All published articles of this journal are available on ScienceDirect.
Early to Mid-Term Results in Trapezio-metacarpal Joint Replacement using the ARPE Implant
Abstract
Background:
Trapezio-Metacarpal Joint (TMJ) arthritis is a common cause of radial sided wrist pain. After conservative measures have been exhausted, the current mainstay of surgical treatment is trapeziectomy. Some surgeons combine this with additional ligament reconstruction and tendon or capsular interposition techniques to provide a more stable base for the thumb metacarpal.
Purpose:
In modern Orthopaedic practice, arthroplasty is the procedure of choice for many end-stage arthritic joints. However, due to the reliable and reproducible outcomes of trapeziectomy, this has yet to be widely adopted by hand surgeons in the management of TMJ arthritis. Recent series of arthroplasty implants have consistently shown good outcomes and trapezio-metacarpal joint replacement has been observed to provide excellent long-term function in the fit and active patient.
Methods:
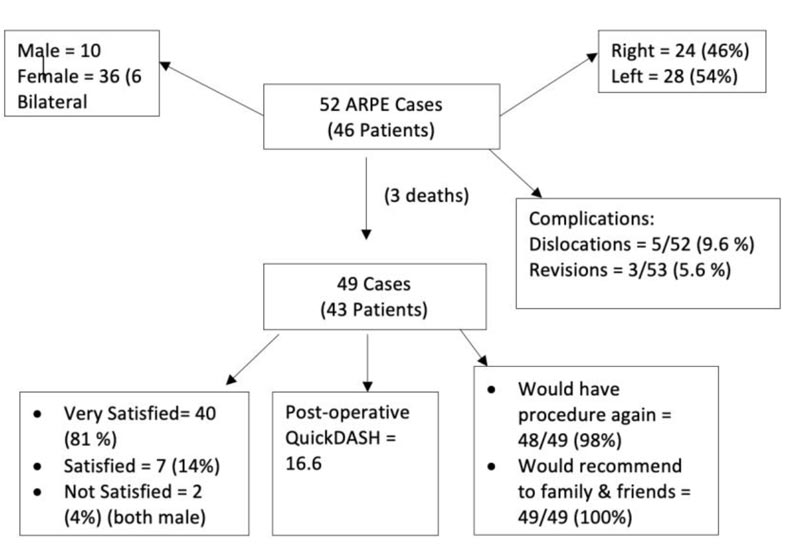
We have performed a total of 52 TMJ arthroplasties in 46 patients in our institution for over 5 years (2011 to 2016). After excluding 3 cases, 43 available patients (49 implants) were subsequently asked to submit QuickDASH scores and a patient satisfaction survey.
Results:
Average QuickDASH score was 16.6, with high patient satisfaction postoperatively at 1 year. Complications included one intraoperative fracture, and five cases of post-operative instability/ dislocation. Dislocations were treated successfully with open reduction and revision.
Conclusion:
TMJ arthroplasty has shown good outcomes and patient satisfaction with a low revision rate and we recommend its use in active patients with well-preserved scapho-trapezio-trapezoid (STT) joints.
1. INTRODUCTION
Trapezio-Metacarpal Joint (TMJ) is one of the most common joints affected by osteoarthritis. The thumb bears increasing loads from the tip to the base and culminates in a force as high as 120 kilograms, generated at the thumb carpometacarpal joint during a forceful pinch [1]. The incidence of TMJ arthritis is high in post-menopausal females, which has been postulated to be secondary to ligamentous laxity. Conservative measures include physiotherapy, splinting and steroid injections. When these methods fail to address patients’ symptoms, operative treatment via a trapeziectomy is often recommended. There have been several modifications to trapeziectomy, such as adjunctive Ligament Reconstruction and Tendon Interposition (LRTI) to act as a ‘sling’ to support the first metacarpal. Temporary pinning using Kirschner wires has also been used to improve postoperative stability and reduced the collapse of the first metacarpal. However, there remains no evidence to demonstrate that any adjunctive measure contributes to improved post-operative function and satisfaction either in the short or long term [2-4]. Trapeziectomy is, however, associated with a weakened pinch grip post-operatively of up to 20% [5], which is especially undesirable in the younger, more active patient cohort. Again, measures taken to maintain trapezial space height have not been shown to influence post-operative function [4, 6]. Furthermore, literature exists that demonstrates evidence of dorsal intercalated segmental instability following trapeziectomy, secondary to disruption of the STT ligament complex [7].
