REVIEW ARTICLE
Muscle Damage in Different Approaches in Total Hip Arthroplasty According to Serum Markers
Stylianos Tottas1, *, Aliki Fiska2, Ioannis Kougioumtzis1, Athanasios Ververidis1, Konstantinos Tilkeridis1, Georgios I Drosos1
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 97
Last Page: 108
Publisher ID: TOORTHJ-13-97
DOI: 10.2174/1874325001913010097
Article History:
Received Date: 15/12/2018Revision Received Date: 04/03/2019
Acceptance Date: 07/03/2019
Electronic publication date: 28/03/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: (https://creativecommons.org/licenses/by/4.0/legalcode). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Total Hip Arthroplasty (THA) is the final treatment of end-stage hip osteoarthritis. Nowadays, THA has become very common, cost- effective and one of the most successful orthopaedic procedures. Recently, surgeons have shifted their interest to approaches according to Minimally Invasive Surgery (MIS). These approaches are either modifications of conventional approaches or they are designed from the beginning as MIS approaches. Muscle damage and soft tissue damage are issues that concern researchers who perform studies on THA.
Objective:
The aim of this study is to review the literature concerning studies by comparing different approaches using serum and inflammatory markers for muscle and soft tissue damage.
Methods:
We searched the PubMed database in the English language systematically for clinical studies or reviews, comparing muscle damage according to serum markers between two or more approaches in primary total arthroplasty.
Results:
In total, twenty-one studies were included in this review. Although the results are controversial, it seems that MIS approaches in most of the studies were related to lower levels of inflammation markers contrasting with conventional approaches. Nevertheless, this difference in muscle damage is not correlated with a difference in functional scores or other perioperative data and clinical outcomes in all studies.
Conclusion:
The existing literature does not lead to a safe consensus about the superiority of any approach. Therefore, there is still a need for further research with well-designed studies.
1. INTRODUCTION
Total Hip Arthroplasty (THA) is the final treatment of the end-stage hip osteoarthritis [1]. Patients undergo THA to be relieved from pain and to regain the function of their affected hip joint [2]. Nowadays, THA has become very common, cost-effective and one of the most successful orthopaedic procedures [2-4] and is referred to as “the operation of the century” [1].
There is a variety of surgical approaches which are used in THA. The conventional approaches are the anterior approach which was modified and popularized by Smith-Petersen and by siblings Judet J and Judet R [5, 6], the anterolateral approach which was initially described by Watson-Jones [7], the lateral approach which was described by McFarland and Osborne [8] and modified by Bauer [9] and Hardinge [10] and the posterior approach which was popularized by Moore [11].
In the last two decades, surgeons have shifted their interest in approaches to Minimally Invasive Surgery (MIS). These approaches are either modifications of conventional approaches or they are designed from the beginning as MIS approaches [12-14]. Procedures with MIS approaches have the objective of minimizing soft tissue damage, reducing postoperative pain and blood loss and improving functional outcome [15]. However, there is no consensus among researchers as to which are clear specifications for determining an approach as “minimally invasive”.
Many well-designed studies compare two or more approaches on the basis of different factors and try to prove which is more appropriate and has the least postoperative complications. These factors may be postoperative functional recovery using protocols (Harris Hip Score, HOOS – Hip disability and Osteoarthritis Outcome Score, etc.) [16], implant positioning through radiographic evaluation [17], or gait analysis [18].
Furthermore, muscle damage and soft tissue damage are issues that concern researchers who perform studies on THA. Consequently, there have been efforts to understand which approaches cause less muscle damage and minimize the adverse effects after surgery. The extent of muscle damage can be estimated by levels of serum and inflammatory markers [19], Magnetic Resonance Image (MRI) analysis [20], or surgical techniques in cadaveric studies [21, 22]
Many conducted studies include intraoperative evaluations such us blood loss, operative time, days of hospitalization, anesthetic methods, possible complications etc. which are collated with different approaches. The insights gained from the existing literature are confused because there is no clear-cut answer as to which approach confers better clinical results.
The aim of this study is to review the literature concerning studies comparing different approaches using serum muscle and soft tissue as well as inflammatory markers.
2. MATERIALS AND METHODS
An extensive search of the PubMed/Medline database was conducted by two authors (ST) and (GD) separately in June 2018 in the English language (Fig. 1). The search terms were ‘total hip arthroplasty’, ‘total hip replacement’,’ muscle damage’, ‘approach’, ‘serum markers’, ’inflammatory markers’ and were combined using the Boolean operators “AND” or “OR.” The lists of similar articles of the reported articles were also evaluated. Furthermore, the reference lists of the included articles were investigated manually to obtain additional trials.
