all cases, mobilization was started on the second day after surgery, using two forearm crutches and a four-point gait with full weight-bearing.
Clinical and Radiological Evaluation of the Patients
At our hospital, preoperative evaluation of all patients to obtain functional and subjective scores has become a matter of routine before total knee or hip replacement. As a result, a prospectively collected preoperative data record was available. The preoperative data of three patients in the allergy group were incomplete and could not be used. The evaluation included all patients who had undergone primary total knee replacement with an anti-allergy-coated implant at our hospital between 2006 and 2007. The control group was matched from an independent study that contained 20 primary knee replacements within the same period. Although all anti-allergy-coated TKRs from the two-year period were included, the number of cases was still small and therefore evidence of the results in the allergy group is limited. One examiner (P.B.) carried out the clinical and radiological follow-up examinations. In addition to a detailed anamnesis, during which any possible postoperative complications, the distance the patient was able to walk, the use of medical aids and analgesia consumption were recorded, a standardized clinical follow-up examination was conducted. The latter was based on the “Hospital for Special Surgery (HSS) Score” according to Ranawat and Shine [19]. This score, which was especially developed for the clinical follow-up of total knee endoprostheses, considers both subjective functional criteria (62%) and objective examination findings (38%), with a maximum attainable value of 100 points.
The patient assessment also included an evaluation of the symptoms and limitations of physical functions in everyday life: the Western Ontario and McMaster Universities score (WOMAC), which is the most frequently used questionnaire for recording arthrosis-specific symptoms from the patient’s point of view [20]. In addition, the health-related quality of life and the general state of health were evaluated by the Short Form-36 (SF-36) score [21].
These data were gathered and then used to analyze all functional, physical and psychological aspects of the postoperative clinical follow-up examinations.
Standardized anterior-posterior (a.p.) and lateral X-rays were taken preoperatively, at day 5 postoperatively and at the above mentioned evaluation times. Radiolucent lines and osteolysis of the femoral and tibial bone stock were noted. The cause of the radiolucent lines was attributed to either signs of loosening and fissures appearing as discrete axis deviations or to an insufficient cement layer. Furthermore, in addition to the positioning of the femoral and tibial implant, the total axis of the operated extremity was evaluated.
Statistical Analysis
All data were scored and analyzed by using the statistical software package SPSS 15.0 (SPSS Inc. Chicago, Illinois, USA) for Windows™. Descriptive statistics data were computed for continuous and categorical variables. The statistics computed for the demographic data included the mean and standard deviations (SD) of continuous variables and are presented as mean ±SD. The statistics for the score outcome are presented as medians with interquartile ranges (IQ).
The sample size calculation was based on the primary HSS score parameter and on information from the above mentioned previous trial. The preoperative mean was about 55 ±10 and the postoperative mean about 70 ±11. The standard deviation of the difference between these values was about 17. Therefore, the sample size was computed in expectation of an average difference between the two time points of 15 with an SD of ≈17. Using the paired t-test, this implied that n=13 patients were necessary in order to detect a difference of about 15 between two situations with a power of 1-ß=0.80 and a two-sided significance level of 0.05. These calculations were performed using module MOT1-1 of nQuery Advisor 7.0 (Statistical Solutions, Saugus, USA).
Comparisons within the groups at the two clinical evaluation points were carried out using a Wilcoxon signed-ranks test (WI) for the difference between two paired samples. In order to determine significant differences in the scores between the two patient groups, the Mann-Whitney (MW) U test by ranks was used as a non-parametric test for comparing independent samples. All p values are the result of two-sided statistical tests and p≤0.05 was considered statistically significant.
RESULTS
Twenty-seven patients were included in the study. Of these, a total of 15 patients with allergies to implant materials had undergone total knee replacement. However, three patients refused a follow-up examination without giving reasons and were therefore excluded. As a result, the allergy group consisted of 12 patients, with one patient who had had a TKR implanted on both sides (n=13 implants). There was a proven nickel allergy in five cases and a proven allergy to cement components in five cases. One patient exhibited a combined sensitization to nickel and cement components. In the remainder of the 12 patients who had undergone a follow-up examination, a coated implant had been used since their anamnesis had indicated sensitization to metal (jewelry). The control group consisted of 12 patients and 12 implants.
During the two-year follow-up period, one patient in the allergy group had to undergo revision surgery several times due to painful restriction of movement without implant malalignment. During long-term progression, instability occurred, and the polyethylene insert was changed. Another patient of the allergy group underwent osteosynthesis of a distal femur fracture after trauma (one year after TKR). No other complications were recorded, in particular implant-related complications.
