All published articles of this journal are available on ScienceDirect.
Total Knee Arthroplasty for Post-Traumatic Proximal Tibial Bone Defect: Three Cases Report
Abstract
Bone stock deficiency in primary as well as in revision total knee arthroplasty (TKA) represents a difficult problem to surgeon with regard to maintaining proper alignment of the implant components and in establishing a stable bone-implant interface. Different surgical procedures are available in these situations, for instances the use of bone cement, prosthetic augments, custom implant, and wire mesh with morsellized bone grafting and structural bone allograft. Structural allograft offers a numerous advantages as easy remodeling and felling cavitary or segmental defects, excellent biocompatibility, bone stock restoration and potential for ligamentous reattachment. In this article we report a short term result of three cases affected by severe segmental medial post/traumatic tibial plateau defect in arthritic knee, for which massive structural allograft reconstruction and primary total knee replacement were carried. The heights of the bone defect were between 27-33 mm and with moderate medio-lateral knee instability. Pre-operative AKS score in three cases was 30, 34 and 51 points consecutively and improved at the last follow-up to 83, 78 and 85 consecutively. No acute or chronic complication was observed. Last radiological exam referred no signs of prosthetic loosening, no secondary resorption of bone graft and well integrated graft to host bone. These results achieved in our similar three cases have confirmed that the structural bone allograft is a successful biological material to restore hemi-condylar segmental tibial bone defect when total knee replacement is indicated.
INTRODUCTION
Bone stock deficiency in primary as well as in revision total knee arthroplasty (TKA) represents a real challenge to surgeon with regard to maintaining proper alignment of the implants and establishing a stable bone-implant interface. Multiple surgical techniques are available in these situations, including use of bone cement, prosthetic augment, custom implant and structural bone allograft. In 1984, Brooks PJ et al. [1], demonstrated the ability of metal augment component to improve the stability of the tibial bone-implant interface; in addition the awful mechanical properties of bone cement have been established [1, 2]. Despite the versatility and a wide variety of augment shapes compatible for the tibial component [3-5], commercially available augments can manage only limited segmental defect, up to 20 mm of depth as recommended by Brand MG, et al. [3]. Even the custom designed implants are not so confidant for total knee arthroplasty with bone defect due to high cost and lack of versatility [4]. The use of fresh allograft transplants in the treatment of large osteochondral defects has been well established in young patients and in particular uni-condylar allograft reconstruction [6, 7].
The structural allograft offers numerous advantages as easy remodeling and filling cavitary or segmental defects, excellent biocompatibility, bone stock restoration, and potential for ligamentous reattachment [1, 8-13]. A common disadvantage of bone allograft includes late resorption, and major risk of infectious disease transmission.
We report a short term results of three patients affected by medial post/traumatic tibial plateau segmental defect in arthritic knee treated by same surgical technique which are primary total knee replacement and massive structural allograft reconstruction.
PATIENTS
Case 1: C.C, female, 62 years old, admitted to our department on January 2003 due to severe residual post/traumatic right knee pain since 10 months. The pain was aggravated by standing and short distant walk which leading to limitation of her usual daily activities. She was suffered of chronic psychic depression, on treatment with antidepressant drugs. Clinical examination reveals mildly swollen tender right knee with varus alignment and extension lag of 15°. Passive range of motion limited between 15-90 degrees. Clear static instability in medio-lateral stress test while is negative in antero-posterior stress tests. She can stand and walk with assistance of one cane. AKS score was 30.
Two views plain radiographs (AP and Lateral) (Fig. 1a), showed mal-union of depressed medial plateau fracture, metphyseal sequestrum fragment and displaced medial fragment with attached medial collateral ligament, laterally sublaxed tibiofemoral articulation, varus deviation of limb mechanical axis of 21°. Moderate osteo-arthritic changes of paltello-femoral joint and wide diaphyseo-metophyseal canal with thin cortices are also noted on both views.

Case 1, Pre-operative plain radiographs.
The plain radiographs of both hips and lower extremities were looks normal. CT scan of right knee confirmed the same X-Ray configuration, pointing out the displacement of bone fragments and the deep cavity defect of medial plateau. According to Anderson Orthopedic Research Institute (AORI) classification, we consider this case as type 2A bone stock defect due to wide medial metaphyseal (28mm height) defect and absence of medial cortex.
