All published articles of this journal are available on ScienceDirect.
Ultrasound-guided Arthroscopic Tuberoplasty for Greater Tuberosity Malunion: A Case Report
Abstract
Background:
Greater Tuberosity (GT) malunion can lead to impingement against the acromion, resulting in pain, stiffness, and weakness of the rotator cuff. For patients with lesser degrees of displacement, partial removal of the GT with rotator cuff repair (tuberoplasty) under fluoroscopic guidance is considered.
Case report:
A sixty-five year old female fell from a standing height and suffered a minimally displaced isolated GT fracture. She was conservatively managed for four months and referred to our institution due to persisting pain and stiffness. The shoulder motion was severely restricted (anterior elevation: 90°, lateral elevation: 45°, external rotation with the arm at side: 25°, hand behind back: 4th lumber vertebrae) and pain aggravated especially when laterally elevated. Plain radiography and computed tomography showed small superiorly malunited GT and magnetic resonance imaging showed no rotator cuff pathology. Ultrasound images showed impingement of the GT against the acromion when laterally elevated. Arthroscopic excision of the malunited GT and rotator cuff repair along with capsular release and acromioplasty was performed under ultrasound guidance. The ultrasound images were simultaneously delineated to the arthroscopic monitor. Dynamic evaluation of the reshaped GT passing under the acromion was possible.
Conclusion:
Intraoperative use of ultrasound during arthroscopic tuberoplasty offers advantages over fluoroscopic guidance concerning control of the amount of bone resection and dynamic evaluation between the GT and the acromion in addition to the problems of radiation and space-occupying devices.
1. INTRODUCTION
Isolated fracture of the Greater Tuberosity (GT) accounts for a small percentage of proximal humerus fractures. The degree of displacement is critical to decide if surgical intervention is needed [1, 2]. Minimally displaced GT fractures (less than 5 mm) can generally be treated non-surgically [1, 3, 4]. Open or arthroscopic fixation with screws and washers, locking plate, or heavy sutures are used for cases with more than 5 mm displacement [1]. Because of the small amount of space available between the GT and rotator cuff passing under the coracohumeral arch, some authors suggest that for displacement >3 mm, surgical intervention should be used for young and active patients [5]. Furthermore, the degree of GT displacement should be carefully monitored after the initial evaluation because its degree could easily increase [2].
Shoulder stiffness, malunion, and nonunion are the most common complications after GT fractures, regardless of treatments [1, 6, 7]. Continuous pain and stiffness due to GT malunion are not acceptable; thus, surgical intervention must be considered [4]. Arthroscopic capsular release with acromioplasty is recommended for shoulder stiffness [6, 8]. Mobilization and fixation of the GT fragment is considered when the fragment is sufficiently large for fixation and is severely displaced [9]. In cases of GT malunion with lesser degrees of displacement, partial removal of the tuberosity along with rotator cuff repair (tuberoplasty) can provide satisfactory results [8, 10-12]. However, it is often difficult to determine the accurate amount of bone resection, even with fluoroscopic guidance during surgery [13]. We report a case of GT malunion, for which we used ultrasonography during arthroscopic tuberoplasty. This enabled accurate resection of the malunited GT and dynamic evaluation of the GT passing under the acromion.