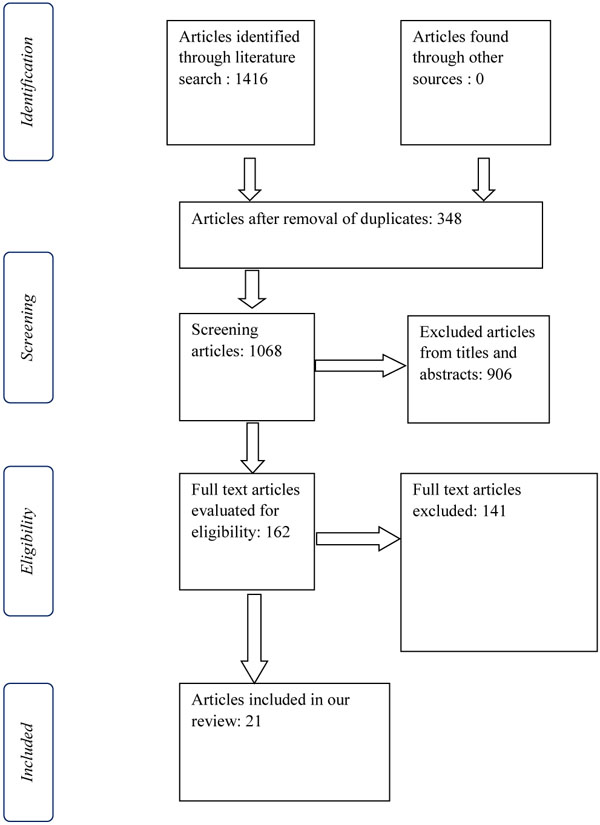 |
Fig. (1). Flow diagram of study selection. |
We included studies which were RCT’s, prospective comparative studies. A study was deemed appropriate if it compared two or more approaches to total hip arthroplasty/ replacement and enclosed indispensably serum markers for muscle damage. To enhance the level of evidence we searched reviews comparing muscle damage in THA according to serum markers.
In total, we found 21 articles which are demonstrated in Table 1. We considered that ethical approval was not required for our study, because it was a literature review and we did not include any medical data of our patients.
All abbreviations and their explanations are included in Table 2 for the reader’s convenience.
| Study | Compared Approaches | Patients | Serum Markers | Results Biomarkers |
Other (pain, function, etc) |
Study Type |
|---|---|---|---|---|---|---|
| 1. Anterior approach versus posterior approaches | ||||||
| Difference in biomarkers | ||||||
| Bergin et al. (2011) [19] | Minimally invasive direct anterior (MIS-DA) vs minimally invasive posterior(MIS-PO) | MIS-DA: 29MIS-PO: 28 | CK, CRP, IL-6, IL-1b, TNF-a | MIS-DA: Lower levels of all markers | MIS-PO: Significant higher operative time and incision length | PRCS |
| Zhao et al. (2017) [41] | Anterior (DAA) vs Postero-lateral (PLA) | DAA: 60 PLA:60 |
CRP, ESR, IL-6 | DAA: Lower levels of all markers the first 4 POD | DAA: Better HHS, UCLA in 3 months | RCT |
| Poehling-Monaghan et al. (2017) [42] | Anterior (DAA) vs Mini Posterior (MPO) | DAA: 50 MPO: 50 |
CK, myoglobin, CRP, TNFa, IL-6 | DAA: Lower levels of all markers with MPA | Pain scores: No significant difference | PRCS |
| No difference in biomarkers | ||||||
| Pilot et al. (2006) [37] | Minimal invasive direct anterior (MIS-DA) vs Postero-lateral (PLA) | MIS-DA: 10 PLA: 10 |
H-FABP, myoglobin, CK, ASAT, LDH, IL-6, IL-10 | No significant differences between the groups | MIS-DA: Higher blood loss (not significant), Longer operative time | PRCS |
| Rykov et al. (2017) [43] | Anterior (DAA) vs Postero-lateral (PLA) | DAA: 23 PLA: 23 |
CK, CRP | No significant differences between the groups | HHS, HOOS: Similar | RCT |
| 2. Anterior approach versus lateral approaches | ||||||
| Difference in biomarkers | ||||||
| De Anta-Díaz et al. (2016) [44] | Anterior (DAA) vs Lateral (LA) | DAA: 49 LA: 50 |
IL-1, IL-6, IL-8, IL-10, IL-12, TNF, CK, ESR, CRP | DAA: Lower levels of biomarkers | MRI: Less soft tissue damage HHS: Similar results |
RCT |
| Nistor et al. (2017) [45] | Anterior (DAA) vs Lateral (LA) | DAA: 35 LA: 35 |
Myoglobin, CK, LDH | DAA: Lower levels of myoglobin CK and LDH: No significant difference |
DAA: Less pain the 1st POD | RCT |
| Mjaaland et al. (2015) [46] | Minimally invasive direct anterior (MIDA) vs direct lateral (LA) | MIDA: 83 LA: 80 |
CK, CRP | LA: Lower CK levels in 4th POD | MIDA: Less pain | RCT |
| 3. Anterolateral versus other approaches | ||||||
| Difference in biomarkers | ||||||
| Mouilhade et al. (2010) [47] | Minimally invasive antero-lateral (Watson-Jones) approach (MIS-AL) with an AL approach with anterior hemimyotomy | MIS-AL: 92 AL-HM: 49 | Myoglobin, CPK | MIS-AL: Lower of CPK at 1st and 2nd POD | MIS-AL: Better functional outcomes at 6 weeks. Less variation of cup inclination. | PRCS |
| Inaba et al. (2011) [48] | Modified Watson-Jones (M-AL) vs modified mini-incision direct lateral approach (MIS-LA). | M-AL: 57 MIS-LA: 60 |
CRP, CK | M-AL: Lower CK levels at 1st POD | Pain and functional outcome: No notable difference | RCT |
| Muller et al. (2011) [20] | Minimally invasive anterolateral (MIS-AL) vs modified direct lateral approach (M-LA). | MIS-AL: 21 M-LA: 16 |
CK, myoglobin | MIS-AL: Lower CK levels at 6 hours and 1st POD | MIS-AL: Less muscle damage | RCT |
| Matziolis et al. (2011) [49] | Minimally invasive anterolateral (MIS-AL) vs minimally invasive transgluteal (MIS-TG) | MIS-AL: 20 MIS-TG: 20 |
sTnI | MIS-AL: Lower levels of sTnl the 1st POD | Similar: Hospitalization, blood loss and complications | RCT |
| No difference in biomarkers | ||||||
| Landgraeber et al. (2013) [50] | Minimally invasive anterolateral (MIS-AL) vs conventional lateral (LA) | MIS-AL: 36 LA: 40 |