Case 2: R.L, female, 65 years old, on October 2008 admitted to our department referring severe recurrent post-traumatic left knee pain since accidental fracture of medial plateau 6 months before. It's associated with static and functional instability that necessitate wearing of hinged knee brace fixed in 30 degree of flexion. She was suffered of chronic panic depression since the age of 34 years, on treatment with anti-depressive drugs. Also had history of multiple myeloma of lower dorsal vertebre treated with drugs and radiation therapy.
Clinical examination revealed moderately swollen left knee, excessive varus alignment in resting position, extension lag of about 15°, passive range of motion restricted between 15-70°, widely unstable tibia-femoral articulation in both antero-posterior and medio-lateral provocative stress. She can stand and walk only with assistance of axillary crutches. AKS score was 34.
Usual radiographs of left knee (Fig. 1b) shows displaced depressed non-union of medial plateau fracture with central fragment sequestrum and displaced medial cortical fragment with the intact insertion of MCL, laterally subluxed tibio-femoral articulation, thin trabecular metaphyseal bone stock with thin cortices and varus knee angulation of 18° from central mechanical axis. Early osteo-arthritic changes on lateral patello-femoral view. CT scan of left knee has confirmed the same finding of plain X-Ray. Tibial bone defect considered to be type 2A of AORI due to large medial segmental (27mm height) defect and absence of medial cortical wall.
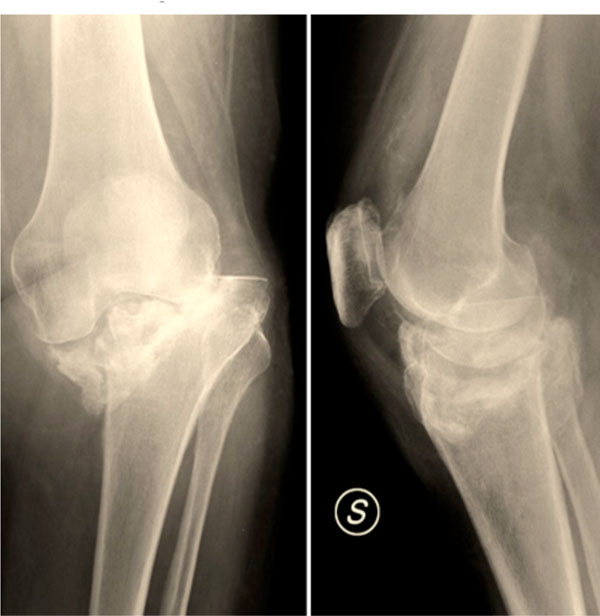
Case 2, Pre-operative plain radiographs.
Case 3: T.R, Male, 59 years old, admitted to our department on March 2009 complaining of sever residual right knee pain and limb gait since car accident occurred one year before, which causing fracture of medial tibial plateau treated surgically with screw fixation, above knee cast. Two weeks later he was candidate for femoro-popletial bypass grafting due to popletial artery contusion and thrombosis. Clinical examination revealed mildly swollen knee with medial tenderness, small antero-medial skin scars. The lower limb resting in severe -varus deviation, with extension lag of 5°, and passive range of motion restricted between 5°-90°; marked medio-lateral joint laxity by applying provocative stress were also present. AKS score was 51.
The plain radiographs (Fig. 1c) showed mal-union of large segment medial palteau depression fixed with one cancellous screw, lateral subluxation of tibio-femoral joint, good metaphyseal bone characters and cortical thickness, varus angulation of 21° from neutral mechanical limb axis and no patello-femoral arthritis. CT scan with 3D reconstruction scan (Fig. 2) of right knee confirmed the severity of the defect considered as type 2A of AORI due to large medial metaphyseal segmental (33mm height) defect and no medial cortical wall seen.

Case 3, Pre-operative plain radiographs.

Anterior and posterior 3D scan sections of knee show sever depressed medial bone stock loss.
So by discussing the clinical and radiographic situation with each one of the three patients, regarding sever pain in unstable sublaxed knee with medial proximal tibial bone loss type 2A of AORI and considering progressive disability even for usual daily activities in such patient age group. We prepared and planned for total knee replacement surgery with stemmed tibial component, posterior stabilizer liner and reconstruction of the medial tibial segmental bone defect with massive structural bone allograft.
