All published articles of this journal are available on ScienceDirect.
Improving Timeliness of Patient Discharge Summaries within Orthopaedic Surgery: A Quality Improvement Initiative
Abstract
Purpose
The discharge summary is crucial for transitioning from inpatient to outpatient care, serving as a key communication tool between hospital and primary care providers. Our multi-site, high-volume tertiary care orthopedic division was identified as a low performer in completing discharge summaries within the institutional 48-hour target. This quality improvement initiative aimed to improve the timeliness of discharge summary completion, targeting >80% completion within 48 hours by June 30th, 2023.
Objective
This study aimed to achieve at least 80% discharge summary completion within 48 hours in the Division of Orthopaedic Surgery.
Methods
An interrupted time series study, based on the Institute for Healthcare Improvement’s ‘Model for Improvement’, was conducted. A quality committee, including representatives from each Clinical Teaching Unit (CTU), a resident representative, and two quality facilitators, utilized root cause analysis, stakeholder interviews, process mapping, and driver diagrams. Interventions included implementing an auto-authenticate option, an audit and feedback system, and engaging medical residents and nurse practitioners. Monthly data tracking used statistical process control charts.
Results
Pre-implementation, the completion rate within 48 hours was 48%. Auto-authentication significantly improved completion rates, with 63% completed within 48 hours compared to 16% with manual authentication. Overall, completion rates rose from 48% to 89%, with auto-authentication usage increasing from 50% to 91%.
Conclusion
This initiative significantly improved timely discharge summary completion, meeting targets. Key success factors included stakeholder engagement, timely performance data, and effective root cause analysis. Medical resident involvement and the audit and feedback system fostered improvements, enhancing patient transitions from hospital to outpatient care.
1. INTRODUCTION
The transition from hospital admission to home is a critical point in a patient’s care. Discharge summaries provide patients and community-based care providers with written communication detailing their hospital stay, diagnosis, interventions performed, and follow-up plans. Discharge summaries are crucial to patient continuity of care post-hospital discharge, and the timely transfer of information at the time of discharge helps contribute to a safe and effective transition of care [1]. Delays in dissemination of discharge summaries have been shown to result in higher readmission rates [2-5]. Based on the recognized importance of timely and accurate completion of discharge summaries, Health Quality Ontario (our institution's governing quality body) has highlighted discharge summaries as a priority and has included this on its list of mandatory quality indicators to be reported by hospitals [4].
At London Health Sciences Centre, a multi-site tertiary care hospital, the institutional target for discharge summary completion is >80% completion within 48 hours. At project initiation in June 2022, the Division of Orthopaedic Surgery was identified as a negative outlier, with a completion rate of 48% within the 48-hour target timeline. The Department of Surgery was identified as the lowest-performing department within the hospital, and the Division of Orthopaedic Surgery was identified as the lowest-performing division within the Department of Surgery. Barriers to timely completion of discharge summaries were previously identified as including the high-volume nature of the clinical service, decreasing lengths of stay as a result of other ongoing improvement initiatives, lack of role clarity, and suboptimal use of our electronic medical records.
The discharge summary process at our institution consists of a member of the medical care team (typically a medical student, medical resident, or fellow) dictating a discharge summary, which is transcribed by a transcriptionist into the electronic medical record. This is then authorized by the most responsible physician, who must complete a discharge summary for all inpatients within 48 hours of discharge prior to being disseminated [6].
The purpose of this quality improvement initiative was to improve the timeliness of discharge summary completion, with a specific goal of achieving >80% completion within 48 hours by June 30th, 2023.
2. METHODS
2.1. Project Design and Implementation Strategy
This study utilized an interrupted time series design. The Institute for Healthcare Improvement’s Model for Improvement was used as a framework, and several PDSA (plan-do-study-act) cycles were conducted to implement and evaluate change ideas in an iterative fashion. Four change ideas were implemented between October, 2022, and June, 2023.
2.2. Settings and Participants
This study was conducted in Western University’s Division of Orthopaedic Surgery. The University of Western Ontario's Research Ethics Board has granted this study ethics exemption. This study was reported in accordance with SQUIRE guidelines.
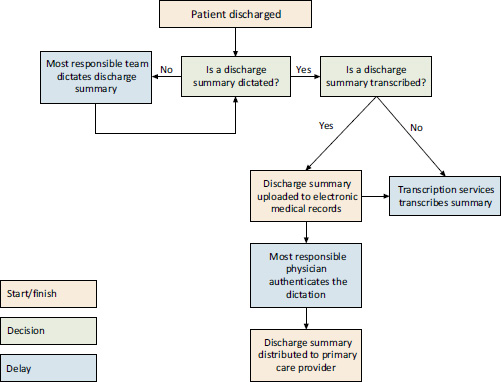
The process mapping of areas where discharge summaries distribution may be delayed.
