All published articles of this journal are available on ScienceDirect.
The Hip in Juvenile Idiopathic Arthritis
Abstract
The hip joint is commonly affected in Juvenile Idiopathic Arthritis (JIA), especially in cases of systemic polyarticular disease. Chronic synovitis of the hip leads to joint destruction, therefore, systemic and local control of the disease is of paramount importance. Non-steroidal anti-inflammatory drugs, Disease Modifying Anti-Rheumatic Drugs (DMARDs), biologics, intra-articular corticosteroid injections, and physical therapy are the mainstay for controlling ongoing inflammation and hip joint contractures. Synovectomy with soft tissue releases is useful in the early stages of the disease, when the joint cartilage is largely preserved. Total joint arthroplasty (THA) is successful in relieving pain, and improving function, ambulation and range of motion in end-stage degenerative arthritis. With improved designs of smaller prostheses and modern bearing couples, it is hoped that the longevity of THA will facilitate a more normal and enduring lifestyle.
1. INTRODUCTION
Juvenile Idiopathic Arthritis (JIA) is the most common rheumatologic disease in children less than 16 years of age and has an incidence of approximately 16-150 cases per 100,000 children worldwide [1, 2]. The hip joint is commonly affected in JIA; in approximately 20-40% of JIA patients, the hip joint will be afflicted by chronic synovitis that leads to pain and stiffness due to ongoing inflammation and progressive joint destruction [2, 3]. Two years after the diagnosis of systemic JIA is made, clinical hip involvement can be expected in about 50% of patients [2]. These events lead to disuse atrophy and regional osteoporosis, contractures and difficulties with ambulation and function. In younger patients usually below the age of 9, local inflammation of the hip joint stimulates growth, resulting in a coxa magna, as well as a very elongated femoral neck with excessive anteversion (“pseudovalgus”) [3]. When the disease is initiated or worsens after approximately age 9 when much growth has been completed, the growth plate of the capital epiphysis may close prematurely, leading to coxa magna but shortening and varus alignment of the femoral neck and overgrowth of the trochanteric apophysis. The proximal femur and acetabulum develop together after birth; altered femoral growth at an early age due to chronic inflammation will subsequently modify the growth and anatomic configuration of the acetabulum [4]. Consequently, in JIA, the acetabulum is frequently dysplastic, shallow in the coronal (frontal) plane, but may be large if there is coxa magna. The femoral head is often partially uncovered, subluxated or even dislocated. Interestingly, in the sagittal plane, the acetabulum is often disproportionately large. With the progression of the disease, the hip joint demonstrates radiographic evidence of increasing loss of joint space, cyst formation, proximal migration (with loss of bone stock) and subluxation. This radiographic progression is associated with more local pain and stiffness, shortening of the limb, contractures and decreased ambulation capacity. Thus, it is important to make the diagnosis of JIA expeditiously so that appropriate treatment can be instituted prior to joint destruction. Earlier assessment of the degree of inflammation of the hip joint can be aided by Magnetic Resonance Imaging (MRI) and ultrasound [5].
2. NON-OPERATIVE MANAGEMENT
Treatment of JIA necessitates a multi-disciplinary approach, as discussed elsewhere in this journal issue [1]. Specifically, for the hip, chronic inflammation leading to pain, contractures and reduced ambulatory capacity must be controlled with appropriate medication, physical therapy and counselling. For the treatment of inflammation of the hip joint, judicious use of non-steroidal anti-inflammatory drugs (NSAIDs), disease modifying anti-rheumatic drugs (DMARDs), and other biologic therapies, pain medication and physical therapy to maintain joint motion, strength and gait are essential elements. Occasional intra-articular corticosteroid injections into the hip joint will provide relief of pain and mitigate synovitis. These may be given up to approximately three times per year [1]. Despite the above, continued arthritis of the hip joint necessitates surgical intervention. A recent study has shown that JIA patients treated medically after the year 2000 with newer biologic therapies had less disability than previously; in fact, 25% of the patients were in remission. Furthermore, only 5% of patients in this cohort had articular joint damage [6]. A recent systematic review reported that despite overall improvements in technology and patient care, total hip arthroplasty (THA) is being performed less frequently in patients with JIA than previously [7].
3. SURGICAL TREATMENT OF THE HIP: JOINT PRESERVATION
Several joint preserving operations are available for the treatment of early JIA of the hip, when medical treatment fails to control ongoing pain and inflammation.
Arthroscopic procedures of the JIA hip can be performed using the supine position and a traction table for distraction [8]. Intra-articular pressures were found to be elevated in JIA due to chronic synovitis [9]. This operation allows assessment of the joint surfaces, irrigation of the inflammatory joint fluid, and limited synovectomy and capsulotomy. This diagnostic and therapeutic procedure is best used in the early stages of the disease and combined with physical therapy.