TMJ arthroplasty is now widely in practice [8]. Theoretically, joint replacement provides a more stable and pain-free joint. Patient satisfaction, therefore, tends to be higher when comparing the two modalities of treatment [9].
Initially, reports of titanium on cemented polyethylene implants in the 1980s demonstrated good pain relief, but with a relatively high incidence of loosening at the cement-bone interface. When silicon implants were compared to TMJ fusion and trapeziectomy, no functional benefit or improvement in pain was observed in any one group over the other [10]. Silicon implants also caused ‘siliconitis', a tissue reaction to silicon-based implants that has rendered these implants unpopular, and metallic on polyethylene prostheses are now the mainstay of bearing combination in TMJ arthroplasty. There has been a rapid evolution in the design and technique of implant insertion, and there are now several available in the market. The commonly available implants for TMJ arthroplasty are ARPE (Biomet, Warsaw, Indiana, USA), Elektra (Small Bone Innovations, Peronnas, France), MAIA (Sovereign Medical Limited, Essex, UK), Roseland (Depuy, Leeds, England) and the Ivory implant (Memometal, Stryker Corporate, Michigan, USA).
Reported outcomes of the ARPE implant thus far are promising, with the results demonstrating good survival rates and better functional improvement compared to the trapeziectomy alone [11-13]. The risk of wear and loosening over time remains, and studies looking at longer-term outcomes are not yet available. The purpose of this study was to assess the short and medium-term functional outcomes, complication rates, patient satisfaction, and survival of TMJ Arthroplasty using the ARPE implant.
2. MATERIALS AND METHODS
Between January 2011 and June 2016, we performed 52 total joint replacements for TMJ osteoarthritis. All procedures were performed in a single center by a single fellowship-trained hand surgeon. The mean patient age at the time of surgery was 58.3 years (SD 8.3). Total number of patients was 46 – 36 females and 10 males. Six patients had bilateral procedures. All bilateral cases were performed in female patients. Twenty-four cases were in the right hand and twenty-eight in the left hand. Three patients had died at the time of study and outcomes for their TMJ replacement was not available. Patients with bilateral procedures completed separate questionnaires for each side. The indication for surgery was painful TMJ arthritis of the thumb, without evidence of STT arthritis, which had not responded adequately to conservative measures. All patients were counselled regarding the options of TMJ replacement and trapeziectomy. Radiographs were assessed for evidence of concurrent STT joint arthritis or Stage 4 changes according to the Eaton-Littler classification [14]. If present, trapeziectomy was offered instead as standard treatment. Patients were also informed about the risk of intra-operative fractures, which would also result in performing a trapeziectomy. This occurred on one occasion and the patient did not have a TMJ replacement.
Finally, during the consent process, both total joint arthroplasty and trapeziectomy were offered to the younger and more physically active individuals, whilst lower demand patients received standard trapeziectomy (Fig. 1).
3. SURGICAL TECHNIQUE
All procedures were carried out through the dorsal approach. Non-retentive trapezial components were used.
A 3 cm longitudinal incision is made, centered over the thumb carpometacarpal joint. Branches of the superficial radial nerve are protected and the abductor pollicis longus and extensor pollicis brevis tendons retracted. An ulnarly based capsular flap is raised exposing the CMC joint. The proximal 5 mm of the metacarpal is resected with an oscillating saw. Any ulnar osteophytes are resected. The metacarpal is prepared by sequential broaching until cortical contact is made and the trial metacarpal component is inserted. The trapezium is levelled with a saw using the resection guide. The center of the trapezium is identified, and the bone is prepared with a curette and the 9 mm reamer. The reamer is inserted until it is 1 mm below the bone surface. The trapezial component is then inserted and a trial reduction carried out to check stability and range of motion. The definitive metacarpal component is then inserted followed by the neck/head component after a further trial. The capsular flap is replaced and sutured with 3-0 polydioxanone sutures.
A thumb spica backslab is applied and the limb supported in a sling. The patient is reviewed after 2 weeks at which point the slab and sutures are removed and a radiograph obtained. At this point, the patient can begin moving the thumb.
When we started performing the procedure, as per the recommendation of the implant manufacturer, a wool and crepe bandage was applied without a slab. However, as we encountered dislocations in the first 2-3 weeks following surgery, we now routinely apply a plaster-of-Paris back slab protecting the thumb for 2 weeks. Patients are reviewed at 2 weeks in the outpatient clinic for removal of slab, wound review and clinical examination. They are advised to gradually return to routine activities and routine referral to hand therapy is not done. Plain radiographs are taken at 6 weeks and at the final 1-year follow-up.