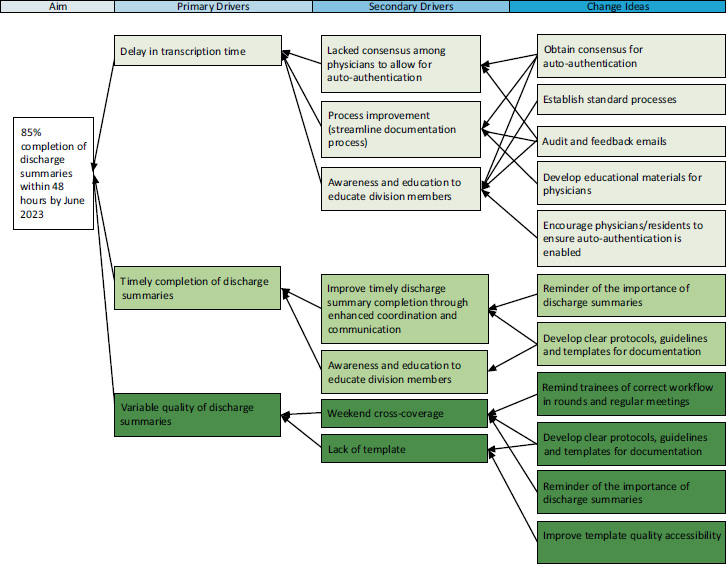
Driver diagram identifying causes of delay and corresponding change ideas.
2.3. Problem Characterization
Process mapping showcased areas of delay in the rate at which discharge summary documents were completed (Fig. 1). A driver diagram (Fig. 2) as well as a fishbone diagram (Fig. 3) identified specific causes of delay in the successful completion of discharge summaries. An analysis of the driver diagram highlighted how change can be implemented for specific challenges as a response to encourage and follow through with improvements.
2.4. Stakeholder Involvement
Key stakeholders were identified and engaged early in the improvement process. An Orthopaedic Surgery Quality Committee was formed to address this and other improvement projects, with representatives from each Orthopaedic Surgery Clinical Teaching Unit (CTU) along with a resident representative, a National Surgical Quality Improvement Program (NSQIP) case reviewer, and two quality facilitators. Further, nurse practitioners were engaged from specific CTUs, who were identified as negative outliers within our division. Physicians from the Departments of Medicine and Otolaryngology, who had previously worked on similar initiatives within their own divisions, were also recruited to serve as project advisers.
2.5. Interventions
The first intervention consisted of educational efforts and stakeholder engagement to ensure that team members were aware of the importance of timely discharge summary completion and to identify any barriers to accurate and timely completion. Educational efforts were repeated with the onboarding of new residents in June of 2023.
The second intervention consisted of an auto-authentication feature for discharge summaries. Time to authentication was identified as a major barrier to timely discharge summary completion, with authentication times exceeding 72 hours in many cases. Departmental consensus was reached on the feasibility of allowing discharge summaries to be auto-authenticated without compromising patient safety, and educational initiatives for team members were conducted to ensure this feature would be used at the time of dictation.
The third intervention consisted of an audit and feedback system that was developed to inspire collegial competition in order to improve completion. The Division of Orthopaedic Surgery is divided into six CTUs, each of which has 3-7 faculty members. On a monthly basis, data was compiled and circulated across the division to comment on overall performance and to identify the strongest and weakest performing CTU each month.
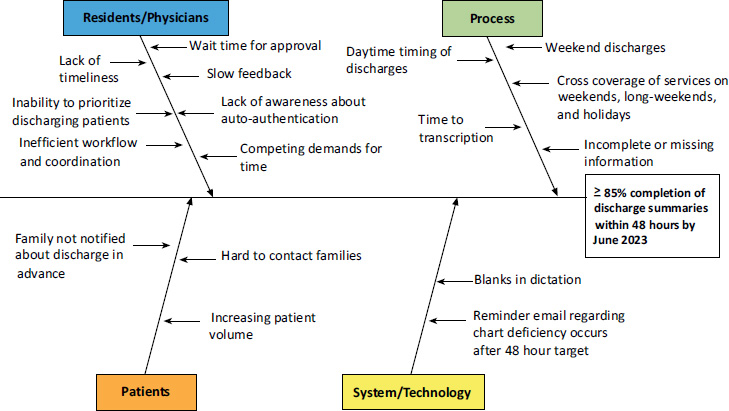
Fishbone diagram revealing specific areas of delay.