CK, CRP | No significant difference | Functional outcomes and pain: No significant difference.MISAL: Longer operating time and greater blood loss | RCT |
| 4. Posterior approach versus minimally invasive posterior approach | ||||||
| Difference in biomarkers | ||||||
| Suzuki et al. (2004) [51] | Conventional posterolateral (PLA) vs minimally invasive posterolateral (MIS-PLA) | PLA: 39 MIS-PLA: 61 |
CRP, ESR, CPK | MIS-PLA: Lower CRP and ESR levels at 1st week CPK levels: No significant difference |
MIS-PLA: Shorter operative time, lower blood loss, less hospital stay. Functional outcomes: Similar |
PRCS |
| Kwak et al. (2014) [40] | Conventional posterolateral (PLA) vs minimally invasive posterolateral (MISPLA) | PLA: 15 MIS-PLA: 15 |
CK, IL-6, IL-8, IL-10, IL-1, aldol-se | MISPLA: Lower levels of CK, IL-6, IL-10, IL-1 at 1st and 3rd POD and IL-8 at 7th POD | MIS-PLA: Less blood loss | PRCS |
| No difference in biomarkers | ||||||
| Fink et al. (2010) [52] | Conventional posterolateral (PLA) vs minimally invasive posterolateral (MIS-PLA) | PLA: 50 MIS-PLA: 50 |
CPK, CK-MM, myoglobin, CRP | No significant differences | MIS-PLA: Lees pain, lower blood loss, less hospital stay | PRCS |
| 5. Lateral approach versus minimal incision lateral | ||||||
| Mazoochian et al. (2009) [53] | Standard lateral (LA) vs minimally invasive lateral approach | LA: 26 MIS-LA: 26 |
CK, myoglobin | MIS-LA: Statistically lower myoglobin levels at 6 h postoperatively | MIS-LA: Shorter operating time, less blood loss and better functional results (HHS- 6 weeks and 3 months) (WOMAC-3 months) | RCT |
| Dienstknecht et al. (2014) [54] | Conventional lateral, transgluteal approach (Bauer) (LA) vs mini-incision (MIS-LA) | LA: 88 MIS-LA: 55 |
CK, CRP | No significant difference | MIS-LA: Lower VAS pain all POD / Shorter operative time | RCT |
| 6. Standard lateral and postero-lateral versus minimally invasive lateral and posterolateral | ||||||
| Shitama et al. (2009) [55] | Conventional lateral (LA), Conventional or postero-lateral (PLA) vs minimally invasive lateral (MIS-LA) and posterolateral (MIS-PLA) | LA: 8 PLA: 20 MIS-LA: 15 MIS-PLA: 19 |
IL-6, CRP | No significant different | Shorter operative time with the standard group | RCT |
| Goosen et al. (2011) [56] | Conventional lateral (LA), Conventional or postero-lateral (PLA) vs minimally invasive lateral and posterolateral | LA: 20 PLA: 20 MIS-LA: 20 MIS-PLA: 20 |
CK, Myoglobim | No significant difference | Shorter operative time with the standard group | Double- blind RCT |
| 7. Three different MIS approaches | ||||||
| Cohen et al. (2009) [57] | Modified Watson Jones (MIS-AL), vs minimally invasive posterior (MIS-I) vs minimally invasive two incision (MIS-II) | MIS-AL: 10 MIS-I: 10 MIS-II: 10 |
CK, CPK, myoglobin | No significant different | Smaller duration of surgery and lower rates of blood loss with MIS-AL | COS |
| Abbreviation | Definition |
|---|---|
| THA | Total Hip Arthroplasty |
| DAA | direct anterior approach |
| PLA | posterolateral approach |
| LA | lateral approach |
| MPA | miniposterior approach |
| PA | posterior approach |
| DLA | direct lateral approach |
| MIDA | minimally invasive direct anterior |
| WJ | Watson-Jones |
| MWJ | modified Watson-Jones |
| Mini-WJ | mini Watson-Jones |
| AHM | Thomine’s anterior hemimyotomy |
| MI-PmG | Mini-posterior modified Gibson |
| C-PmG | Conventional - posterior modified Gibson |
| ALMI | Mini anterolateral |
| AL | Anterolateral |
| mDL | modified direct lateral |
| TG | Transgluteal |
| TL | Translateral |
| MIS | minimally invasive |
| HHS | Harris Hip Score |
| WOMAC | Western Ontario and McMaster Universities Osteoarthritis Index |
| HOOS | Hip disability and Osteoarthritis Outcome Score |
| PMA | Postel Merle d’ Aubigne Hip Score |
| RCT | randomized controlled trial |
| PRCS | Prospective comparative study |
| COS | cohort study |
| POD | postoperative day |
| Serum marker | Definition |
|---|---|
| CRP | C-reactive protein |
| LDH | lactate dehydrogenase |
| TNF-a | tumor necrosis factor-a |
| ESR | erythrocyte sedimentation rate |
| IL | Interleukin |
| CK | creatine kinase |
| CK-MM | creatine kinase – muscle specific |
| H-FABP | Heart-type fatty acid binding protein |