Open synovectomy of the hip is a safe and reliable procedure, which may be combined with the release of contractures of soft tissues, including tenotomy and capsulotomy/capsulectomy [3, 10-12]. In one recent study, the survivorship of the hip at 4 years after synovectomy was 94%, with significant improvement in scores for pain, mobility and walking ability [10]. The surgery is usually performed through an anterior iliofemoral surgical approach (Smith Peterson approach). If the synovium is excessively hypertrophic and not accessible, the hip is dislocated. The ligamentum teres is resected. In the series referenced above, cysts were curetted and debrided. The labrum was left intact. Extremes of hip positioning during dislocation were avoided. If a residual hip flexion contracture measured greater than 20°, the rectus femoris and iliopsoas tendons were released or lengthened. The patient was mobilized full weight bearing immediately and began a structured exercise program.
4. SURGICAL TREATMENT OF THE HIP: ARTHROPLASTY
Arthroplasty of the hip is indicated in patients with JIA when the pain and disability from advanced degenerative arthritis cannot be managed successfully with conservative management. Although hemiarthroplasty and resurfacing procedures have been attempted in the past, they have generally been abandoned because of inadequate relief of pain, poor bone stock, and continued protrusion with loss of bone stock in the case of hemiarthroplasty or hemi-resurfacing.
Total hip arthroplasty (THA) is challenging because of the small anatomic proportions and excessive anteversion of the femur and acetabulum, poor bone stock, generalized under-development and atrophy of the soft tissues around the hip, and the availability of suitable implants [13]. Originally, cemented hip replacement was used for reconstruction [14-23]. However, some of these series have shown relatively high complication and failure rates, especially of the acetabular component due to aseptic loosening and wear. Two large series from specialized centers using Charney implants have reported excellent long-term results. Wroblewski’s series of cemented Charnley THAs in rheumatoid patients less than 50 (some of whom had JIA) reported survivorship of 93% at 10 years, 87% at 15 years, 81% at 20 years and 74% at 25 years [23]. The overall revision rate was 14%. In a Finnish series of patients with juvenile chronic arthritis undergoing Charnley THA, the overall implant survivorship was 91.9% at 10 years, and 83% at 15 years. Survivorship of the acetabular component was 87.8% and that of the femoral component was 87.7% at 15 years. The ongoing use of corticosteroids reduced the longevity of the implant significantly, with an associated hazard ratio of 2.64. Given these excellent long-term results using the Charnley cemented THA in specialized centers, one must conclude that this construct is the gold standard with which newer implants must be compared.
Many of the series reporting the outcome of THA in younger patients, group several diagnoses together, so it is often difficult to separate out the patients with JIA from other diagnoses such as hip dysplasia, Perthes disease, post-traumatic arthritis, etc. One recent study reported a revision rate of 25% after 5-24 years in a cohort of 118 THAs in patients less than 30 years of age. Twenty-five percent of the cohort had JIA [24]. In a series of 108 revision THA in patients less than 35 years of age who were comprised of multiple different diagnoses including JIA, acetabular loosening occurred in 30.1%, femoral loosening in 23.7% and polyethylene wear was found in 24.7% after a mean of 10.1 years [25]. In the above 2 series, the majority of patients had conventional polyethylene as a bearing surface. Newer bearing surfaces such as ceramic or metal on highly cross-linked polyethylene and ceramic-on-ceramic have shown improved survivorship in younger patients [26, 27].
More recently, cementless implants are being used more frequently in younger patients. This reconstructive approach can be more difficult than cemented arthroplasty, especially on the femoral side, where a firm press fit must be obtained for initial stability and long-term fixation, despite challenging anatomical abnormalities and poor bone stock. Nevertheless, several reports have been published using cementless implants with good success. When reviewing these series, one must be cognizant of the fact that those with longer follow-up generally use non-cross-linked polyethylene. In these series, the acetabular component is small, and therefore the polyethylene liners are thin, pliable and wear at a higher rate compared with highly cross-linked polyethylene in current use.
