SYSTEMATIC REVIEW
Hip and Knee Arthroplasty in Patients with Mucopolysaccharidosis: A Systematic Review
Kimon Toumazos1, Nicole Williams2, *
Article Information
Identifiers and Pagination:
Year: 2023Volume: 17
E-location ID: e187432502212290
Publisher ID: e187432502212290
DOI: 10.2174/18743250-v16-e221228-2022-7
Article History:
Received Date: 17/05/2022Revision Received Date: 14/10/2022
Acceptance Date: 04/11/2022
Electronic publication date: 23/02/2023
Collection year: 2023

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Aims:
To review the use of knee and hip arthroplasty for patients with mucopolysaccharidoses (MPS) to inform clinicians and patients of this emerging area of orthopaedic practice and direct future studies.
Patients and Methods:
An Embase database review was conducted according to Preferred Reporting Item for Systematic Reviews and Meta-analyses (PRISMA) guidelines to identify relevant published articles. Extracted information included demographic data, indications for surgery, surgical details, post-operative outcomes and complications.
Results:
Ten articles reported 15 patients with a total of 5 knee and 20 hip arthroplasties were identified and included. The mean age was 28.3 years and mean follow up duration for knee and hip arthroplasties was 3.6 years and 5.1 years respectively. Indications for surgery included pain in all patients, reduced range of motion, genu valgum and joint instability. Complex arthroplasty techniques were required including extensive soft tissue releases, instrumentation modification, screw fixation and modular/dysplasia arthroplasty components. There were four intra-operative fractures in hip arthroplasty patients and one hip arthroplasty underwent revision due to loosening. Pain resolution was documented for all knee arthroplasties and 90% of hip arthroplasties, whilst complications occurred in 9/20 (45%) of all arthroplasties.
Conclusion:
Arthroplasty surgery in this rare patient group can be successfully performed for pain relief and improvement in function with careful pre-operative planning and multidisciplinary management. Treating teams should be encouraged to share their experience to contribute to our understanding of indications, technique and outcomes for arthroplasty procedures in MPS patients.
1. INTRODUCTION
Mucopolysaccharidosis (MPS) [1] has long been a life-limiting disease, but recent medical advancements have resulted in remarkable changes in prognosis. MPS, a form of lysosomal storage disease, is caused by deficiencies of enzymes involved in the breakdown of glycosaminoglycans (GAGs) [2].GAGs play an important role in cell biology, and signalling pathways and impairment of these molecules lead to multisystemic involvement with a range of somatic, neurologi-cal, haematological, and ocular symptoms [2]. There are seven major types of MPS (MPS I – Hurler syndrome, MPS II – Hunter syndrome, MPS III Sanfilippo syndrome, MPS IV – Morquio syndrome, MPS VI – Maroteaux-Lamy syndrome, MPS VII – Sly syndrome, MPS IX – hyaluronidase deficiency). The syndromes are differentiated by their associated enzyme deficiency and further subtypes, including less-rapidly progressive and intermediate phenotypes such as MPS, IS – Scheie syndrome, and MPS IH/S – Hurler/Scheie syndrome [3].
The musculoskeletal manifestations involving the hip and knee result from GAG-related dysregulation of connective tissue homeostasis and lead to major issues for the orthopaedic surgeon, such as short stature, skeletal dysplasia, joint stiffness, or hypermobility [2]. Joint stiffness and contractures are found in all forms of MPS except for MPS IV and IX. They can be attributed to defective bone modelling in combination with thickened joint capsules secondary to GAG deposition and fibrosis [3]. Patients may present with swollen, stiff joints but without the signs of local inflammation such as erythema and warmth seen with diseases such as rheumatoid arthritis or juvenile idiopathic arthritis [4]. Short stature in MPS follows GAG deposition in the growth plates, disturbing endochondral ossification. Dysostosis multiplex is the characteristic pattern of skeletal dysplasia described in MPS. GAG deposition in the articular cartilage leads to increased apoptosis of articular chondrocytes through mechanisms including activation of lipopolysaccharide (LPS) signalling pathway and reduced differentiation of the chondrocytes leading to poor mineralisation of bone [5]. The LPS pathway is activated as the GAG accumulation has structural similarities to LPS. Hence the musculoskeletal manifestations of MPS are predominantly targeted toward cartilage formation rather than the bone [4].
