All published articles of this journal are available on ScienceDirect.
Total Knee Arthroplasty Conversion after Open-wedge High Tibial Osteotomy
Abstract
Background:
Open-wedge High Tibial Osteotomy (HTO) is an effective treatment for Osteoarthritis (OA) of the knee; however, postoperative changes due to HTO can make subsequent Total Knee Arthroplasty (TKA) technically difficult and can affect long-term survival.
Case Report:
Medio-lateral stability along with balanced flexion and extension gaps provides a good functional outcome.
A 71-year-old man underwent TKA conversion after open-wedge HTO 12 years earlier; the conversion was performed due to arthritic deterioration in the knee. Medial instability was noted because of poor ligament balancing. The residual medial instability was managed with a knee brace due to the unavailability of the constrained prosthesis. Management of persistent mediolateral instability persisting after soft tissue release and balancing ideally requires varus-valgus constraint.
Conclusion:
TKA conversion after open-wedge HTO requires a special technique and careful preparation before surgery.
1. INTRODUCTION
Surgical treatment options for Osteoarthritis (OA) of the knee are High Tibial Osteotomy (HTO), unicomponental knee arthroplasty, and Total Knee Arthroplasty (TKA). Two options of HTO for the treatment of medial compartment knee OA are closed-wedge HTO and open-wedge HTO. Open-wedge HTO has become increasingly employed as an alternative to closed-wedge osteotomy. In relatively young patients who are very physically active and have significant symptoms of medial compartment knee OA, HTO may delay the indication for TKA [1, 2], but postoperative changes due to HTO can make subsequent TKA technically difficult and affect the long-term survival. Lateral deviation of the tibial articular surface due to HTO can make intraoperative deployment and placement of the ideal component difficult, and special treatment may be required. Medial instability during the TKA procedure is also problematic. We present a case of TKA after open-wedge HTO with residual imbalance during the operation that gradually improved.
2. CASE
A 71-year-old man underwent open-wedge HTO for OA of the right knee 12 years previously. He had no symptoms in his right knee after HTO for 9 years. However, he developed progressive pain in both knees. He underwent TKA of the left knee one year later. After the left TKA, his right knee pain worsened. Therefore, he was referred to our department for surgery. His medical history, and that of his family, was unremarkable.
Physical examination revealed swelling, effusion, and medial joint line tenderness in the right knee. The Range of Motion (ROM) was between 5° and 120°. McMurray tests for the medial meniscus were negative. There was no varus-valgus instability. The knee score of the Hospital for Special Surgery (HSS) was 72. Weight-bearing radiography demonstrated a Kellgren-Lawrence OA grade of 3 (Fig. 1). The anatomical lateral distal femorotibial angle was 166°.
Right TKA was performed using a balance knee system Trimax PS type and stem extension of 3 cm (Japan Medical Dynamic Marketing, INC., Tokyo, Japan) with cement. The bone defect was not seen in the baseplate contact area of the tibia, but the artificial bone used during HTO remained without being replaced by the bone in the proximal medial tibia. Therefore, considering reducing the shearing force, a stem extension was used. The Medial Collateral Ligament (MCL) was detached from the tibia under the periosteum. Valgus release was performed as much as possible to the extent that posterolateral instability would not develop. Scarring and fibrosis of the medial soft tissue sleeve compromised the medial release assessment. The mediolateral balance was poor and medial instability was noted.
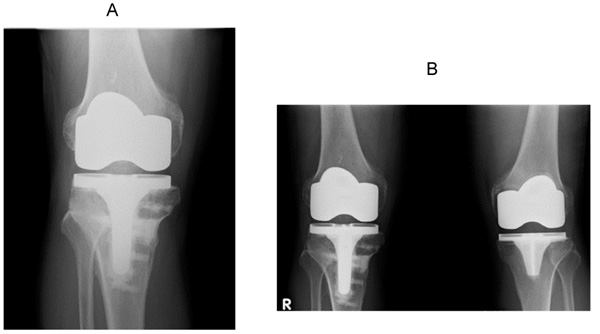
The residual medial instability was managed with a knee brace due to the unavailability of the constrained prosthesis. After the operation, a plaster slab was placed on the right leg for 1 week (Fig. 2). Range of Motion (ROM) exercises were initiated 1 week after the surgery with a knee brace. Full weight-bearing was allowed at 6 weeks postsurgery. The knee brace was placed on the right knee for 3 months (Fig. 3). The medio-lateral balance gradually improved. He had mild pain in his right knee joint 1 year and 9 months after right TKA, and the ROM was from 5 to 110°. The HSS score was 85 points (Fig. 4). Almost no medial instability was noted during the clinical examination. The mediolateral balance gradually improved.