Outcomes were assessed through postal questionnaires. Six patients did not return the forms by post and were contacted via telephone by the lead author (IM) and their scores were recorded accordingly. Three patients had deceased, and outcome data were obtained from all 43 remaining patients. The main outcome score used was the Quick-DASH score. Additionally, the patients were asked about their satisfaction, whether they would have the procedure again, recommend the procedure to their family or friends, return to the previous level of activity and finally if they had any major problems related to the procedure. A literature review was performed using MEDLINE for the last 10 years between 2006 and 2016 using search terms “Trapeziometacarpal”, “Trapezio-metacarpal” “Thumb”, “Arthritis”, “Arthroplasty” and “CMCJ”.
4. RESULTS
4.1. Patient Outcome Measures and Satisfaction
The mean post-operative QuickDASH score was 16.6 (SD 19.75). Out of the 49 cases, 40 (81.60%) were very satisfied and 7 (14.28%) were satisfied. Two (4%) patients were not satisfied. These were both males and had persisting pain. Despite this, 48 of the 49 patients (97.9%) said they would have the procedure again and all patients (100%) would recommend the procedure to a friend or family member Fig. (2).
4.2. Dislocations
There were 5 out of 52 (9.6%) joint dislocations. Three of these were in males and two in females. All occurred within the initial two weeks of surgery (mean 10 days – Range 3-13). Closed reduction was unsuccessful in all cases and the joints were reduced with an open technique and a plaster of Paris cast was applied for 2 weeks. In one case, a fall post-operatively had resulted in a peri-prosthetic trapezium fracture, resulting in dislocation. A revision was thus abandoned and a trapeziectomy performed. This experience led to a change in practice, and we routinely use a constrained cup for the Trapezium. At the time of writing, there have been no further joint dislocations following this change.
4.3. Revision
Three cases required revision (5.6%). Two were revised for painful mal-position, and one case was revised for mal-position and dislocation.
4.4. Other Complications
Six patients (11.5%) still had persisting pain, two of which required revision for mal-position of the implant. There were no cases of deep or superficial infection in this series. There was one case of intra-operative fracture of the trapezium during implantation of the cup and a trapeziectomy was performed in this case. This case has, therefore, not been included in the analysis of our study as the patient had a standard trapeziectomy. It was decided not to include the outcomes for this single patient. However, this is a recognized complication and patients are counselled regarding this scenario.

5. DISCUSSION
Arthroplasty of the TMJ is increasing in popularity in the management of TMJ arthritis. Although arthroplasty is the mainstay of treatment for most arthritic joints in the body, it is yet to be universally adopted in the case of TMJ osteoarthritis. Literature reporting longevity and outcomes are relatively scarce and limited to case series. At present, the lack of inclusion in the joint registries is a large contributing factor to this. Trapeziectomy is an effective treatment modality providing long-term pain relief [5] and is appropriate in cases of pan-trapezial arthritis. However, evidence suggests that post-operatively patients report weakened pinch grip and substitute a decrease in function for pain relief [5], and that adjunctive measures such as ligamental suspension do not influence this significantly [2, 3, 15]. We believe that in the correct patient with isolated TMJ disease, arthroplasty achieves excellent functional results with a low complication rate when done regularly. It should, therefore, be considered for those patients who are younger, fitter and have higher functional demands but the careful discussion regarding complications and need for revision surgery is vital.
In comparison to trapeziectomy, TMJ arthroplasty provides inherent stability and maintenance of carpal height. This can lead to earlier return to work and activities of daily living. Our results at 1 year demonstrate extremely high patient satisfaction rates of 95% following TMJ arthroplasty. QuickDASH scores post-operatively were very promising, with a mean score of 16.6 (SD 19). This is representative of a functional score of ‘little difficulty’ being rated for all tasks included. This supports the outcomes of other authors with regards to implant survival and QuickDASH score.
Brutus [16] demonstrated that functional results and pain relief at 6 months in 63 patients were excellent following TMJ replacement using the ARPE implant. In the longer term, Jacoulet et al. [17], Eecken et al. [11] and Martin-Ferrero [12] reported excellent medium-term results with the ARPE replacement at 5, 6 and 10 years, respectively.