Modern advancements in hematopoietic stem cell transplantation and enzyme replacement therapy have drastically changed prognosis in patients with MPS [6]. With the increased age of patients with this disease and improvement in many systemic manifestations but minimal improvement in the musculoskeletal manifestations, orthopaedic interventions are increasing [7]. Many patients with MPS types I, II, IV, and VI will undergo orthopaedic procedures during their lifetime due to the associated skeletal dysplasia, nerve compression syndromes, and spinal pathology. Common orthopaedic procedures include guided growth surgery, osteotomies, and soft tissue releases [7, 8].
Arthroplasty is emerging as a procedure in this patient group, as improved multidisciplinary care and systemic therapy mean that patients are living longer, with improved functionality, and seeking a better quality of life [7]. Still, systemic therapies have not been shown to reliably ameliorate joint pathology.
This study aims to summarize the literature on knee and hip arthroplasty performed in this patient population to provide information for clinicians managing this condition and define the direction for future studies.
2. MATERIALS AND METHODS
A literature review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [9]. A search of published literature was conducted in April 2021 by a qualified librarian using the Embase database. Search terms included combinations of “MPS,” “mucopolysaccharidosis,” “arthroplasty,” “replacement,” “hip,” and “knee.” A screening process was then conducted with a review of titles and abstracts. Articles were excluded if they did not include sufficient information or when they were general review articles on MPS (Fig. 1). The initial search identified 22 articles (Fig. 1), of which three were excluded as they reported MPS undergoing cardiac or upper limb procedures [10-12]. Seven general review articles on MPS were excluded, and two articles mentioned arthroplasty but had insufficient information to be included in the final data [13, 14]. The included ten articles reported 15 patients with 25 arthroplasties, 5 knee arthroplasties [15, 16], and 20 hip arthroplasties [17-24].
Information collected included demographic data (gender, MPS type, height and weight, age, previous treatment), surgical indications (symptoms, physical examination findings), surgical details (approach, prosthesis details, intraoperative and early postoperative complications), and postoperative data (timing of final follow up, function quality of life, late postoperative complications).
Descriptive statistics were used with normally distributed data, including mean and standard deviation.
3. RESULTS
3.1. Patients