SURGICAL TECHNIQUE
All the patients are treated by same surgical technique in which a straight anterior median incision was carried from 2 cm above the patellar pole extended distally to a few cm below the tibial tubercle. After medial para-patellar arthrotomy, the soft tissues insertion and residual adhesions were dissected in more extensive fashion on the medial side in order to expose the old fracture site, with attention to preserve the distal attachment of the superficial medial collateral ligament which more easy to practice a subperiosteal dissection and extend back to the posterior medial corner of the knee as necessary. Both cruciate ligaments were then scarified.
A large type 2A of AORI bone defect was seen in all cases that compromised a major portion of the medial tibial plateau and metaphysis were demonstrated. Adding to residual necrotic fragments adherent by fibrous scar tissue to the rest of proximal tibial bone. Most of the fragments were displaced posterior and medially which were excised after dèbridment of surrounding scar tissues. Resurfacing of Residual medial tibial gap using air saw creating a box with smooth bony walls (Fig. 3), the box created was measured in three dimensions to fashioning the allograft block shape which was different in each case.
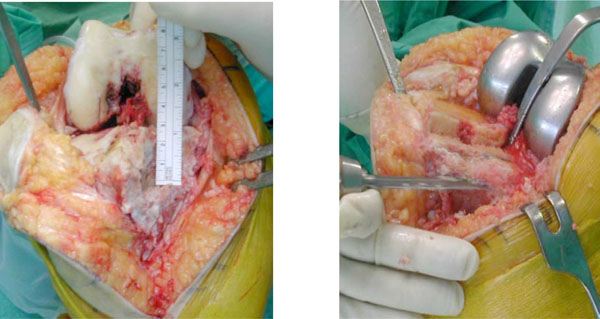
Measurement and preparation of segmental defect, under resection of tibial plateau, in such a way to convert oblique defect to rectangular stepped one.
The femoral and tibial cut preparation is independent of each other, and therefore either of them may be performed first. Probably in cases of major posterior displacement of the medial tibial fragments, starting with the femur cuts could facilitate wide exposure and easer tibial cut preparation. For all cases we have used NexGen LPS (Zimmer, Warsaw, Indiana, USA) complete knee solution instrument case/trial for preparation and implantation of total NexGen LPS (Zimmer, Warsaw, Indiana, USA) prosthesis with stemmed tibial component.
- Femoral preparation. The femoral preparation was performed in usual fashion. We prefer to use a Whiteside line as a reference of rotational alignment for femoral set. we created an entry point at the superior portion of the intercondylar notch just anterior/lateral to the insertion of the posterior cruciate ligament. Then we have settled and engaged the intramedullary alignment guide to the proper side and valgus angle (usually 6°), standard distal cut block was fitted to IM guide until seats on most prominent condyle, the distal femoral cutting block with 3 degree of flexion. Then performed distal cutting. Next carried step was the sizing of the component by applying IM femoral A/P sizing guide into femoral hole until contact distal cut surface and ensured both feet rest on the posterior condyles. The femoral size was seen directly from guide measure. Which were size E in cases 1, 2 and size F in case 3. After we have established the correct distal femoral rotation. We have seated and checked correct size A/P cutting guide and completing the other 4 femoral A/P cuts. Last step we have carried by selecting notch/chamfer guide of same size as A/P cut guide, to perform intercondylar box and drilling holes for the two femoral pugs. For more accuracy we have selected LPS femoral trial size, removed notch/chamfer guide and inserted femoral trial in place to protect the condyles during tibial preparation.
- Tibial preparation. In such non anatomical situation of fractured tibial plateau, it was difficult to find clear entry point for tibial IM guide. So tibial tuboresity was considered as reference point and 15-20mm posterior to it for creating a hole to introduce IM reamer. We have reamed the tibial canal with 10 to 14 mm reamers consecutively until filling of contact with tibial cortices. Lifting in place the last reamer size to be used as IM guide, the depth of reamer introduced was on the 2nd slot line seen on the reamer (200mm) in away to reach tibial isthmus, so we achieved better stability of the reamer. Then the IM guide adapter and tibial cut block was attached to IM guide reamer in place. We have created and ensured correct alignment and height (8-10mm) of tibial cut block using unaffected lateral plateau as referring surface. Fixed the block with 2 or 3 pins and started resection of lateral plateau with oscillating saw blade. We have used the other slots of the cutting guide for additional 5 and 10 mm under-resection with reciprocating saw and in such way we converted the oblique wedge shaped defect into a two-step construct surfaces (Fig. 4).