The HSS score improved preoperatively to postoperatively in both groups (Table 2). However the increase in subjective functionality and in the objective examination findings was only significant in the control group (WI test p=0.003). In particular, the parameters “pain” and “muscle strength” of the HSS score exhibited significant improvements compared to the preoperative initial findings in both groups (WI test: pain p≤0.017, muscle strength p≤0.025). The function parameter showed a significant improvement in the control group (WI test p=0.003), whereas the improvement in function in the allergy group was non-significant (WI test p=0.057). A comparative analysis of both study groups found a significant difference in the overall HSS scores at both evaluation time points (MW test p≤0.050); these findings are remarkable, since the control group had a significantly lower score preoperatively and a significantly higher score postoperatively.
HSS, WOMAC and SF-36 scores at each evaluation point
| HSS Score | WOMAC Score | SF-36 Score | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Group | Allergy | Control | MW-test | Allergy | Control | MW-test | Allergy | Control | MW-test |
|
|
|||||||||
| Preoperative | 65.0 | 54.0 | p=0.050 | 49.0 | 44.3 | p=0.418 | 44.0 | 53.0 | p=0.382 |
| IQ | IQ | IQ | IQ | IQ | IQ | ||||
| 9.0 | 19.0 | 16.1 | 9.9 | 46.0 | 20.0 | ||||
|
|
|||||||||
| Follow up | 75.0 | 82.5 | p=0.030 | 60.5 | 73.5 | p=0.168 | 46 | 64.5 | p=0.052 |
| IQ | IQ | IQ | IQ | IQ | IQ | ||||
| 16.0 | 11.0 | 38.0 | 31.0 | 34.0 | 28.0 | ||||
|
|
|||||||||
| WI-test | p=0.059 | p=0.003 | p=0.028 | p=0.003 | p=0.859 | p=0.084 | |||
The Wilcoxon test (WI) indicated significant differences between the evaluation time points within the groups. The Mann-Whitney test (MW) indicated significant differences between the groups. The level of significance is p≤0.05. All values are presented in medians with interquartile ranges (IQ).
Postoperative versus preoperative improvements in the WOMAC score were significant in both groups (WI test p≤0.028). A comparison of the preoperative and postoperative scores of the groups found no significant differences between the allergy group and the control group (MW test p≥0.168) in the overall score (Table 2).
For the postoperative evaluation, the SF-36 score indicated a non-significant improvement in the control group compared to the initial preoperative findings (Table 2). No increase in the quality of life was found in the allergy group between the preoperative and postoperative evaluations. When comparing both groups, no significant differences were found in the overall score (MW test p≥0.052) at any time.
In the allergy group, the range of motion amounted to 125.0° IQ 38° (flexion 85-135°) and in the control group the value was 117.5° IQ 25° (flexion 95-135°). Extension deficits >5° were not identified in either of the two groups. One patient in the allergy group exhibited extension hypermobility of 5°.
Radiological Outcomes
Implant positioning in most cases was optimum or exhibited only slight deviations. Radiolucent lines around the femoral component, which were not detected in the X-ray pictures made immediately after surgery, were observed in one case in zones 1 and 2 (anterior) and 3 and 4 (posterior) in the allergy group. Radiolucent lines were present in the control group in four cases. In one case, these lines were positioned in zones 1 and 4. In three patients, radiolucent lines were only detected in one zone (in two patients’ zone 1 and in one patient zone 4). A femoral implant in a patient in the allergy group exhibited a surgical gap of up to 2 mm in zone 1 (anterior). This was caused by missing cement augmentation due to the use of a cementless implant (Fig. 2).

X-rays (anterior-posterior and lateral) of the knee joint of a 73-year-old female patient 25 months after implantation of a cement-free Genia® total knee replacement (left) with an anti-allergic (Ti(Nb)N) coating, as well as X-rays of a 55-year-old male patient 24 months after implantation of a cemented Genia® total knee replacement made of a cobalt-chromium alloy (right). No radiolucent lines were detected around the components in either of these cases. In the lateral view of the total knee replacement with the anti-allergic coating, a gap is visible in femoral zone 1, which is caused by discrete over-dimensioning with flexed positioning of the component.
The tibial implants were firmly fixed in all cases. Radiolucent lines were detected in two patients in the allergy group (zones 8, 9 and 10 respectively zone 6) and in one patient in the control group (zones 1 and 10). Stable fixation can be assumed in all cases because no clinical symptoms of implant loosening were present at the follow-up examination. The radiolucent lines around the femoral and tibial components had a maximum size of 1 mm. No cases of osteolysis occurred within the 24-month follow-up period.
DISCUSSION
As the number of implantations is increasing, total knee replacement systems must meet higher demands with respect to load-bearing capacity and function [3]. Changes in implant design and material with the aim of minimizing abrasive wear and solving the allergy problem associated with metallic materials have led to the development of coated implants [4, 6]. However, comprehensive prospective or retrospective studies have not been published so far due to the small number of implantation procedures using allergy-coated primary total knee replacement.