There were 5 males and 10 females with a mean age of 28.3 years (range 16-43 years). The mean height and weight were 144.8cm and 52.9kg, respectively. MPS type was MPS type IH (2 patients) [17, 18], MPS IS (2 patients) [22], MPS III (2 patients) [23], MPS IV (8 patients) [15, 16, 20, 21, 24] and MPS VII (1 patient) [19] (Table 1). All five patients who underwent knee arthroplasty had a diagnosis of MPS IV [15, 16]. Various MPS types made up the hip arthroplasty group [20, 21, 23, 24]. Five patients underwent unilateral surgery [16-18, 22], and 10 patients had bilateral surgery [15, 19-24]. Pre-surgery 7 patients required small assistance [3, 6, 7, 9, 13, 16, 21-24], 2 patients required mobility aids [23, 24], and 3 patients were wheelchair dependent [15, 17, 20]. Pre-surgery ambulatory status was not reported for 3 patients [16, 18, 19]. Eight studies reported the year of surgery, with the earliest dated 1987 [19].
| Study | MPS Type | Age/Gender | Joint, Side | Follow-up (Yrs) | Complication |
|---|---|---|---|---|---|
| Atinga et al. 2008 | 4 | 22M | Knee, R | 5 | Severe blood loss requiring ICU admission. Acute hepatic transaminitis (no cause identified). |
| Atinga et al. 2008 | 4 | 22M | Knee, L | 5 | Peroneal nerve palsy. Recovered in 12 months. |
| de Waalmalefijt et al. 2000 | 4 | 43F | Knee, R | 4 | Required vastus intermedius release due to restricted flexion. |
| de Waalmalefijt et al. 2000 | 4 | 42F | Knee, L | 3 | - |
| de Waalmalefijt et al. 2000 | 4A | 44F | Knee, R | 1 | - |
| Gautam et al. 2008 | 1H | 17F | Hip, L | 8 | Intra-operative fracture. |
| Guffon et al. 2019 | 7 | 29M | Hip, R | 4 | Loosening of stem and cup 4 years post-operation. The limb length discrepancy of the operated leg is 5cm longer. |
| Ilyas et al. 2017 | 4 | 16F | Hip, R | 15 | Intra-operative fracture. |
| Ilyas et al. 2017 | 4 | 16F | Hip, L | 15 | - |
| Leonard et al. 2011 | 4 | 26M | Hip, L | 5 | - |
| Leonard et al. 2011 | 4 | 26M | Hip, R | 5 | Intra-operative fracture. |
| Pietri et al. 2005 | 1S | 38M | Hip, L | 5 | - |
| Pietri et al. 2005 | 1S | 38M | Hip, R | 5 | - |
| Pietri et al. 2005 | 1S | 43M | Hip, L | 1 | - |
| Pryce et al. 2010 | 4B | 25F | Hip, R | 7 | - |
| Pryce et al. 2010 | 4B | 25F | Hip, L | 7 | - |
| Pryce et al. 2010 | 3 | 17F | Hip, R | 5 | - |
| Pryce et al. 2010 | 3 | 18F | Hip, L | 5 | - |
| Pryce et al. 2010 | 3 | 18F | Hip, R | 3 | - |
| Pryce et al. 2010 | 3 | 18F | Hip, L | 3 | - |
| Tassinari et al. | 4 | 29F | Hip, R | 1.6 | Sciatic nerve palsy. Recovered by the end of the follow-up period. |
| Tassinari et al. | 4 | 29F | Hip, L | 1.6 | - |
| Tassinari et al. | 4 | 34F | Hip, R | 1.5 | - |
| Tassinari et al. 2008 | 4 | 34F | Hip, L | 1.5 | Intra-operative fracture. |
| O'hEireamhoin et al. 2011 | 1H | 23F | Hip, L | 2 | - |
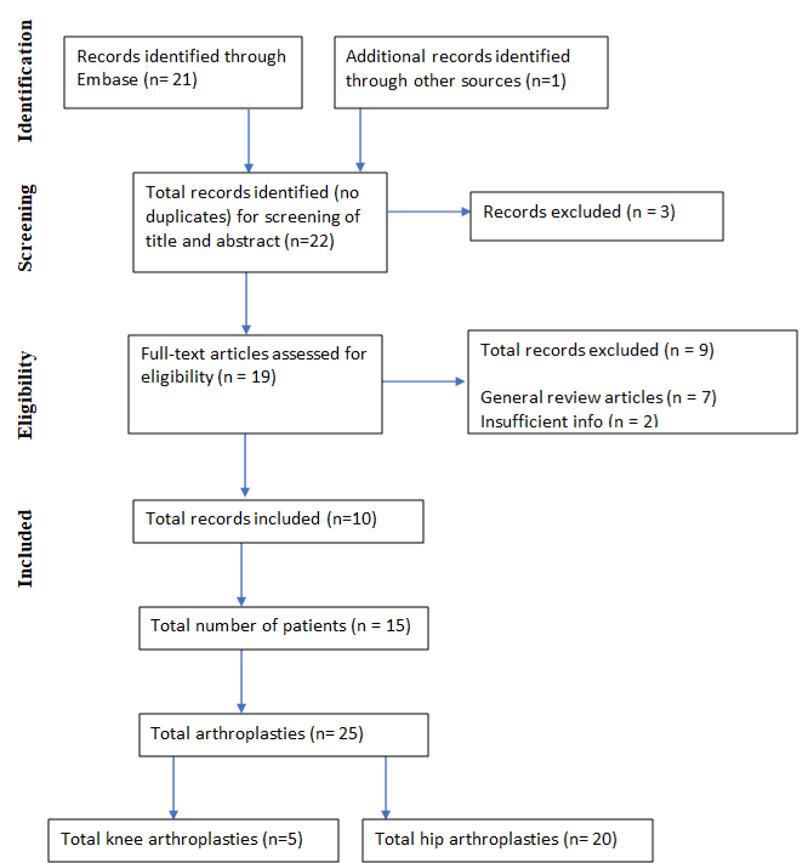 |
Fig. (1). Prisma 2009 Flow Diagram for including MPS arthroplasty studies 8. |
3.2. Indications for Surgery
All patients reported significant pain pre-operatively. Of the 15 patients where lower limb alignment was reported, all had genu valgum. Previous orthopaedic surgery was reported for three patients (1 knee, 2 hip arthroplasties) involving both affected and unaffected limbs [16, 17, 19].
For patients undergoing knee arthroplasty, the pre-operative range of motion (ROM) mean was 136 degrees flexion (SD, 20.7). Instability/joint laxity was reported in 4 knees and not reported in one case [15, 16].