An early series of 25 cementless THAs (both off-the-shelf and custom made) in 16 JIA patients reported a 10% acetabular loosening rate after 4.5 years [28]. In a series of 47 hips in 25 patients in which both cementless and cemented components were used, there were few differences in survivorship up to 19 years post-operatively [29]. Cemented sockets and cementless stems tended to have slightly increased longevity, but the results were not statistically significant. Implant survivorship at 19 years was 54.9%. In a series of 20 hips comprising both 10 cemented and 10 cementless femoral implants and cementless sockets, at 2-20 year (average 9.2 years) post-operatively, there were bilateral cup revisions in one patient only [30]. Other early smaller series with mixed cemented and cementless implants have also been reported [31]. Odent et al. reported a series of 62 cementless Zweymuller THAs (including a threaded acetabular component with a 28 mm inner diameter) in 34 patients with a mean follow-up of 6 years (range 3-13 years) [32]. Three cases had a metal-on-polyethylene bearing couple; in 21, the bearing was alumina-on-polyethylene and in 38, it was metal-on-metal. At 13 years, the survivorship was 100% for the femoral component and 90.1% (2 failures) for the acetabular component. Daurka et al. reported the mid-term results of 52 cementless THA in JIA at a median of 10.5 years (range 6-15 years). Thirteen of the 52 hips underwent revision. All 23 of the ceramic-on-ceramic bearing THA survived, however only 16 of 29 (55%) of the metal-or ceramic-on (conventional non-cross-linked) -polyethylene hips survived. Wear and osteolysis lead to acetabular component revision in 11 of 13 cases. Thirty-one cementless hydroxyapatite (HA)-coated alumina-on alumina THAs were followed for 60–108 months [33]. One cup was revised at 17 months for loosening. Figgie’s group performed a retrospective study of 56 JIA patients with 97 primary THAs (41 bilateral, 15 unilateral) with a mean of 12 years of follow-up. Thirty percent of the implants were custom components [34]. Eighty-seven percent of acetabular components and 62% of the femoral components were cementless. The survivorship was 96% at 5 years, 84% at 10 years, 62% at 15 years and 50% at 20 years. Age over 25 years at surgery was associated with improved survivorship.
Although not commonly performed, one stage bilateral THAs have been reported in JIA patients. Although the series are small and often confounded by diagnoses other than JIA, one stage bilateral THA, at least in the short term, appears to be another treatment option [35].
What is the complication rate after THA in JIA? When examining the peri-operative complication rate in patients with all types of inflammatory arthritis undergoing THA as documented in the US Nationwide Inpatient Sample between 2002 and 2002, a significantly higher overall complication rate was found compared to patients with osteoarthritis [36]. Patients with JIA had increased prevalence of specific complications, including central nervous system complications, hematomas, wound infections, and periprosthetic fractures.
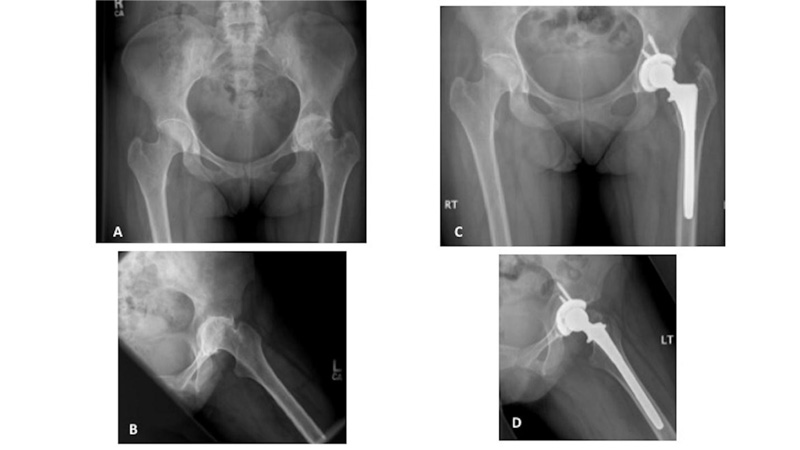
A - Pre-operative anteroposterior (AP) radiograph of the pelvis. Note the protusio due to loss of medial bone stock, the virtual absence of joint space, small osteophytes, and cyst formation of the left hip.
B - Pre-operative frog lateral view of the left hip.
C - Post-operative radiograph showing a cementless cup with screws and a cementless proximally porous coated stem.
D - Post-operative frog lateral view of the left hip.
The prosthesis used by the author, in this case, was one of the earliest cementless implants available for small proportioned patients. This prosthesis is no longer available.
Our experience with THA in JIA patients encompasses over 25 years using primarily cementless components [13, 37-41] (Figs. 1 and 2). A direct lateral approach was used for exposure, performing an anterior capsulectomy and dislocating the hip anteriorly. This approach was chosen due to the excessive anteversion in the femur and acetabulum, facilitating easy visualization of the hip and dislocation without force. Furthermore, as opposed to the posterior approach, the limb is placed over the side of the operating table with the knee bent to 90° (if possible) without undo torsion that could potentially lead to femoral fracture. After the femoral neck is cut, the femoral component is prepared for cementless fixation. If the bone stock was very poor, early in the series, cemented stems were used. Unfortunately, due to the small size of the components, modern cement technique with the centralization of the stem could not be used, often leading to thin cement mantles. Cementless cups were used in almost all cases. Rarely, if the acetabulum was severely dysplastic, a roof ring and cemented cup were used. Our initial experience reported in 1998, with a follow-up of 2-8 years (mean = 4.5 years), was satisfactory; in 29 cases, only 1 femoral component needed revision for loosening [38]. Pain relief, function and range of motion improved significantly. However, with a longer follow-up of up to 20 years, 37 cases were reviewed, and demonstrated a higher failure rate [37]. Failures were generally due to conventional polyethylene wear and osteolysis (Fig. 3); all 3 standard cementless implants with minimal porous coating just at the collar area (Osteocap, Biomet) failed to osseointegrate, loosened and migrated. Three other femoral components (1 cemented and 2 cementless) loosened up to almost 20 years later, due to osteolysis. At the final follow-up of almost 20 years, 12 of 37 (32.4%) hips required revision. Most of these revisions were straightforward, however, some were very complex because of the severe bone loss associated with osteolysis [40]. Furthermore, the early and late complication rate was substantial, with intra-operative femoral fracture, late infection and mechanical loosening.