2. CASE REPORT
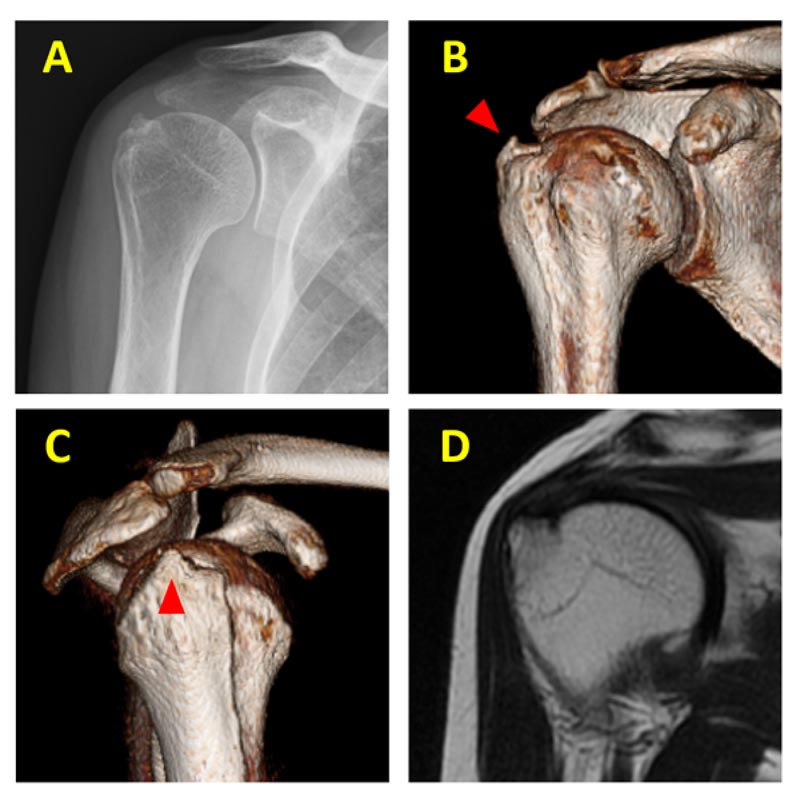
A 64-year-old, right-handed woman suffered a right GT fracture without dislocation of the shoulder after falling from a standing height. She was diagnosed with an isolated GT fracture with minimal displacement. She was treated conservatively with sling immobilization for a week and subsequently recommended passive range of motion exercise at the first clinic visit. She visited our hospital 4 months after the injury with severe pain and stiffness. Active and passive ranges of motion were restricted with 90° forward elevation, 45° lateral elevation, 25° external rotation with the arm on the side, and the 4th lumbar vertebrae at hand behind back. Pain aggravated, especially during lateral elevation. Plain radiography and computed tomography showed a small superiorly migrated and malunited GT fragment (Fig. 1A-C). Magnetic resonance imaging showed an intact rotator cuff (Fig. 1D). Ultrasonography revealed an impingement of the GT to the acromion during lateral elevation (Supplementary video 1). Despite intense rehabilitation and pain control with non-steroidal anti-inflammatory drugs and a few intra-articular and subacromial steroid injections, the symptoms persisted. Therefore, surgical treatment was recommended.
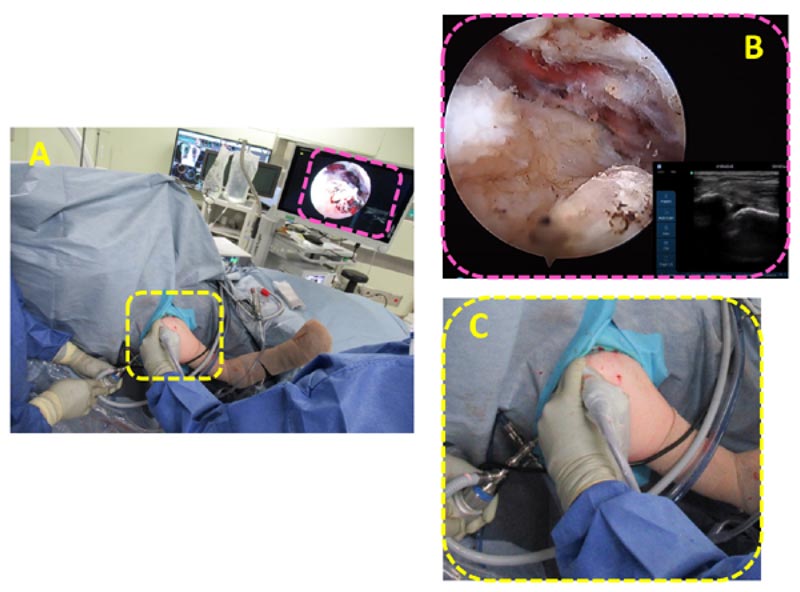
The affected shoulder was examined with the patient under general anesthesia in a beach-chair position. Severe stiffness was observed. Standard posterior and anterior portals were created, and the glenohumeral joint was viewed via a diagnostic arthroscopy. The rotator interval was covered with thick dense fibrous tissues accompanying synovitis, and the joint capsule became thick and stiff with the development of abnormal blood vessels. Resection of the thickened rotator interval, including the coracohumeral ligament, followed by the entire capsular release, was performed [14]. The arthroscope was then removed from the glenohumeral joint and introduced into the subacromial space. A lateral portal was created, and the subacromial bursae were resected to clearly view the entire GT and the malunited fragment. An ultrasonography (Sonosite S-series; Fujifilm Corp., Tokyo, Japan) was then performed, and the ultrasound images were simultaneously delineated to the arthroscopic monitor (Fig. 2). The transducer and its cable were covered with a sterilized bag and introduced from the lateral aspect of the shoulder. The rotator cuff was carefully detached from the malunited fragment with a radiofrequency device (VAPR Angled Side Effect; DePuy Mitek, Raynham, MA), and the bone prominence was resected with an acromionizer (Dyonics Incisor Plus Platinum; Smith & Nephew, Boston, MA) under ultrasonographic guidance (Supplementary video 2). The impingement of the GT against the acromion was improved. Finally, the detached rotator cuff was repaired with an anchor (Q-FIX 2.8 mm; Smith & Nephew) and two simple sutures.