For patients undergoing hip arthroplasty, the pre-operative extension was reported in 13/20 patients with a mean fixed flexion deformity of 15 degrees (SD, 16.5). Pre-operative flexion, abduction, and adduction range were reported for 11/20 surgeries with a mean of 74 degrees (SD, 17.5), 11.4 degrees (SD, 13.8), and 8.2 degrees (SD, 8.4), respectively. Mean internal rotation (10/20 hips) was 1 degree (SD, 2.1); external rotation (10/20 hips) was 8.1 degrees (SD, 10.2) [18-21, 23, 24]. Of the 15 hips that had preoperative radiographs, the mean caput-collum-diaphyseal angle was 139.7, with seven showing coxa valga [18, 23, 24]. Failure of conservative treatment and/or progression of the deformity was reported in six hip arthroplasties (four patients) [19, 23]. One patient (MPS III) presented with bilateral avascular necrosis of the femoral heads [23].
3.3. Surgical Details
A standard midline incision was reported for two knee arthroplasties; however not specified if the approach was lateral or medial parapatellar [15]. The approach was not described for the remaining knee arthroplasties. All knee arthroplasties used cemented components. Extensive soft tissue releases were required in all knee surgeries; however, in one knee arthroplasty, this was limited due to excessive bleeding [15]. All knee arthroplasties used some form of constrained components. Two by Atinga et al. were described as fully constrained, and three by de Waal Malefijt were described as posteriorly stabilised [15, 16]. Intraoperative shortening of the femoral component was performed in two knee arthroplasties using a diamond saw to accommodate the short limb length [15].
Seven of the 13 approaches reported for hips were posterior [17, 18, 20, 22] and six anterolateral [21, 24]. Of the 19 hip arthroplasties where the use of cement was reported, the acetabular component was cemented in 42% (8/19) cases [20, 23], and femoral stems were cemented in 58% (11/19) of surgeries [20, 22, 23]. The acetabular component size was reported in 12/20 cases with a mean of 45.2mm (range 36-50). The distal component size was reported in 9/12 cases, with dedicated hip dysplasia, short stem, or modular stem designs used in all cases. Screw fixation of the acetabular component was used in 50% (10/20) of cases [21, 22, 24]. Component materials for hip arthroplasty were reported for 13 cases which included metal on metal (1 case) [18], metal on polyethylene (8 cases) [20, 23, 24], and ceramic on ceramic (4 cases) [21, 24]. Intra-operative calcar/proximal femur fracture occurred in 20% (4/20) hip arthroplasty cases [18, 20, 21, 24]. These were all managed with cerclage wire fixation.
Anaesthetic details, tourniquet use, concomitant osteotomies, and hip soft tissue releases were infrequently reported (Tables 2-4).
| Arthroplasty Component | Number of cases (%) | Neurological Compromise | Fracture | |
|---|---|---|---|---|
| Approach | Midline Not reported |
2 (40) 3 (60) |
1** 0 |
0 0 |
| Stability of prosthesis | Constrained Not-constraint |
5 (100) 0 (0) |
1** 0 |
0 0 |
| Cemented | Yes No |
5 (100) 0 (0) |
1** 0 |
0 0 |
| Intraoperative prosthesis modification | Yes No |
2 (40)* 3 (60) |
1** 0 |
0 0 |
| Soft Tissue release | Yes No |
5, all extensive (100) 0 (0) |
1** 0 |
0 0 |
| Arthroplasty Component | Number (%) | Prosthesis Failure (1, Guffon et al.) | Intraoperative Fracture (4) | Neurological Compromise (1**) | |
|---|---|---|---|---|---|
| Approach | Anterolateral Posterior* Not reported |
7 (35) 6 (30) 7 (35) |
0 0 1 |
2 2 0 |
1 0 0 |
| Cemented Acetabular | Yes No Not reported |
8 (40) 11 (55) 1 (5) |
0 0 1 |
1 3 0 |
0 1 0 |
| Cemented Femoral | Yes No Not reported |
11 (55) 8 (40) 1 (5) |
0 0 1 |
1 3 0 |
0 1 0 |
| Type of Prosthesis | Metal on Metal Metal on Poly Ceramic on Ceramic Insufficient information |
1 (5) 8 (40) 4 (20) 7 (35) |
0 0 0 1 |
1 1 2 0 |
0 1 0 0 |
| Screw Fixation (acetabular) | Yes No |
10 (50) 10 (50) |
0 1 |
2 2 |
1 0 |
| Study | Acetabulum Size (mm) | Stem Size |
|---|---|---|
| Gautam et al. | 44 | Size 1, short stem (ProximaTM Hip Duofix, Depus Synthes) |
| Ilyas et al. | 40 | Size 5 DDH stem, small diameter (Protek, Sulzer Medica, Winterthur, Switzerland) |
| Ilyas et al. | 36 | Size 5 DDH stem, small diameter (Protek, Sulzer Medica, Winterthur, Switzerland) |
| Leonard et al. | 50 | Size 3, modular (ABG II, Howmedica) |
| Leonard et al. | 50 | Size 3, modular (ABG II, Howmedica) |
| Pietri et al. | 48 | Not reported. |
| Pietri et al. | 48 | Not reported |
| Pietri et al. | 48 | Not reported |
| Tassinari et al. | 40 | Size 13, modular (Wagner cone, Zimmer) |
| Tassinari et al. | 40 | Size 13, modular (Wagner cone, Zimmer) |
| Tassinari et al. | 48 | Size 9, modular (Apta, Adler Ortho) |
| Tassinari et al. | 50 | Size 9, modular (Apta, Adler Ortho) |
3.4. Postoperative Details
The mean reported follow-up for knee arthroplasty was 3.6 years (range 1-5 years) and 5.1 years (range 1-15 years) for hip arthroplasty. There was no reported peri-operative mortality in the cohort.