3. DISCUSSION
HTO is one of the established treatments for knee OA and is performed worldwide. In relatively young, active patients who require pain relief and functional improvement, HTO may be satisfactory and may delay the indication for TKA. Amendola reported that the ideal indication for HTO is a young patient (<60 y of age) with isolated medial OA, a good ROM, and no ligamentous instability [2]. Billings reported that two-thirds of the knees in their series had a good or excellent clinical result after a postsurgical average of 8.5 years [1-4]. Niinimäki reported an overall survival of 89% at 5 years and 73% at 10 years, using the Kaplan-Meier analysis. Hui reported that the probability of survival after HTO at 5, 10, and 15 years was 95%, 79%, and 56%, respectively. Arthritic deterioration in knees with HTO may progress during longer follow-up and lead to TKA. After HTO, the knee may develop lateral deviation of the tibial articular surface to the tibial axis and changes in soft tissue balance due to rotational deformity, causing problems during TKA, such as increased osteotomy of the medial tibial cheek, poor ligament balance due to PCL shortening, and imbalance of internal and external soft tissues [5, 6]. TKA conversion after HTO was reported to not differ clinically from TKA performed without prior HTO [7-9]. Noda reported that the clinical results of TKA after HTO are slightly inferior to those of primary TKA, likely because of technical problems [10]. Efe reported significant differences between TKA with and without prior HTO only in the ROM and knee score of the HSS [11]. Radiographically, the HTO-TKA group had more loosening and impingement of the tibial component [12]. Soft tissue problems, difficulty with patella eversion, management of retained hardware, handling of coronal and sagittal plane deformities of the proximal tibia, and difficulties in ligament balancing have been emphasized during TKA conversion after HTO. In this case, ligament balancing was an important and difficult problem.
The weight-bearing radiogram showed a Kellgren-Lawrence OA grade of 3. The anatomical lateral distal femoro-tibial angle was 166°.
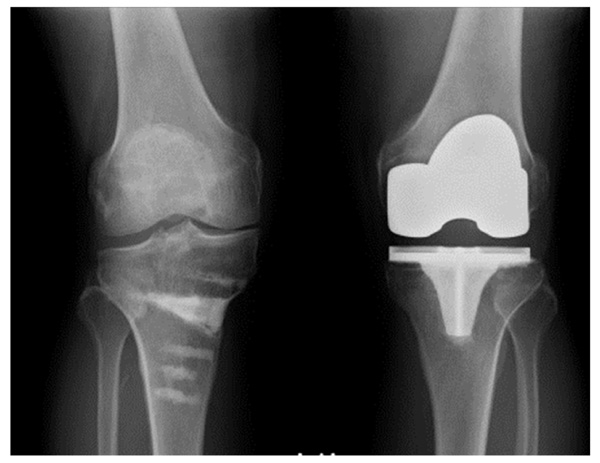

A-P view.

A-P view.
Joint instability after TKA can be caused by numerous risk factors such as inappropriate osteotomy, insert placement, insert selection for the joint gap, and soft tissue imbalance. Vince reported that the possible modes of tibiofemoral instability after TKA could be classified into four patterns: varus-valgus, recurvatum, flexion, and global instability [13]. The type, in this case, was varus-valgus instability; in particular, medial instability. There are several options for surgical treatment of medial instability during TKA surgery: MCL attachment transfer, MCL reconstruction, and constrained TKA [14]. The prostheses used for collateral ligament failure are the constrained type and semi-constrained type. These implants are indicated in cases of collateral ligament deficiency or excessive instability requiring reconstruction. Vince reported that the common surgical solution for a constrained implant to substitute for collateral ligament deficiency might fail if the deforming forces are not eliminated or reduced [13]. In this case, conservative treatment was provided for medial instability during TKA surgery due to lack of preparation of another prosthesis. If medial instability had persisted after surgery, we would have considered revision TKA using the constrained type. However, the conservative treatment was effective. The instability of the medial support mechanism, which became like a rope and lacked flexibility, might have been corrected by wearing the brace and performing ROM training. However, TKA conversion after open-wedge HTO requires a special technique and careful preparation before surgery.
CONCLUSION
We performed TKA conversion on a patient who underwent open-wedge HTO 12 years earlier. The medial instability during TKA caused by ligament balancing was problematic. Conservative treatment using a knee brace was performed, and the medial instability improved gradually. However, careful preparation before surgery is required for such cases.
LIST OF ABBREVIATIONS
| OA | = Osteoarthritis |
| TKA | = Total Knee Arthroplasty |
| HTO | = High Tibial Osteotomy |
| HSS | = Knee-rating Scale of Hospital for Special Surgery |
| FTA | = Femoro-Tibial Angle |
| ROM | = Range of Motion |
| MCL | = Medial Collateral Ligament |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
We have obtained consent to publish from the patient.
STANDARDS OF REPORTING
CARE guidelines have been used for conducting this study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
ACKNOWLEDGEMENTS
Declared none.