| ASAT | aspartate aminotransferase |
| sTnI | Skeletal troponin I |
3. SERUM / INFLAMMATORY MARKERS
As THA has evolved, many surgeons have affiliated MIS approaches. One of the challenge researchers cope with, is to determine the invasiveness of every approach. It has been proposed that measurement of serum and inflammatory markers consists of an objective method to assess the extent of the intervention of soft tissue and muscles in different approaches in THA. A variety of humoral mediators and acute-phase proteins may be raised, in response to soft tissue impairment after surgery.
C-Reactive Protein (CRP) is an acute-phase protein secreted by the liver and induced by pro-inflammatory cytokines. Its serum levels increase in trauma, inflammation or infection [23, 24]. CRP has brief half-time and its levels correspond to the potency and duration of the inflammatory factor [25].
Erythrocyte sedimentation rates (ESR) express the feature of erythrocytes to adhere together and descend through the blood plasma at the bottom of the container in 60 minutes [26]. ESR levels are increased in inflammation, infection, malignancy, pregnancy, anemia, heart malady, renal failure, collagen vascular disease and any other clinical situation that raise fibrinogen [27].
Lactate Dehydrogenase (LDH) catalyzes the anaerobic transformation of pyruvate to lactate and creatine kinase (CK) catalyzes the ATP-dependent phosphorylation of creatine [28, 29]. The use of both enzymes has been widespread regarding soft tissue injury [30].
TNF-a is an acute phase protein generated during the process of inflammation. It interferes in vascular endothelial cells and accelerates the formation of clotting, atherosclerotic plaque and damage of vessels [31]. Interleukins (IL) consist of a large category of over 50 cytokines produced by molecules of the immune system. They stimulate intricate immu- nomodulatory activities depending on different causative factors [32]. In some studies of our review, IL-1, IL-6, IL-8, IL-10, IL-12 and IL-1β were used to evaluate muscle damage.
Myoglobin is a protein that is crucial for intracellular pervasion of oxygen in muscles [33] and is elevated in the circulatory system in the case of muscle injury [34].
Heart-type fatty acid binding protein (H- FABP) was initially used as a vulnerable biomarker for cardiac muscle injury [35]. Afterward, its relation to skeletal muscle trauma was investigated as well. In 2005, Maurice M.A.L. Pelsers et al. in their review inquired into the repercussions of H-FABP levels after other diseases including skeletal muscle injury. They underlined that the concurrent evaluation of H-FABP and myoglobin serum levels is a contributory factor to determine skeletal muscle impairment [35].
Aspartate Aminotransferase (ASAT) is an enzyme found principally in liver tissue, but also in other tissues including muscles [36]. Consequently, it has been used as a marker for muscle damage as well [37].
Furthermore, skeletal troponin I (sTnI) has been established as a susceptible serum marker of muscle injury [38, 39]. Finally, aldolase is an enzyme that catalyzes the transmutation of fructose to glyceraldehyde and dihydroxyacetone and is plentiful in muscle tissue [40].
4. RESULTS
4.1. Anterior Approach Versus Posterior Approaches
4.1.1. Difference in Biomarkers
Bergin et al. (2011) conducted a level II comparative study between minimally invasive direct anterior (MIS-DA) and minimally invasive posterior (MIS-PO). CK, IL-6, IL1β and TNF-a markers were evaluated preoperative, immediately after surgery and on 1st and 2nd POD. CRP was measured at 1st and 2nd POD. The results indicated the superiority of MIS-DA, because lower levels of all inflammatory markers were estimated compared with MIS-PO. Especially, CK levels elevated 5.5 times higher with MIS-PO instantly after the operation. According to the evaluation of the outcome, CK levels seemed to correlate with the surgical approach, blood loss and transfusion. IL-6 was related to blood loss and IL-1β with ASA grade, incision extent and transfusion. From all the perioperative patient’s elements, significantly higher operative time and incision length in the posterior group were observed [19].