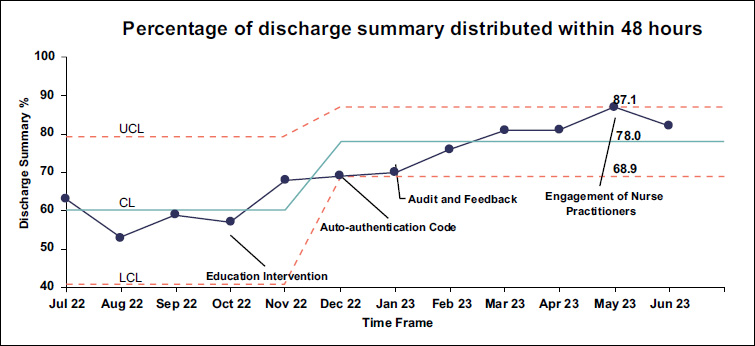
The statistical process control chart shows the percentage of discharge summaries distributed within 48 hours. Arrow markers identify each intervention. CL, center line; LCL, lower control limit; UCL, upper control limit.
The fourth intervention consisted of the engagement of nurse practitioners to assist in completing discharge summaries. This was specifically targeted at lower-performing CTUs and for Monday morning completion for patients who were discharged over the weekend, as Monday mornings were identified as a particularly busy time for medical residents.
2.6. Performance Measures and Evaluation
Performance was evaluated using process, balancing, and outcome measures. The primary outcome measure was the proportion of discharge summaries completed within the 48-hour target. Process measures included the proportion of discharge summaries using auto-authentication. To evaluate the effectiveness of auto-authentication, the percentage of discharge summaries dictated with manual authentication within 48 hours was compared to the percentage of discharge summaries dictated with auto-authentication task code 10 within 48 hours. Furthermore, process measures included the proportion of discharges completed on weekends and a comparison of performance between weekend discharges and weekday discharges. Balancing measures were identified to include possible reasons for the delay in discharge summary completion, using feedback from residents, physicians, and consultants. Semi-structured interviews were also conducted with several multidisciplinary members of the care team to ensure that no negative impacts on overall workflow were identified as a result of a newfound focus on timely discharge summary completion.
Monthly data were collected for 12 months, from June, 2022 to June, 2023. Statistical process control charts were developed to demonstrate performance over the duration of the study period, and special cause variation was identified using Shewhert’s methodology. Data were displayed at meetings and communicated to all stakeholders monthly as audit and feedback.
3. RESULTS
This project led to a significant improvement in the rate of discharge summary completion within 48 hours, from 48% in the three months prior to project initiation to 87.1% at project completion. The statistical process control chart (Fig. 4) demonstrates progressive and sustained improvement in discharge summary completion rates. The chart is labelled with the timing of all four of the interventions.
In July, 2022, 257 discharge summaries were completed within 48 hours among all CTUs compared to 354 discharge summaries completed within 48 hours in June, 2023.
4. DISCUSSION
Timely and accurate completion of discharge summaries is a challenge faced by many healthcare systems [1-3, 5, 7-10]. Primary care providers (PCPs) and other healthcare providers struggle with treating patients if they do not have adequate information about their patients' health status readily available [3, 11-14]. This can cause delayed or inaccurate communication between hospital-based physicians and primary care physicians, resulting in an inaccurate representation of a patient's recent interventions, hospitalizations, drug plans, or other intended care plans [2, 13, 15]. Our quality improvement initiative successfully improved our performance in this important quality indicator, allowing us to surpass our institutional and provincial targets. This also elevated the Division of Orthopaedic Surgery to the second-highest-performing surgical division and increased the hospital-wide metric from a total of 72% to 76%.
There were several critical features of this project that we believe contributed to the overall success of this initiative. Firstly, broad stakeholder engagement and buy-in helped ensure our division was working collaboratively towards this common goal. Additionally, the engagement of residents and nurse practitioners helped with identifying the unique barriers to success for different CTUs and ensuring that we could address those with change ideas.
Secondly, access to timely and detailed data helped target interventions where they would be most effective. For example, it was identified that time to authentication was a key driver of delays to discharge summary completion, with authentication times of >72 hours in several months. This allowed us to develop and implement the auto-authentication feature, ensuring that we could bypass this lengthy authentication process.
Finally, the audit and feedback system was essential in achieving ongoing improvement in this area. This ensured that attending physicians, medical trainees, and nurse practitioners across the division were paying attention to this important metric. Additionally, it helped leverage the competitive nature of orthopaedic surgeons to help foster collegial competition and provided the incentive for lower-performing CTUs to improve their performance on a monthly basis. In four of the nine months, the lowest-performing CTU in one month became the highest performer in the subsequent month, likely as a result of this audit and feedback system.
When implementing the audit and feedback system, a decision was made to disseminate the results on a CTU level rather than identifying individual providers. This ensured that no individual attending surgeons or trainees felt ‘singled out’ for their performance. Individual self-performance data was made available to each provider upon request.