One knee arthroplasty patient underwent vastus intermedius release 9 months postoperatively due to restricted flexion of 65 degrees during rehabilitation [16]. One patient who underwent knee arthroplasty required intensive care unit (ICU) admission for severe blood loss. There were no other reports of ICU admission as precautionary or a consequence of surgery [15]. One knee arthroplasty patient developed a post-operative peroneal nerve palsy that had resolved at the final follow-up [15]. One knee arthroplasty patient developed transaminitis, which was attributed to a combination of tissue hypo-perfusion and hypoxia on a background of regular use of paracetamol [15]. All knee arthroplasty patients reported significant pain improvement at the final follow-up. Oxford Knee Scores (OKS) for two knee arthroplasties (one patient) showed improvement from 22 to 39 at five years [15]. International Knee Society (IKS) score for three knee arthroplasties (two patients) reported scores of 91, 90, and 90 at follow-up with no pre-operative measures [16].
One hip was revised due to the loosening of the femoral stem and acetabular component four years post-initial operation [19]. One hip arthroplasty had post-operative sciatic nerve palsy [24], which had resolved at the final follow-up. Significant pain improvement was achieved in 90% (18/20) of hip arthroplasties, with one patient reporting moderate pain at follow-up [18] and one reporting ongoing pain-causing disability [19]. The hip group achieved 80% (16/20) of arthroplasties requiring no aids post-operatively [18, 20-24], 20% (4/20) required aids [17, 19, 23], and no patients used wheelchairs postoperatively. Only one hip arthroplasty reported Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and Harris Hip Scores (HHS) with significant improvements in both measures pre-operatively to post-operatively [25]. One hip arthroplasty patient reported a symptomatic limb length discrepancy of 5cm requiring shoe raises on the contralateral side [18].
Overall, there were 9 (45%) complications, including fractures (four, all hip arthroplasty), loosening (one hip arthroplasty), nerve damage (one hip, one knee), post-operative stiffness (one knee), and severe blood loss (one knee) (Table 1).
4. DISCUSSION
With medical advancements in patients with MPS, arthroplasty of the hip and knee is becoming more common in the multidisciplinary approach. This review collates the current literature on arthroplasty in this rare patient group.
Ten publications reporting knee or hip arthroplasty in 15 patients were identified. Publication bias is difficult to avoid, given the rarity of the disease. Authors may selectively publish complication data; conversely, authors may prefer to publish successful cases. The largest case series of arthroplasty in MPS reported three patients with six hip arthroplasties [23].
The musculoskeletal complications of MPS are well-described and do not satisfactorily respond to modern medical management. These complications include short stature, skeletal dysplasia (termed dysostosis multiplex in MPS), joint stiffness (particularly MPS I, II, VII) or hypermobility (particularly MPS IV), and avascular necrosis (particularly MPS III) [4]. Impaired ossification associated with dysostosis multiplex results in hip dysplasia and genu valgum. Attempts in children to prevent the development of hip osteoarthritis with osteotomies have been proven ineffective [26].