Zhao et al. (2017) in their RCT highlighted the efficacy of direct anterior approach (DAA) with the posterolateral approach (PLA). The measured serum markers at 1st – 4th (post-operative day (POD) were CK, CRP, IL-6, ESR. DAA was related to statistically significant reduced levels of all markers. Proportionately, patients with DAA needed less time for hospitalization and reported less perceived postoperative pain. Furthermore, functional outcomes using Harris Hip Score (HHS) and University of California Los Angeles activity score (UCLA) indicated the superiority of DAA in 3 months after the operation but no statistically significant discrepancies in 6 months. Conversely, PLA outweighed DAA in terms of less intraoperative blood loss and shorter operative time [41].
Similar results were reported by Poehling-Monaghan et al. (2017), who investigated the association between serum markers and functional outcome in direct anterior approach (DAA) compared to mni-posterior (MPO) approach. They included CK, CRP, IL-6, TNF-a and myoglobin measured at 1st and 2nd POD. Patients who underwent mini-posterior approach had more increased CK, CRP, myoglobin and IL-6 levels than the DAA. Although the greater muscle damage due to serum markers with the mini-posterior approach did not have implications in postoperative functional outcome and VAS pain, no statistically significant differences between two approaches were observed [42].
4.1.2. No Difference in Biomarkers
Pilot et al. (2006) conducted a non-randomized, non-blinded comparative study between minimally invasive direct anterior (MIS-DA) and conventional posterolateral approach (PLA). They measured the inflammatory markers H-FABP, IL-6, ASAT, LDH, CK and myoglobin preoperatively and postoperatively at 2 hours, 4 hours, 6 hours, 1st POD and 3rd POD. On the contrary, no functional outcomes were recorded. Researchers concluded that serum marker levels were influenced proportionately in both approaches without significant differences. Quaintly, there was slightly higher blood loss in patients undergoing MIDA approach. The authors assumed that this is a consequence of the required long operative time for MIDA [37].
Rykov et al. (2017) in their RCT compared direct anterior approach (DAA) with a posterolateral approach (PLA). In terms of muscle damage, CRP and CK markers were evaluated preoperatively and postoperatively at 2 hours, 1st POD, 1st week and 6th week. Furthermore, functional outcomes were assessed with HHS and HOOS preoperatively and 6th week postoperatively. The obtained results revealed no significant discrepancies between the approaches [43].
4.2. Anterior Approach Versus Lateral Approaches
De Anta-Díaz et al. (2016) conducted an RCT comparing direct anterior approach (DAA) with the lateral approach (LA) evaluating soft tissue and muscle damage and functional outcomes. Muscle damage was evaluated with the markers IL-1, IL-6, IL-8, IL-10, IL-12, TNF-a, CK, ESR, CRP. Furthermore, researchers incorporated MRI analysis of the affected soft tissue based on a protocol, pre-operatively and 6 months after surgery. DAA was recorded to have statistically significant lower levels regarding IL-6 at 1st POD, IL-8 at 4th POD, CK at 4th POD, CRP at 15th POD and ESR at 30th POD. MRI findings tracked down greater fatty atrophy in all gluteus muscles with LA. On the other hand, although DAA was found to preserve soft tissue intact better, that was not reflected in postoperative functional outcomes and both groups registered with equivalent HHS. The authors inferred that both approaches are efficient and safe, pointing out that the experience of the surgeon is crucial [44].
Nistor et al. (2017) in their RCT compared 35 patients with a direct anterior approach (DAA) and 35 patients with a lateral approach (LA). They studied muscle damage using myoglobin at 1st POD and CK and LDH serum markers for the first 5 POD. Additionally, postoperative pain, implant positioning and possible complications were assessed. Myoglobin levels were distinctively lower with DAA, but no significant differences in other markers were noticed. Additionally, they reported no differences in terms of postoperative complications and radiographic evaluation. Nevertheless, DAA was related to less postoperative perceived pain especially the 1st POD [45].
Similar results recorded by Mjaaland et al. (2015) compared minimally invasive direct anterior (MIDA) with direct lateral (LA). The authors did not find distinctive differences in terms of CRP the first four POD between the two approaches, but CK levels were estimated significantly lower with LA at 4th POD. Nevertheless, MIDA was proved more efficient as far as postoperative pain was concerned, because it was associated with less pain at all POD [46].
4.3. Anterolateral Approaches vs. Lateral Approaches
4.3.1. Difference in Biomarkers
Mouilhade et al. (2010) conducted a multicenter prospective study contrasting minimally invasive antero-lateral (Watson-Jones) approach (MIS-AL) with an anterolateral approach with anterior hemimyotomy (AL-HM) in terms of muscle damage with serum markers, functional outcomes, complications and radiographic assessment. Lower CPK levels were recorded at first two POD in patients undergoing MIS-AL, but no significant differences were recorded at myoglobin levels 10 hours postoperatively between the two approaches. MIS-AL revealed better functional outcomes at 6 weeks postoperatively using PMA, HHS, WOMAC. X-rays showed less fluctuation rates in cup inclination with AL-HM. Finally, there were no considerable discrepancies regarding blood loss and complications [47].