- Allograft preparation. After measurement of length, width, height of the hemicylindrical trimmed defect space of residual medial condyle, taking into consideration the stepped aspect to prepare and fit the structural allograft. We created and matched a hemi-cylindrical block from proximal tibial mass allograft of our institute bone bank and temporally fixed to host lateral condyle with 2 (2.2mm) K-wires. The graft height should be more than measured defect depth which allows for final cut of created tibial plateau parallel to prepared proximal tibial cut (Fig. 5). Now we reapplied the tibial IM guide and the tibial cut block to finish medial reconstructed tibial stock in manner equal to lateral prepared surface (Fig. 6). To finish tibial preparation we have selected the stemmed tibial plate size and ensured the rotational alignment. Then we have placed the tibial stem drill guide and drilled with stem drill, then have assembled proper size tibial broach and impacted to create etched groove for tibial plate component. At this step, we have fixed the allograft hemi-cylinder reconstruct with definitive 3 titanium screws and then removed the tibial broach guide.
- The knee was balanced in flexion and extension after insertion of trial articular surface of appropriate size. The patella was prepared by removing all osteophytes, synovial tissue around and was resurfaced with thin oscillating saw blade. Preparation of all component size. Continuous pulsating lavage of all bony surfaces for few minutes, preparation of cement Simplex+ Tobramycin, implant the tibial then femoral components and lift the trail articular surface chosen in place for few minutes in knee extension. Last step was insertion of definitive poly-ethylene articular surface insert before reduction and closure of the wound in layers (Fig. 7).
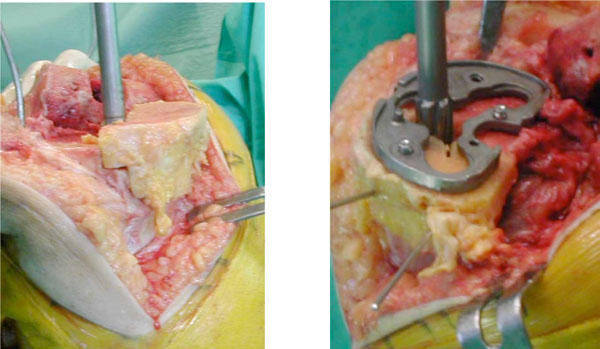
Fitting the allograft, fixation with temporary K-wires and finishing tibial preparation.
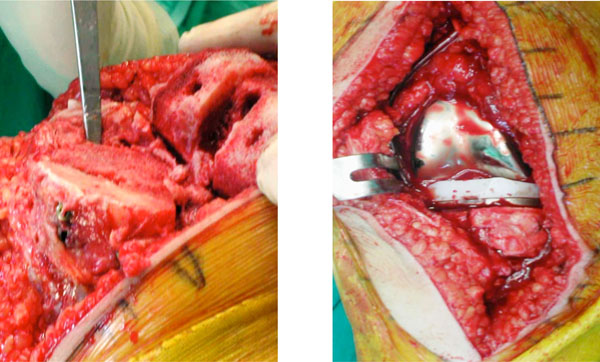
Screws fixation of allograft, selected definitive component implanted in situ.
The postoperative care was same as eventual rehabilitation program for standard total knee replacement, on 2nd postoperative day and after drain removal all the cases were started continuous passive motion exercise with CPM machine in progressive increment of range of motion until they arrived between 0-100 degrees in case 1, 2 and between 0-90 degrees in case 3 and no full weight-bearing were practiced before the hospital discharge for all cases.
RESULTS & DISCUSSION
In our cases report we focused on the reconstruction of the peripheral (segmental) defect of the tibial bone stock secondary to previous tibial plateau fractures. The initial fracture in case 1 and 2 were insufficiency fractures due to low energy trauma related to bone osteopenia. The patients were in fact more than sixty years old females, so that post-menopausal osteoporosis could be considered as causing factor. However it is important to remember that both were for long term in treatment with anti-depressive drugs, which are reported as one of leading factors for bone osteoporosis [14]. The third case was a failure of an inadequate internal fixation. In all three cases the tibial bone deficiency was classified as an Anderson Orthopedic Research Institute (AORI) Type 2A which involved the entire medial tibial plateau (27 to 33mm segmental defect), with subsidence and varus angulation. In the opposite lateral plateau the bone was relatively normal.