In the present study, we observed lower rates of improvement in mid-term functional scores and quality of life in the allergy group treated with the Ti(Nb)N-coated total knee endoprosthesis Genia® in comparison to a matched control group with the use of uncoated implants of an identical geometry. In an independent prospective study with an uncoated implant type of the same design, 75.6 points (HSS scores) were achieved six months after surgery [1]. Other studies using different TKR systems identified HSS score values between 85.0 and 93.0 points one year postoperatively, with a similar average preoperative score of 55.9 to 62.0 points [22, 23]. The control group achieved similar high scoring values during the follow-up examinations.
The comparison of both groups found significant differences in the HSS scores. The control group had a significantly lower score preoperatively, whereas the postoperative evaluation showed opposed significant results. Furthermore, no significant improvements were found in patients with coated implants compared to the initial preoperative findings. These results could have been affected by the fact that non-implant-related revision surgery was carried out in two cases in the allergy group. Moreover, one female patient in the allergy group suffered from persistent grade 1 medial instability with an extension deficit of 5° after conservative therapy of a traumatic rupture of the medial collateral ligament. Due to these non-implant-related restrictions, the evidence of the results in the allergy group may be limited.
No preoperative differences were found in the WOMAC and the SF-36 scores between the two groups and the postoperative differences were also non-significant. Correspondingly, the anamnestic data gathered at the follow-up evaluation showed a discrete distortion of the results caused by new developed comorbidities, which negatively affected the outcome of the allergy group, i.e. two cases of degenerative lumbar spine pathology and one case of severe osteoarthritis of the hip [21].
Comprehensive prospective studies with anti-allergic TKRs have not been conducted so far. Furthermore, there is no information on whether or not patients with allergies have a reduced functional outcome in general. Only small numbers of implantation procedures using allergy-coated primary total knee replacement are available. Therefore, investigations are and will be limited in terms of evidence.
Since the age distribution in both groups only slightly differed, it can be assumed that no systematic distortion occurred in this context. As yet, a significant influence of patient age on early functional outcome after total knee replacement is not known; however, significant influences were reported in follow-up examinations covering a period of one year or more [24]. Implant positioning showed no major deviations in the allergy and control groups. Hence, the postoperative outcome should not be influenced by implant mal-alignment. Four knee replacements in the allergy group were implanted by two other surgeons; therefore, a surgeon bias may be relevant in these cases.
The radiolucent lines around the components observed in our study in both groups could be risk factors of implant loosening, even though no clinical symptoms were evident. The presence of asymptomatic radiolucent lines of up to 1 mm in size around the tibial component was found in 3 to 9.5% of all cases and around the femoral component in 2.7% of all cases [25, 26]. These lines occur in the early postoperative phase (up to three months) and can be interpreted as a stress-shielding phenomenon. Since no early postoperative radiological data were available for our study patients, the detection of stress-shielding was not possible.
Bin et al. [22] evaluated the range of motion of a standard-type and high-flex design total knee replacement system. After a year of follow-up examinations, the two study groups exhibited HSS scores of 92.0 and 93.0 points, with significant differences in the range of motion (129.8° ±5.2° vs 124.3° ±9.2°). In another study that included 684 total knee replacements, the average range of motion found was 110° ±15° [27]. Therefore, the range of flexion motion in the present study is within the values reported by both groups. However, the range of motion in TKR should not be used as the only criterion for evaluating postoperative outcome. A low percentage weighting of the range of motion in knee scores indicates the relatively minor significance of this parameter [19]. Nevertheless, a minimum degree of flexion is a prerequisite for a good postoperative outcome with respect to functional, physical and psychological aspects. Patients with a limited range of motion, i.e. a degree of flexion below 95°, exhibit a significantly worse WOMAC score [27].
Ceramic implants and implants made of titanium alloys, which only rarely trigger allergic reactions, are an alternative to the anti-allergic cobalt-chromium coating in knee endoprostheses [4, 14, 17]. However, titanium materials that do not have a surface coating are not used for total knee replacement due to their comparatively low wear resistance [15]. Studies of ceramic knee components exhibited HSS scores of 86 points, with a range of motion of between 113° and 124° and a follow-up period of between one and ten years [14, 25, 28, 29]. However, ceramic implants are characterized by a higher risk of brittle fracture and the demand for cement-free implant fixation has not been realized so far, particularly in connection with polyvalent sensitization to cement components. Therefore, the use of ceramic knee implants is still limited [4, 14].
CONCLUSION
In summary, this clinical, comparative study noted differences in the postoperative outcome between the allergy group with Ti(Nb)N-coated total knee replacements and the control group (uncoated implants with an identical implant geometry). In clinical routine, the focus is increasingly placed on hypersensitivity reactions to implant materials, which are the subject of current research. In this context, the aim is to find valid methods for diagnosing implant allergy as well as optimal solutions in the case of sensitization to specific implant materials.
CONFLICT OF INTEREST
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party directly or indirectly related to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution or other non-profit organizations to which one or more of the authors are associated.
ACKNOWLEDGEMENT
None declared.