In 2011, Inaba et al. (2011) compared the modified Watson-Jones (M-AL) and modified mini-incision direct lateral approach (MIS-LA). CRP and CK levels were measured immediately after the operation, and at 1st, 3rd, 7th, and 14th POD. Significant higher levels of CK were recorded only at 1ST POD with MIS-LA. However, there were no notable differences concerning functional outcome and measured VAS pain [48].
The same year, Muller et al. (2011) in their RCT compared minimally invasive anterolateral (MIS-AL) Versus modified direct lateral approach (M-LA). They studied soft tissue damage using myoglobin and CK postoperatively at 6 hours, 1st and 4th POD and performing MRI at 3 months and 1 year postoperatively. At 6 hour and 1st POD CK levels were higher with M-LA. MRI revealed greater abductor muscle and tendon damage in M-LA. The authors inferred that MIS-AL approach exhibited less obvious soft tissue impairment [20].
Matziolis et al. (2011) underlined the superiority of minimally invasive anterolateral (MIS-AL) compared to minimally invasive transgluteal (MIS-TG) approach. Researchers measured skeletal troponin I (sTnI) as a specific and susceptible serum marker for muscle damage and recorded distinct lower levels with MIS-AL approach at 1st POD. Although there were no notable differences in terms of hospitalization, blood loss and complications, the authors emphasized the restriction of muscle interference using AL approach [49].
4.3.2. No Difference in Biomarkers
On the contrary, Landgraeber et al. (2013) in their RCT reported no statistically significant differences postoperatively concerning CRP and CK levels, functional outcomes and perceived pain between minimally invasive anterolateral (MISAL) and conventional lateral (LA). Furthermore, the MIS approach was associated with greater blood loss and longer operative time. The authors indicated the experience of surgeons and predilection for each approach, as the most contributory factors for the success of the operation [50].
4.4. Posterior Approach Versus Minimally Invasive Posterior Approach
4.4.1. Difference in Biomarkers
Suzuki et al (2004) conducted a comparative study between conventional posterolateral (PLA) and minimally invasive posterolateral (MIS-PLA). CRP, ESR were evaluated at 1st and 2nd postoperative week and CPK at 1st POD, 1st and 2nd postoperative week. CRP and ESR levels were significantly lower at 1st week in the MIS group. However, CPK did not indicate important differences between the two groups. Concerning other postoperative data, MIS approach was associated with significantly shorter operative time, lower blood loss and fewer days of hospitalization. In terms of functional outcomes, the Japanese Orthopaedic Association score (JOA) revealed similar results [51].
In 2014, Kwak et al. (2014) compared the conventional posterolateral (PLA) (15 cm incision length) to a minimally invasive posterolateral (MIS-PLA) (7-8 cm incision length). To examine soft tissue damage, they used CK and aldolase serum markers and IL-1, IL-6, IL-8, IL-10 cytokines at 1st, 3rd, 7th and 14th POD. The results showed that during the proximate postoperative period (1st and 3rd POD) MIS approach was related to significantly lower levels regarding all markers. In addition, the mean blood loss was statistically higher in patients undergoing PLA. The authors summarized that MIS approach provokes less impairment in soft tissue and restricts systematic inflammation after surgery [40].
4.4.2. No Difference in Biomarkers
On the contrary, Fink et al. (2010) in their prospective study compared conventional posterolateral (PLA) and minimal invasive posterolateral (MIS-PLA) approaches. CPK, CK-MM, and myoglobin were recorded on the 1st and 2nd POD and CRP was measured on the 3rd POD. Conversely to the previous study, serum markers did not indicate a meaningful difference in muscle and soft tissue injury between the two groups. Yet, MIS approach was related to lower levels of perceived pain at rest, lower levels of total blood loss and shorter required period of hospitalization [52].
4.5. Lateral Approach Versus Minimally Invasive Lateral Approach
We found only two studies, comparing the standard lateral (LA) with the minimally invasive lateral approach (MIS-LA).
Mazoochian et al. (2009) measured CK and myoglobin laboratory data 6 hours after surgery, at 1st POD and at 2nd POD, in patients treated with standard lateral (LA) or minimally invasive lateral (modified Hardinge) approach (MISLA). The results showed statistically notable lower myoglobin levels only at 6 h postoperatively with MIS-LA approach. Furthermore, MISLA approach was associated with shorter operating time, less blood loss and better functional results (HHS and WOMAC score) on the day of discharge, 6 weeks and 3 months postoperatively [53]. In 2014 Dienstknecht et al. (2014) compared muscle damage between conventional lateral, transgluteal approach (Bauer) (LA) and mini-incision (MIS-LA) approach with CRP and CK markers. Serum markers were measured at 2nd and 7th POD. No statistically important differences were observed regarding serum markers. Yet, discernibly lower levels of VAS for pain were observed in the first 6 POD with the MI approach [54].