In consideration of the patient’s age, the time elapsed from the lesion and early osteo-arthritic damages; we decided that performing a primary total knee arthroplasty as a reasonable solution considering reconstruction of residual bone defect. The use of fresh allograft transplants in the knee for the treatment of large osteochondral defects has been well established [6, 7]. Uni-condylar allograft reconstruction has been reported as a reliable technique in both oncological [6] and non oncological lesion [7], allowing restoration of the knee anatomy and kinematics with satisfactory and functional results. Unfortunately this technique should be considered only in young patients as intermediate solution.
When primary total Knee Arthroplasty is the treatment indication and associate with segmental bone loss of tibial side, multiple surgical options are available. These include use of bone cement, metal augment, custom implant, metal mesh cage with allograft and structural bone allograft [1-3, 5, 8-13, 15]. In 1984, Brooks et al. [1] in the laboratory study demonstrated the ability of metal augment and custom implant to improve the stability of the tibial bone implant interface, as well as the awful mechanical properties of bone cement. The clinical application has subsequently confirmed that theory, so the cement alone or the combination of cement and screws are now considered only in case of relatively small lesion [2,9,13].
Despite the versatility and a wide variety of augment shapes, including hemi-wedges, full wedges, and symmetric spacers, commercially available augments can manage only a limited defect, up to 20 mm of deep [3]. Finally for some authors, metal augmentation should be reserved only in elderly patients in reason of possible deterioration with the time [2, 15, 16]. Porous tantalum cones have been used to restore metaphyseal defect in both primary and revision arthroplasty [5, 17]. Long and Scuderi, have published their results in 16 patients with type T2A/B and T3A/B of AORI classification, in whom tibial tantalum cones where used for cavitary defect, they have achieved promising short term results and have observed good tibial component fixation with well marked tantalum/host bone incorporation [17]. Indeed such promising outcomes, they are still only for large cavitary defects, while segmental patterns required reconstruction with bulk allograft and stemmed prosthesis. Discordant result has been reported in the patterns of revision surgery using massive allografts [18-23].
Clatworthy et al. [22], who studied specifically 52 cases of revision with of uncontained tibial defect treated with bulk allograft, reported a success rate of 92% at 5 years follow-up.
Finally disadvantage of using custom made implants include the lack of versatility and the high cost [1].
The use of morselized allograft in revision TKA where described by Whiteside in 1998, reporting his radiological and histological analysis [23]. More recently Lonner et al. have described the technique of molded wire mesh with bone allograft impaction for large uncontained osseous defects in revision knee arthroplasty. Even if they have got a favorable short term results, however it is deal with a technically demanding solution which requires extensile exposure [24].
Structural bone allograft that, applied since many decades as a biological material to restore bone in different reconstructive procedures, offer numerous advantages, including biocompatibility, bone stock restoration and potential for ligaments reattachment. Regarding their versatility it is possible to treat a wide range of bone deficiency allowing the surgeon to shape the allograft to fit the bone deficit and avoid unnecessary removal of host bone. Finally allograft is relatively cost-effective if compared to the high cost of custom-made implants [2, 8-13, 18-24].
The goals of structural allograft reconstruction are to maximize the stability of the graft-host bone contact and provide a stable platform for fixation of implant. The first step is to remove all the nonviable bone and soft tissue from in and around the defect, the presence of viable bone is absolutely necessary to maximize the likelihood of graft incorporation [14, 25, 26]. Once the bed of the defect is debrided usually an oblique area of bone loss that was previously demonstrated does not provide an adequate stability of the tibial component [15, 25]. Conversion of the oblique peripheral defects into rectangular space with vertical and horizontal surfaces (Fig. 4), before repair has been demonstrate to improve stability for the tibial component fixation [15]. The stepped patterns have also a biological advantage since it allow improving the contact area of the host-graft construct maximizing the probability of graft incorporation [26, 27]. Regarding the choice of the graft as it is important to shape the allograft similarly in order to fit the defect precisely. We have used in all 3 cases an allograft obtained from a proximal tibia. Graft fixation was important step should be taken in consideration, the modality of fixation were discussed and reported to have same precautions of technical details as that given for the other parts of the operation [28]. Even if the screw fixation was theoretically disadvantageous, since the screw hole may act as stress risers. We have stabilized the graft with two or three titanium screws in all cases. To avoid any chance of fixation screws impinging on the definitive implant, the graft was temporary fixed with kirschner wires, and then the trial component with stem was fitted into place. Definitive fixation is completed using partially or fully threaded cancellous screws and washers. In all our case an extension stem of 100 mm was used in accord to decreases proximal axial load of the reconstructed metaphyseal area [1,15]. Standard femoral component with posterior stabilizer liner was the less constrained necessary in all cases since we were able to maintain the distal insertion of the superficial medial collateral ligament in all cases. All cases were discharged within seven to ten days post-operatively and they were able to ambulate with assistance of two crutches without weight bearing on the affected side for three months.