Other implants used also yield promising results. Krukhaug et al. [18] reported a 90% 5-10 year survival in 479 cases performed using a combination of Swanson Silastic, Swanson titanium, Motec and Elektra Implants. Interestingly, they report that the newer metal implants did not outperform/outlive the Silastic/monoblock variants. Regnard [19] et al. reported on their first 100 cases using the Electra TMJ replacement prosthesis. Their results showed good outcomes in 83 out of the 100 cases at a mean follow-up of 54 months. Badia [20] reported excellent outcomes in 24 out of 26 TMJ replacements in their series using the Braun-Cutter implants.
As with every form of arthroplasty, revision is an expected long-term concern. This is most commonly due to mechanical wear of the prosthesis, but can also be due to secondary instability, component malposition, or peri-prosthetic fracture. Hansen [21] cited learning curve as a possible reason for a high failure rate in their early experience with the Elektra implant in 17 cases. A further report from Hansen [22] reported poor outcomes with the Moje Acamo TMJ arthroplasty prosthesis. In our series, 6 prostheses out of 52 required early revision. The main cause for revision was dislocation (5/6), the rate of which was immediately influenced by a change in practice – cast immobilization for 2 weeks post-operatively. Interestingly, 3 out of 6 dislocations occurred in males, although the ratio of males:females undergoing the procedure was 1:7. This preponderance for dislocation in the male cohort could be reflective of increased functional demand at an earlier stage, and should be taken into consideration during the consent process and peri-operative management/immobilization. The ARPE cup is uncemented, but Hansen reported no significant difference in functional outcomes and revision rates between cemented and uncemented cups [23].
Both dislocation and aseptic loosening are reported as common complications in the literature, regardless of implant choice. Dislocation rates seem quite consistent across the current literature in ARPE prosthesis, with 5-9% [11, 16, 17, 19, 24] being quoted in comparison to our incidence of 9.6%. Krukhaug et al. evaluated 479 primary TMJ replacements, analysis of which did not indicate gender or age to be predisposing factors for revision rate [18]. Thillerman reported a 2 year cumulative revision rate of 42% in their series of 42 Motec TMJ replacement [25]
Loosening is another relatively common complication, mainly of the trapezial component, which has been reported in various prostheses. Apard revised 5 out of 43 ARPE prostheses for loosening [24], and Hernández-Cortés [26] and Klahn et al. [27] cited the failure of the trapezial component as being responsible for loosening in 44-47% of their Electra implants after 5 years.
In the case of failed joint replacement secondary to instability, loosening, on-going pain or dissatisfaction, the salvage procedure would be a secondary Trapeziectomy. In a series of 15 such cases, when compared with age and sex-matched subjects, it was shown that this cohort performed equally well in DASH score and strength testing as those having undergone primary Trapeziectomy [4].
This study does have some limitations. Due to its retrospective nature, pre-operative functional scores are not available, nor is functional comparison with age/sex-matched cohorts with trapeziectomy i.e. lack of a control arm. Follow-up was excellent, however, and apart from those patients who had deceased, 100% follow-up at 1 year with satisfaction scores was achieved. Six patients had bilateral procedures and they completed questionnaires for each side in order to document the effect of each procedure. The effect of the procedure on the one hand may skew the results of the procedure on the contralateral side and therefore, affect the overall outcomes of the study.
CONCLUSION
This study supports the growing body of evidence for TMJ arthroplasty. It demonstrates excellent functional outcomes scores using QuickDASH and patient satisfaction in the short and medium-term, with a low complication rate. Following 5 early joint dislocations (1 secondary to trauma), we would advocate the use of a constrained prosthesis and immobilization for a period of at least 2 weeks. This had a demonstrable and seemingly immediate effect on the rate of dislocation in our series, without evidence of impaired functional scoring. Further work is required over the next 5-10 years to evaluate the lifespan of these implants and establish long-term outcomes.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The project was case note review and patient outcomes recording after informed consent and did not require formal ethical approval after review by our institutional research department.
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. Reported experiments on humans were in accordance with the ethical standards of the committee responsible for human experimentation (institutional national), and with the Helsinki Declaration of 1975, as revised in 2008.
CONSENT FOR PUBLICATION
Informed consent was taken from all patients and all patients completed the study questionnaires.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
The study was performed in the authors’ personal time and involved a review of case notes and was not funded by any organization. The minimal cost of postage of questionnaire was borne by the authors.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