Papers in this review did not detail the multidisciplinary management of patients in the peri-operative period, but this is paramount for safe surgery in MPS patients. Patients with MPS are at high risk for anaesthetic complications due to airway, respiratory and cervical spine manifestations of the disease [27]. With increasing numbers of surgeries being performed on MPS patients, there are increasing case reports of the devastating complication of peri-operative thoracic spinal cord infarction in MPS patients [28]. This complication occurs in the anatomical watershed region of the thoracic spine vascular supply. Recommendations to minimise its occurrence include lower limb neuromonitoring in lower extremity surgeries, careful patient positioning, and judicious blood pressure control [29]. Pre-operative whole spine MRI has been recommended to evaluate the cervical spine and ensure no anomalies to contraindicate spinal anaesthesia [21, 27, 28].
This review highlights the importance of pre-operative planning in this patient group [8]. Intraoperative shortening of the femoral component was required for two knee arthroplasties to accommodate short limb-length and multi-planar deformity [15]. All knee arthroplasties were performed in MPS IV patients. These patients have severe, progressive genu valgum and joint hypermobility, requiring some form of constraint with a prosthesis, and there is the risk of peroneal nerve palsy post-operatively [15, 30]. De Waal et al. reported peroneal palsy in the one knee arthroplasty, which did not have an intra-operative release of the peroneal nerve. Two knees in the same series that underwent nerve release did not have this complication [16]. Atinga et al. described using the tourniquet to help prevent bleeding when undergoing extensive soft tissue releases in patients undergoing knee arthroplasty [15]. Given the small stature of this patient group, a paediatric tourniquet is usually required.
Dysplasia hip, modular, and small/short diameter stems were used to accommodate the varied femoral osteology, including small size and abnormal versions in MPS patients [21]. The use of screw fixation in half the hip arthroplasties may reflect the poor bone quality and the lack of coverage of the acetabular component due to altered osseous anatomy [22]. The most popular hip prosthesis was metal on polyethylene, followed by ceramic on ceramic. Materials are partly due to surgeon preference; however, patient activity levels, risk of higher impact activity, and dislocating should be considered [31]. Intra-operative femoral fracture requiring cerclage wire fixation occurred in 4/20 hip arthroplasty cases. This rate is higher than the reported mean in the literature of 0.23% in cemented arthroplasty and 3.0% in uncemented implants [32]. Given the morphological changes in MPS patients, difficulty in implant placement can be compounded by lower bone mineral density, particularly in MPS types III and IV [33, 34]. For other MPS types, bone mineral density scans are usually within the normal range when corrected for short stature [35]. Considering bone stock and appropriate implants (standard vs. custom-made) may help prevent intra-operative fractures [20, 24].
Postoperative complications were rarely reported in this patient group, with one patient requiring soft-tissue release for stiffness post-knee arthroplasty and one case of hip arthroplasty loosening requiring revision [16, 19]. Longer-term follow-up is required to determine arthroplasty revision rates and complications in this patient group. There is a lack of literature regarding function and quality of life pre- and post-orthopaedic interventions in MPS patients [26]. HHS, WOMAC, IKS, and OKS scores were reported pre- and post-operatively for only four patients [15, 16, 24]. Pleasingly, these scores and pain scores were reliably improved with surgery in MPS patients.
Arthroplasty surgeons should be aware that less-rapidly progressive or attenuated forms of MPS can present for the first time in early adulthood and are commonly misdiagnosed or have a delayed diagnosis [25, 36]. Joint stiffness without signs of joint inflammation, carpal tunnel syndrome, and hip dysplasia are common presentations of less-rapidly progressive MPS subtypes in early adulthood [25].
Although not the focus of this paper, it is important to consider that the management of MPS, including systemic and orthopaedic management in childhood, is evolving. Acetabular and femoral osteotomies improve radiological parameters for patients with MPS in the short to medium-term [16] but have failed to prevent the development of clinically significant osteoarthritis in adulthood [37]. The benefits of achieving improved anterior and superior hip coverage with osteotomy [16] must be weighed against literature that reports that patients who have undergone prior osteotomies show lower activity scores and higher revision rates post-hip arthroplasty [38]. Guided growth for progressive, pathological genu-valgum in children is a relatively low-risk procedure increasingly used in MPS, particularly in MPS IV [30, 39]. Its role in minimising the development of knee osteoarthritis in these patients is yet to be established.
