All published articles of this journal are available on ScienceDirect.
Patella Infera in an HIV Positive Patient Following Total Knee Arthroplasty
Abstract
A lowering of the patella after total knee arthroplasty is accompanied by pain and a restriction of the range of motion. With its etiology being unclear at present, a multifactorial genesis is under discussion. For the first time, we present a case report describing an HIV infection as a possible cause of patella infera.
A 54-year-old HIV-positive woman developed patella infera (Insall-Salvati ratio 0.6) with a painful restriction of motion 18 months after implantation of a bicondylar surface prosthesis. By changing to a partially coupled endoprosthesis, distalization of the joint line and partial patellar resection, the patient was free of symptoms with a ROM of 0°/0°/110°.
All risk factors known from the literature could be excluded in this case, so that the presence of an HIV infection has to be discussed as a possible cause.
INTRODUCTION
The reasons for the development of patella infera after total knee arthroplasty are still unclear, despite a prevalence of 25% [1, 2]. Verified risk factors include previous operations on the knee [3, 4], delayed postoperative mobilization [5] and lateral release [2].
The presence of an HIV infection is accompanied by impaired wound healing and scar formation [6], and coincides with Dupuytren's contractures [7, 8]. However, there have been no reports of an influence of HIV infection on ligamentous structures of the knee to date. For the first time, we describe a lowering of the patella in an HIV-positive woman
CASE REPORT
The right knee of a 54-year-old woman was treated with a cementless bicondylar surface prosthesis without patellar replacement, due to primary varus gonarthrosis in January 1999 (Foundation Knee, Endoplus, Germany). The patient did not have an orthopedic or internal medical history. The endoprosthesis was correctly positioned, in particular the preoperative joint line was maintained with an Insall-Salvati ratio of 1.1. Computed tomography was used to ensure the correct rotation of the femoral and tibial components. Lateral release was not necessary on primary implantation. The patient was discharged after a complication-free course, with a ROM of 0°/0°/90°.
18 months later, the patient presented with a painful restriction of motion to 0°/ 15°/70°. Clinical symptoms were anterior knee pain, a mild overheating of the joint, and crepitation over the entire range of motion. Plain radiographs revealed a marked patella infera (Insal-Salvati ratio 0.6). Radiological controls conducted over the further course showed a successive lowering of the patella (Fig. 1). The bone mineral density of the patella appeared to be normal in the plain radiographs, so that reflex dystrophy and at least markedly deficient blood supply to the patella and surrounding tissue could be ruled out. In the laboratory tests, an HIV infection was detected for the first time. The patient was completely asymptomatic.
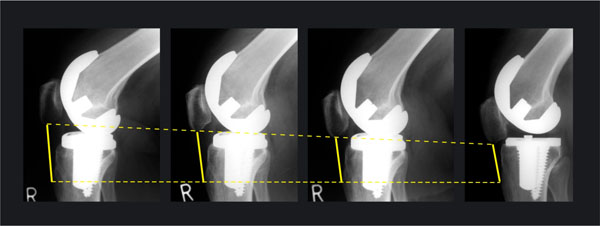
Development of patella infera. 18 months postoperatively, the patella contacts the PE inlay at 60° flexion.
Revision surgery was performed, with the prosthesis being changed to a partially coupled system (Solution, Endoplus, Germany). Intraoperatively, scar changes of the thickened and shortened patellar ligament were seen, with a normal Hoffa's body. A biopsy of the patellar ligament revealed degenerative changes, with a reduction in cell density and compression of collagen fibers (Fig. 2). The tibial and femoral components were correctly rotated and the patella was centered.