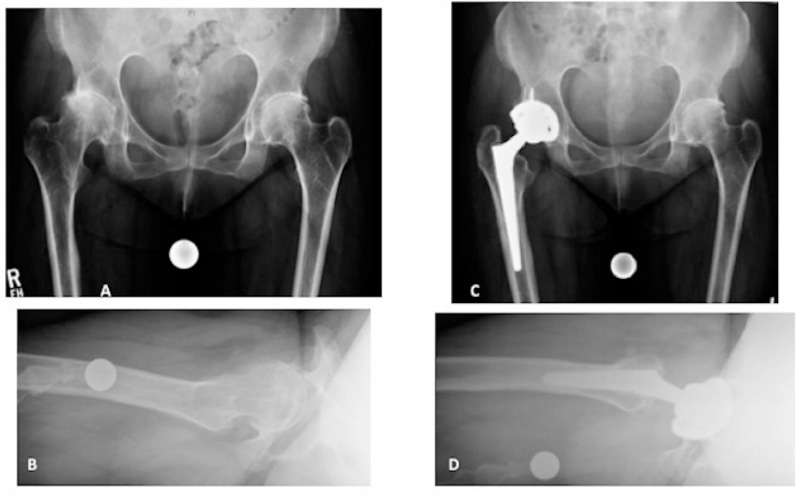
A - Pre-operative AP radiograph of the pelvis. Note the absent joint space, subluxation with dysplasia, and subchondral sclerosis and cyst formation of the right hip.
B - Pre-operative frog lateral view of the left hip
C - Post-operative radiograph showing a cementless cup with screws and a cementless Wagner Cone femoral stem (Zimmer Biomet, Warsaw, IN).
D - Post-operative frog lateral view of the left hip.
The prosthesis used in this case is the preferred one by the author currently.

A - AP radiograph of the pelvis several years after the right THA. The right hip has been replaced with a cemented stem and a cementless cup with screws (hybrid THA). Note the high placement of the socket due to prior dysplasia. The left hip shows advanced arthritis.
B, C, D - Years later, the left hip has been replaced with a hybrid THA. The right hip now shows advanced polyethylene wear and periprosthetic osteolysis.
B- AP radiograph of the pelvis; C- Iliac oblique Judet view; D- Obturator oblique Judet view
Post-operative AP (E) and cross table lateral (F) radiographs of the revised right THA. The entire cup was replaced due to its small size and failed locking mechanism. The femoral head size was increased. The stem was well fixed; the deficient calcar was strut grafted.
After 2003, cross-linked polyethylene has been used, which has dramatically reduced the incidence of polyethylene wear and osteolysis. In addition, for the last 10 years, we have used the cementless Wagner Cone femoral component (Zimmer Biomet, Warsaw, IN) which has numerous small sizes to accommodate the small proportions in JIA, and facilitates placement in appropriate anteversion easily, due to the symmetric proximal femoral portion of the stem (Fig. 2). We recently reported our initial experience with this stem in small statured patients (some of whom with JIA) with excellent results [42].
CONCLUSION
Patients with JIA frequently develop progressive, debilitating arthritis of the hip; this is complicated by small anatomic proportions, excessive femoral and acetabular anteversion, poor bone stock and muscle atrophy. Conservative medical and surgical management is first implemented. THA is a very successful surgical procedure for patients with painful end-stage degenerative arthritis. In the past, lack of appropriate-sized implants and bearing couples compromised implant longevity. Modern implants and bearing surfaces have been associated with good pain relief, improved ambulation, a more normal lifestyle, and (hopefully) increased long-term survivorship.
CONSENT FOR PUBLICATION
All patients participated on a voluntary basis and gave their informed consent.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
No funding was used for the preparation of this publication.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The author is grateful to Katherine Hwang MS, clinical data manager of our orthopaedic database, and to the patients with juvenile arthritis and the numerous medical personnel for the excellent care of these patients.