Postoperatively, the shoulder was placed in a sling for 3 weeks, and passive range of motion exercises was initiated the day after surgery. Active range of motion exercises was allowed after removal of the sling. A year after the surgery, she had regained full range of motion of the shoulder and could use her shoulder without experiencing pain during daily activities. The American Shoulder and Elbow Surgeons scores improved from 30 points preoperatively to 95 points at one year after the surgery.
3. DISCUSSION
We successfully managed a case of superiorly migrated GT malunion with a treatment approach that consisted of (1) capsular release and lysis of adhesions around the coracoacromial ligament; (2) subacromial decompression and treatment of associated pathology when needed; and (3) tuberoplasty and rotator cuff repair under ultrasonographic guidance. The treatment method of GT malunions is determined by the size of the bone fragment and the direction of displacement [4]. When the GT fragment is small and superiorly displaced, arthroscopic excision of the malunited bone prominence and rotator cuff repair (tuberoplasty) could be considered.
Mutch et al. proposed a morphologic classification of isolated GT fractures into three types: avulsion, split, and depression [15]. Avulsion-type fractures can be treated similar to rotator cuff repair because of the small bone fragment, and the best candidate for arthroscopic tuberoplasty when a GT fragment is malunited and symptomatic. Tuberoplasty needs detachment of the rotator cuff from the GT followed by resection of the malunited bony prominence. The rotator cuff is reattached to the GT, and an acromioplasty may be performed to maintain the subacromial space. A few small case series have reported the usefulness of arthroscopic tuberoplasty for GT malunions [8, 10-12]. However, in some cases, it is difficult to determine the extent of the bone resection even with an image intensifier.
Diagnostic ultrasonography of the shoulder can identify abnormalities in the rotator cuff, biceps tendon, glenohumeral and acromioclavicular joints, as well as in other soft tissue structures [16]. Ultrasonography is also increasingly used for the facilitation of minimally invasive procedures such as subacromial or glenohumeral injections and needle aspiration of the calcified tissues in the rotator cuff [17]. However, there are few reports of intraoperative use of ultrasonography during shoulder surgery [18, 19]. Boehm et al. described 10 cases of acromioclavicular disorders treated with arthroscopic lateral clavicle resection. They reported that intraoperative use of ultrasound allowed a precise amount of bone resection [18]. Hashiuchi et al. reported a case of ultrasound-guided arthroscopic decompression of a supraspinous fossa cyst [19]. In this study, we reported the usefulness of the intraoperative use of ultrasonography during arthroscopic tuberoplasty for GT malunion, which allowed monitoring of the amount of bone resection and dynamic evaluation between the acromion and the GT without fluoroscopic guidance.
CONCLUSION
Intraoperative ultrasonographic monitoring during arthroscopic tuberoplasty is a useful method to detect small bone fragments as well as control the amount of bone resection. Furthermore, it can easily detect dynamic motion of the shoulder components during arthroscopic surgery without any exposure to radiation.
ABBREVIATION
| GT | = Greater Tuberosity |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study is approved by the ethic committee of Tohoku University Graduate School of Medicine Japan with the approval of NO. 2020-1-577.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
All patients participated on a voluntary basis and gave their informed consent.
STANDARDS OF REPORTING
CARE guidelines have been used for this study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publisher’s website along with the published article.