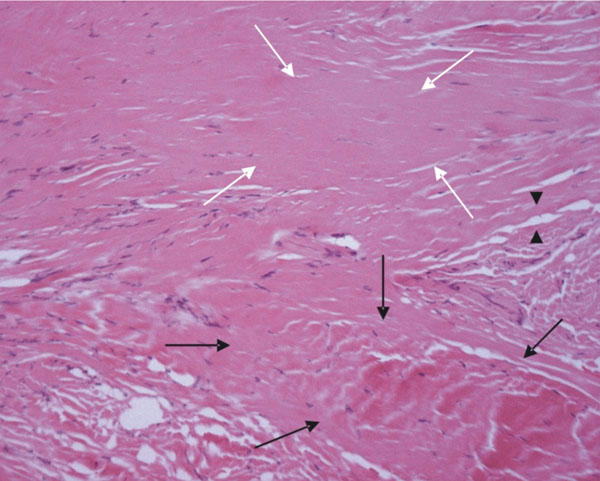
Section through a biopsy from the patellar ligament, with only partially retained ligament structures in the form of taut collagenic connective tissue (black arrows). The majority of the sample shows degenerative changes, such as maceration of the fibers, the absence of fibrocytes (white arrows) and small foci of lipomatous transformation (arrow tips). Connective tissue proliferation cannot be seen (hematoxylin-eosin, magnification 200x).
The joint line was distalized 8mm and the patella was partially resected 8 mm distally (Fig. 3). The range of motion under anesthesia was improved from 0°/15°/70° to 0°/0°/120°. The postoperative course was free of complications, so that the patient could be discharged with an active ROM of 0°/ 0°/ 110° and complete freedom from pain.

Postoperative image after change to a partially coupled prosthesis and distalization of the joint line by 5mm.
DISCUSSION
The etiology of patella infera remains unclear and is a matter of controversial debate. The risk factors verified to date include previous repositioning osteotomies [3, 4], prolonged postoperative immobilization [5] and the performance of lateral release [2]. Weale concludes that lateral release, by reducing the blood supply to the patellar ligament, leads to its fibrosis and shortening. However, it cannot be ruled out that a biomechanical conflict that requires the performance of lateral release traumatizes the patellar ligament itself. This interpretation is supported by the investigations of Wojtys, who sees excessive scar formation within the context of arthrofibrosis as the cause of patella infera [9]. However, this causal chain can also be reversed, as a low patella has an unfavorable biomechanical effect and itself leads to restricted motion and incorrect weight-bearing, which can result in a chronic inflammatory reaction [10, 11].
In the present case, the intraoperative site showed a correct implantation and centrally running patella, while lateral release had not been performed. We decided against a proximalization of the tuberosity, in order not to reduce the perfusion of the already shortened patellar ligament [12]. The use of a partially coupled system in this case had the advantage, in our view, that a microtraumatization of Hoffa's body and the patellar ligament on the basis of an impingement by the femoral component can be ruled out, as ap-translation of the components to each other is not possible. The long-term outcome of a partially coupled endoprosthesis is, however, to be observed critically with regard to the high degree of activity of young patients.
In the literature, two different mechanisms of action of the HI virus on wound healing are discussed. On the one hand, an increased release of oxygen radicals by neutrophilic granulocytes occurs, which impairs collagen synthesis and is held responsible for the coincidence of HIV and Dupuytren's contracture [7, 8]. On the other hand, a reduction in CD4-positive lymphocytes in peripheral blood is pathognomonic for HIV infection. T-helper-cells have a chemotactic effect, promote the proliferation of fibroblasts and also influence collagen synthesis [6, 13]. The present histological picture, which shows degenerative changes in the sense of a maceration of collagen fibers, the loss of fibrocytes and small foci of lipomatous transformation (Fig. 2), might therefore be explained by a lack of these T-cell functions.
The present findings led us to the hypothesis that there is a connection between the patient's HIV infection and the development of the patella infera. The case presented makes it possible to understand failures experienced in HIV positive patients, despite the correct implantation of a total knee replacement. As a result of its low prevalence of less than 1% in the industrialized countries (WHO 2002), the HI virus cannot explain the occurrence of patella infera after total knee arthroplasty in all cases. However, on the basis of the impaired collagen synthesis and wound healing of an HIV-positive patient, a lower tolerance of the patellar ligament towards microtraumatization and reduced perfusion are conceivable causes of patella infera. We therefore conclude that a particularly soft-tissue sparing surgical method is indicated in the presence of an HIV infection. In this context, discussion in the literature has suggested operating without a tourniquet [14], using a subvastus approach [15, 16], doing without lateral release and preserving Hoffa's body [17].