CONCLUSION
The findings of this review are that knee and hip arthroplasty can be performed safely in patients with MPS but with a higher complication rate than in the non-MPS population. Careful pre-operative planning and multidisciplinary management, including an experienced anaesthetist and awareness of the potential for underlying atlantoaxial instability, are required. Surgeons should be encouraged to share their experiences, including reporting functional and quality-of-life outcomes and longer-term follow-up to help facilitate decision-making and surgical planning in patients with this rare and complex disease.
Authors’ Contributions: Kimon Toumazos was involved in data collection and manuscript production. Both Nicole Williams and Kimon Toumazos were involved in data analysis/interpretation.
LIST OF ABBREVIATIONS
| MPS | = Mucopolysaccharidosis |
| GAG | = Glycosaminoglycan |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| LPS | = Lipopolysaccharide |
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank BioMarin Pharmaceutical Inc. for assistance with the literature search.
SUPPLEMENTARY MATERIAL
The PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
REFERENCES
| [1] | Mucopolysaccharidoses. Phenotypic Series - PS607014 Online Mendelian Inheritance in Man Available from: https://omim.org/phenotypicSeries/PS607014 (Accessed on: 16-4-22). |
| [2] | Fecarotta S, Tarallo A, Damiano C, Minopoli N, Parenti G. Pathogenesis of Mucopolysaccharidoses, an Update. Int J Mol Sci 2020; 21(7): 2515. |
| [3] | Zhou J, Lin J, Leung WT, Wang L. A basic understanding of mucopolysaccharidosis: Incidence, clinical features, diagnosis, and management. Intractable Rare Dis Res 2020; 9(1): 1. |
| [4] | Aldenhoven M, Sakkers RJB, Boelens J, de Koning TJ, Wulffraat NM. Musculoskeletal manifestations of lysosomal storage disorders. Ann Rheum Dis 2009; 68(11): 1659-65. |
| [5] | Simonaro CM, D’Angelo M, He X, et al. Mechanism of glycosaminoglycan-mediated bone and joint disease: implications for the mucopolysaccharidoses and other connective tissue diseases. Am J Pathol 2008; 172(1): 112-22. |
| [6] | Stapleton M, Hoshina H, Sawamoto K, et al. Critical review of current MPS guidelines and management. Mol Genet Metab 2019; 126(3): 238-45. |
| [7] | Dhawale AA, Thacker MM, Belthur MV, Rogers K, Bober MB, Mackenzie WG. The lower extremity in Morquio syndrome. J Pediatr Orthop 2012; 32(5): 534-40. |
| [8] | White KK. Orthopaedic aspects of mucopolysaccharidoses. Rheumatology (Oxford) 2011; 50(Suppl. 5): v26-33. |
| [9] | Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. |
| [10] | Abstracts of the 22nd European Congress of pathology. September 4-9, 2009. Florence, Italy. Virchows Arch 2009; 455(Suppl 1): S1-S448. |
| [11] | Barry MO, Beardslee MA, Braverman AC. Morquio’s syndrome: severe aortic regurgitation and late pulmonary autograft failure. J Heart Valve Dis 2006; 15(6): 839-42. |
| [12] | Blude EA, Reiff DB. De La Caffinière replacement arthroplasty in Morquio-Brailsford disease. Radiogr Today 1990; 56(642): 14-7. |
| [13] | Stewart F, Simon J, Karen T, heather . An attenuated form of Morquio disease in Northern Ireland. Mol Genet Metab 2013; 108(2): S88. |
| [14] | Raggio CL, Yonko EA, Khan SI, et al. Joint replacements in individuals with skeletal dysplasias: one institution’s experience and response to operative complications. J Arthroplasty 2020; 35(8): 1993-2001. |
| [15] | Atinga M, Hamer AJ. Total knee replacements in a patient with the Morquio syndrome. J Bone Joint Surg Br 2008; 90-B(12): 1631-3. |
| [16] | de Waal Malefijt MC, van Kampen A, van Gemund JJ. Total knee arthroplasty in patients with inherited dwarfism - a report of five knee replacements in two patients with Morquio’s disease type A and one with spondylo-epiphyseal dysplasia. Arch Orthop Trauma Surg 2000; 120(3-4): 179-82. |