4.6. Standard Lateral and Postero-lateral Versus Minimally Invasive Lateral and Posterolateral
In 2009, Shitama et al. (2009) conducted an RCT of 62 THA. All operations were performed with either lateral or postero-lateral approach and divided into conventional lateral (LA) and posterolateral (PLA) and minimal invasive lateral (MIS-LA) and posterolateral (MIS-PLA) groups. CRP and IL-6 serum markers were recorded preoperatively and the 1st POD. After the assessment of the results, no statistically noteworthy discrepancies were found in soft tissue damage and functional postoperative outcomes. The researchers concluded that the mean longer incision length with standard approaches did not deteriorate postoperatively clinical results [55].
Proportionate results were detected later by Goosen et al. (2011) in their double-blind RCT. They allocated 120 patients into MIS and standard groups, using PLA and AL approach. CK and myoglobin levels were equal before and after surgery in both classes. Similarly, there were no statistically significant differences in terms of blood loss, complications and implant positioning. Regarding functional outcomes, patients undergoing MIS approaches had only significantly better HHS at 6 weeks postoperatively [56].
4.7. Three Minimal Invasive Approaches
Finally, Cohen et al. (2009) conducted a study comparing three MIS approaches; a modified Watson Jones, minimal invasive posterior (MIS-I) and minimally invasive two-incision (MIS-II) approach. They measured CK, CPK and myoglobin preoperatively and at 1st h, 8th h, 16th h, 1st POD, 36th h, 2nd POD and 3rd POD postoperatively. The authors came to the conclusion that the fluctuation of serum markers levels did not differ significantly between the approaches and proposed that no approach has an important advantage [57].
5. DISCUSSION
Total hip arthroplasty (THA) has become one of the most successful orthopedic operations. Several approaches to hip joint for primary THA are applied, either conventional approaches (anterior, anterolateral, lateral, posterior) or minimally invasive approaches (MIS modifications of classical approaches or new MIS approaches) are favorable in modern THA. Proponents of these approaches point out that they are designed according to the concept of better postoperative functional outcomes, smaller incision length and less invasiveness. On the other hand, opponents of MIS approaches argue that this term has not been sufficiently clarified, because the evaluations of postoperative results are biased by patient selection, surgeon’s preference and experience and the measurement of different functional protocols. Therefore, MIS term has become known prevalently not for its essential advantages but for marketing reasons. Another objection is that sometimes MIS approaches are correlated with worse perioperative and postoperative data (e.g. longer operative time, larger levels of blood loss or other complications) especially during the learning curve. Consequently, researchers have not met the consensus yet, which is the exact term of MIS approach and which approach confers the best postoperative results. Finally, the choice of the approach used touches on the preference and the experience of every surgeon.
Regarding the evaluation of muscle damage, several methods have been described such as the measurement of serum and inflammatory markers, Magnetic Resonance Imaging and surgical techniques in cadaveric studies. Specifically, considering the currently available literature, which is incorporated in our review, we cannot strongly support the superiority of any approach. However, in most studies, MIS approaches are related to lower levels of muscle damage serum markers. Another objective of our review is to correlate other perioperative and postoperative factors and results (e.g. postoperative pain, blood loss, functional outcome, operative time and other data) with the application of each approach.
As stated above, the anterior approach is probably the most studied approach. In our review, eight studies evaluated anterior or MIS anterior approaches. In five studies [19, 41, 42, 44, 45], anterior approach was correlated with lower levels of serum markers compared to posterior approaches or lateral approaches. From these studies, only one reported shorter operative time using DAA [19]. Two studies estimated longer operative time with DAA [41, 45], one study reported no significant differences between the approaches [44] and one study did not assess the operating time [42]. No study recorded statistically significant discrepancies in blood loss or transfusion requirements. Regarding postoperative functional outcomes, two studies referred to better results. The first study [41] reported better Harris Hip Score (HHS) and University of California Los Angeles activity score (UCLA) three months postoperatively. The second study [42] registered more steps in the immediate postoperative days in hospital for patients who underwent DAA. Moreover, two studies correlated lower levels of perceived (VAS) pain with patients who underwent DAA [42, 45]. Three studies measured implant positioning [19, 41, 45]. Zhao et al. found that DAA approach was related to the smaller fluctuation of cup inclination and anteversion. Nistor et al. found greater cup abduction in LA approach group. Bergin et al. measured no considerable differences. Only one study [44] evaluated MRI findings postoperatively and compared them with muscle damage according to serum markers. Statistically significant discrepancies were observed because lateral approach caused important fatty atrophy in all gluteal muscles and thickness of tensor fasciae latae muscle contrasting with DAA. These results coincided with the estimated lower levels of serum markers of DAA postoperatively. Finally, no studies registered notable differences in regards to postoperative complications.