Subdividing the results on a CTU level rather than an individual provider level also allowed the improvement team to work with the identified CTUs physician extenders. When two specific CTUs were noted to consistently have lower completion rates, three nurse practitioners who support these CTUs were engaged in the project. Slight changes were made to the workflow based on their feedback, which allowed them to become more easily involved in the discharge summary completion process.
Another important feature that contributed to the success of this initiative was broad institutional support. Improving discharge summary completion was identified on institutional and departmental levels as a priority and was included as a key metric within the hospital’s quality improvement plan. As a result, there was good organizational consensus regarding the importance of this initiative.
This study builds on other studies in the literature demonstrating that simple quality improvement projects can be effective in improving discharge summary completion rates [1, 7]. Using similar strategies to our study, You et al. [8] completed a quality improvement project within the Department of Otolaryngology at our institution and demonstrated that the implementation of an auto-authentication and audit and feedback system increased the timeliness of when discharge summaries were being distributed. Our quality improvement initiative commenced using strategies similar to those applied by You et al. [8]. These were then tailored to some of the unique challenges within the Orthopaedic Surgery division. Specifically, the fact that at our institution, Orthopaedic Surgery is a high-volume service with many patients admitted for <24 hours led to the residents providing CTU coverage to take a more team-based approach to discharge summary completion.
Similarly, while this study outlines strategies to improve discharge summary completion that can be spread and scaled more broadly, it is important to tailor them to the local context in which they are being applied. This project’s success was dependent on consensus among providers to auto-authenticate the discharge summaries, accurate and timely data provided by our quality and performance team, and a collaborative and engaged group of residents and attending surgeons. Without each of these features, the aforementioned improvement strategies may have been less impactful. The strategies and collaboration described were specific to our centre, and thus limit the generalizability of the results of this project.
Several challenges were encountered during the implementation of this study. These included frequent changeover of medical trainees and the introduction of visiting medical trainees from other sites, necessitating multiple formal and informal educational sessions for trainees. The monthly audit and feedback emails also helped address this challenge by serving as a regular reminder of the necessity to complete discharge summaries.
Additionally, the extremely busy nature of the clinical service posed challenges. Most resident groups developed a standardized workflow, where the primary resident supervising a patient would complete the discharge summary the following morning. This posed a challenge on weekends. Resident coverage decreased from an average of 6 residents per site during weekdays to an average of 1.5 residents per site on weekends. Combining this with the busy nature of weekend call coverage meant that very few discharge summaries were being completed on weekends. Discharges on the weekends had their discharge summaries completed on Monday mornings, but our 48-hour completion target meant that Friday discharges were frequently not completed within the required time frame.
Additionally, due to personnel changes in our institution’s Surgical and Quality and Performance Departments, we were unable to continue data collection beyond June, 2023, as data was no longer reviewed regularly or systematically. While we achieved excellent improvement over the study period, we were unable to assess the sustainability of this improvement.
Overall, our study was successful in improving the discharge summary completion rate within 48 hours from 48% to 87.1% over the nine-month study period. The improvement strategies outlined in this study can be utilized to sustain improvement at our institution and can be applied to facilitate similar improvements at other institutions with adaptations to the local environment.
CONCLUSION
A dedicated quality improvement initiative can significantly improve the timeliness of discharge summary completion in a high-volume tertiary care orthopaedic surgery unit, with significant positive implications for patient care through transitions of care. Critical drivers of improvement included broad stakeholder engagement and buy-in, audit and feedback systems, streamlined processes, and access to timely and detailed data.
AUTHORS’ CONTRIBUTION
E.S., N.S., S.N., C.D., K.E., and R. K.: Proposed the project rationale; E.S., N.S., S.N., C.D., K.E, J.D, C.P., and R.K: Developed the project plan; S.N., C.D., K.E., and R.K: Led stakeholder engagement; E.S., N.S., S.N., C.D., K.E, J.D., C.P., and R.K.: Interpreted and analyzed data and carried out Plan-Do-Study-Act cycles; E.S., N.S., J.D., and C.P.: Prepared the manuscript.
LIST OF ABBREVIATIONS
| CTU | = Clinical Teaching Unit |
| NSQIP | = National Surgical Quality Improvement Program |
ETHICAL STATEMENT
We received a Quality Improvement Ethics Exemption from Western University's Research Ethics Board.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Dr. Julie Strychowsky and Dr. Louise Moist for their guidance and the quality and performance team at London Health Sciences Centre for providing timely and accurate data. Most importantly, they would like to appreciate the orthopaedic surgery residents at Western University as they were instrumental in the success of this project, and their engagement and dedication to patient care allowed for all of these improvements to be successful.