| [17] | O’hEireamhoin S, Bayer T, Mulhall KJ. Total hip arthroplasty in mucopolysaccharidosis type IH. Case Rep Orthop 2011; 2011: 1-2. |
| [18] | Gautam D, Malhotra R. Total hip arthroplasty in Hurler syndrome – 8 years follow up – A case report with review of literature. J Orthop 2018; 15(1): 111-3. |
| [19] | Guffon N, Froissart R, Fouilhoux A. A rare late progression form of Sly syndrome mucopolysaccharidosis. JIMD Rep 2019; 49(1): 1-6. |
| [20] | Ilyas I, Kashif S, Rabbani S, Alrumaih HA. Simultaneous bilateral total hip arthroplasty in Morquio syndrome. Arthroplast Today 2017; 3(3): 144-6. |
| [21] | Leonard M, Nicholson P. Bilateral uncemented ceramic-on-ceramic total hip arthroplasty in a 26-year-old man with Morquio syndrome. Am J Orthop 2011; 40(11): E229-31. |
| [22] | Pietri M, Sorriaux G, Valle AG, Salvati EA. Total hip replacement in identical twins with Scheie Mucopolysaccharidosis. Hip Int 2005; 15(1): 55-8. |
| [23] | Lewis JRP, Gibson PH. Bilateral hip replacement in three patients with lysosomal storage disease: Mucopolysaccharidosis type IV and Mucolipidosis type III. J Bone Joint Surg Br 2010; 92-B(2): 289-92. |
| [24] | Tassinari E, Boriani L, Traina F, Dallari D, Toni A, Giunti A. Bilateral total hip arthroplasty in Morquio-Brailsford’s Syndrome: a report of two cases. Chir Organi Mov 2008; 92(2): 123-6. |
| [25] | Vijay S, Ed Wraith J. Clinical presentation and follow-up of patients with the attenuated phenotype of mucopolysaccharidosis type I. Acta Paediatr 2005; 94(7): 872-7. |
| [26] | Williams N, Challoumas D, Eastwood DM. Does orthopaedic surgery improve quality of life and function in patients with mucopolysaccharidoses? J Child Orthop 2017; 11(4): 289-97. |
| [27] | Moretto A, Bosatra MG, Marchesini L, Tesoro S. Anesthesiological risks in mucopolysaccharidoses. Ital J Pediatr 2018; 44(S2)(Suppl. 2): 116. |
| [28] | Williams N, Cundy PJ, Eastwod DM. Surgical management of thoracolumbar kyphosis in patients with mucopolysaccharidosis. Spine 2017; 42(23): 1817-25. |
| [29] | Georgiadis AG, Koester TM, Mackenzie WG, et al. Intraoperative neurological monitoring in lower limb surgery for patients with mucopolysaccharidoses. J Pediatr Orthop 2021; 41(3): 182-9. |
| [30] | Ashby E, Eastwood D. Characterization of knee alignment in children with mucopolysaccharidosis types I and II and outcome of treatment with guided growth. J Child Orthop 2015; 9(3): 227-33. |
| [31] | Merola M, Affatato S. Materials for hip prostheses: A review of wear and loading considerations. Materials (Basel) 2019; 12(3): 495. |
| [32] | Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties. Bone Joint J 2016; 98-B(4): 461-7. |
| [33] | Nur BG, Nur H, Mihci E. Bone mineral density in patients with mucopolysaccharidosis type III. J Bone Miner Metab 2017; 35(3): 338-43. |
| [34] | Kubaski F, Kecskemethy HH, Harcke HT, Tomatsu S. Bone mineral density in mucopolysaccharidosis IVB. Mol Genet Metab Rep 2016; 8: 80-4. |
| [35] | Fung EB, Johnson JA, Madden J, Kim T, Harmatz P. Bone density assessment in patients with mucopolysaccharidosis: A preliminary report from patients with MPS II and VI. J Pediatr Rehabil Med 2010; 3(1): 13-23. |
| [36] | Williams N, Challoumas D, Ketteridge D, Cundy PJ, Eastwood DM. The mucopolysaccharidoses. Bone Joint J 2017; 99-B(9): 1132-9. |
| [37] | Kennedy J, Noel J, O’Meara A, et al. A long-term retrospective evaluation of functional and radiographic outcomes of pediatric hip surgery in hurler syndrome. J Pediatr Orthop 2016; 36(1): 25-8. |
| [38] | Amstutz HC, Le Duff MJ. Effects of previous osteotomy on outcome of hip resurfacing arthroplasty. Orthopedics 2017; 40(4): e609-16. |
| [39] | Cooper GA, Southorn T, Eastwood DM, Bache CE. Lower extremity deformity management in MPS IVA, morquio-brailsford syndrome: Preliminary report of hemiepiphysiodesis correction of genu valgum. J Pediatr Orthop 2016; 36(4): 376-81. |