At last follow-up( 95 months in case 1, 27 months in case 2 and 21 months in case 3), they were free of pain, maintained post-operative range of motion and they can walk for several distances without assistance and full weight bearing. Post-operative AKS score was improved to 83,78,85 consecutively. The last plain radiographic control (Fig. 8a-c) evaluate well aligned prosthesis, no signs of prosthetic loosening, well integrated allograft, no allograft resorption or collapse, no demarcation line between bone allograft and host bone.
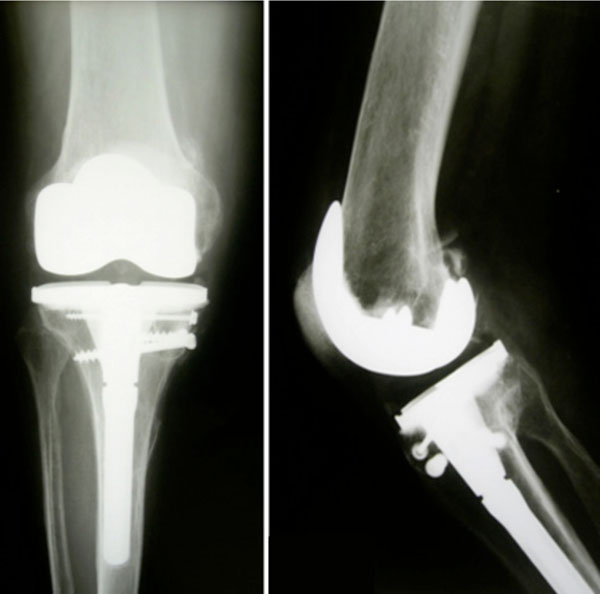
Case 1, last follow-up plain radiographs, 6 years after the surgery.

Case 2, last follow-up plain radiographs, 1 year after the surgery.

Case 3, last follow-up plain radiographs, 8 months after the surgery.
We were able to find only a few reports about the use of structural allograft for post/traumatic segmental tibial defects at the time of primary total knee replacement. In some case reports, Peters C.L, et al. was including altogether three cases where the reconstruction of the medial femoral condyle was associated with the reconstruction of the medial collateral ligament [11]. Other similar cases were reported in the series performed by Haidukewych G.J, et al. [29] that making difficult to know the real evolution of the graft-implant construct. However, in the literature there are variable papers reporting about the use of allograft to restore bone defect during revision knee arthroplasty, especially for uncontained defects which have had demonstrate about 25% of allograft failure [19, 20, 21]. Most of those cases had had a circumferential segmental bone defect of tibial plateau. In a series of Mnaymneh W et al. in early nineties they reported an higher rate of failure up to 50% in case of massive bone loss treated with a whole femoral allograft o a whole tibial allograft metaphyses or both [18]. Engh G.A and Ammeen D.J, whose have reviewed the result of forty-nine knees with severe tibial bone loss found only four cases of failure for reason non directly related to collapse o resorption of the graft. Mostly were contained defect and ten presented an uncontained deficiency of which only four cases were restored with full segment allograft [21]. Therefore six patients had some similarity with our cases of no graft failure were noted. Recently Backstein D, et al. have reported an 85,2% of success rate at an average follow-up of 5,4 years in a series of 68 revision that required a structural allograft for the treatment of uncontained defect [30].
Even if a variability of result are present in the literature, due to the significant difference of the lesion treated, all the authors agree on affirm that the use of a intramedullary stem with a sufficient length to engage diaphyseal bone is mandatory to decrease axial and shear loads to the structural allograft in accordance with previously data emerging from the laboratory [8].
In concern to the results discussed in the literature and the preliminary results achieved in our similar three cases, potentate the structural bone allograft as a successful biological material to restore hemi-condylar segmental tibial bone defect when total knee replacement is indicated.