On the other hand, two studies [37, 43] found no considerable differences in serum markers between anterior and posterior approaches. Contrary to their expectations, Pilot P et al. (2006) and colleagues noticed equivalent muscle damage due to serum maker in both approaches, more required operating time and relatively higher blood loss postoperatively when using MIS anterior approach. Similar outcomes were recorded by Rykov et al. (2017), as DAA was associated with longer operative time and slightly higher rates of blood loss. Lastly, no considerable differences were recorded in terms of complications.
Merely one study [46] reported higher CK levels at 4th POD using the anterior approach compared to the lateral approach. Furthermore, the duration of surgery was longer with MIDA. Conversely, the perceived pain was significantly lower at all POD.
MIS anterolateral approach was evaluated in six studies. In four studies, [47, 48, 20, 49] MIS-AL was associated with less invasiveness according to serum markers compared to MIS LA, AL approach with anterior hemimyotomy (AL-HM), MIS transgluteal (TG) or modified DLA. All these studies observed imperceptible differences regarding blood loss and postoperative complications between the approaches. One study recorded significantly longer operative duration approach and perceived pain using MIS-AL [47]. The same researchers also found better functional scores six weeks postoperatively with MIS AL. In addition, Michael Muller et al. 2011 found in their follow-up examination significantly higher rates of negative Trendelenburg sign 1 year after surgery in patients undergoing ALMI. Three studies [47-49] dealt with implant positioning through radiographic evaluation and only one revealed higher fluctuation in cup inclination with MIS AL [49].
Conversely, in two studies [50, 57] no significant differences were observed in muscle damage contrasting with MIS posterior and MIS two incision or conventional lateral (LA) approaches. Cohen et al recorded shorter operative time and lower rates of blood loss at MIS-AL group. Quaintly, Landgraeber et al estimated longer duration of surgery and higher levels of blood loss in MIS-AL group.
Three studies dealt with the comparison between standard posterior and MIS posterior approaches. Two studies [40, 51] ratified the eminence of the MIS technique, but one study [52] did not come up with significant differences in serum markers. All three studies punctuated the predominance of MIS approach. Specifically, the MIS technique was correlated with lower levels of blood loss in all studies. Two studies [51, 52] showed less required duration of hospitalization for the patients who had undergone MIS approach. Suzuki et al recorded less operative time for MIS approach and finally, Fink et al estimated less perceived pain.
Moreover, from the two studies comparing conventional lateral approach and MIS lateral approach, one underlined the efficacy of MIS method [53], but the other study [54] deduced that both approaches cause similar muscle damage. Yet, both studies underlined the superiority of MIS LA approach. Mazoochian et al demonstrated the advantages of MIS method in terms of shorter operating time, lower blood loss and better functional results (HHS and WOMAC) 6 weeks and 3 months postoperatively. On the other hand, Dienstknecht et al registered lower rates of VAS pain and shorter required surgical time in the MIS group.
Finally, two studies compared simultaneously conventional lateral (LA) or postero-lateral (PLA) approaches with minimal invasive lateral (MIS-LA) and posterolateral (MIS-PLA). The results did not demonstrate significant differences in serum markers [55, 56]. Both studies calculated longer operative time in MIS groups. Concerning the other perioperative and postoperative data, there were no statistically significant differences.
Despite the useful details which emerged from our review, we can nevertheless elucidate that there are some limitations to our article. Concerning our research, we included only the Pubmed database in the English language. On the other hand, some of the included studies had methodological limitations and they are susceptible to bias. These limitations are the comparison of unequal samples and unprivileged rando- mization. Specifically, some researchers choose their patients according to specific criteria in order to promote an approach. For example, in some studies patients with high body mass index (BMI) do not undergo THA with the anterior approach. Therefore, the anterior approach is correlated with less invasiveness and better postoperative outcomes compared with other approaches without sufficient evidence. In addition, most studies do not cope with bone impairment during implant positioning and to what extent this process influences the postoperative inflammation. Furthermore, the methodology of each of the included studies incorporated the assessment of different serum markers in different time periods. Consequently, no markers were found with a distinct specification in muscle damage. Moreover, some studies did not correlate muscle damage and other postoperative outcomes in order to optimize the efficiency of the approaches. Finally, there is still a lot of disagreement over the highly contentious issue of postoperative functional protocols. Some researchers use predefined protocols which are not consolidated and culminate in eventual better results for specific approaches.
At this point, we must underline that the efficacy of any approach is not based mainly on the measurement of muscle damage and its intervention. The contributing factors that seem to have great importance are the improved postoperative functional outcomes, the small levels of perceived pain and the patient’s satisfaction. Because a great deal of controversy surrounds the performance of MIS approaches or conventional muscle-sparing approaches, we should point out that the experience and the training of every surgeon constitute the most significant factors for the success of THA.
CONCLUSION
THA has proved a very successful operation, which enables patients to enhance their motility and subsequently their life’s quality. MIS approaches in primary THA have gained ground in the last decades regarding the conception of respect of soft tissue, restricted blood loss, limited perceived pain and rapid recovery. In our review, we focused on investigating which approach is more efficient in terms of reducing muscle and soft tissue damage as is expressed by serum markers. It seems that MIS approaches were related in most of the studies with a lower level of inflammation markers contrasting with conventional approaches. Yet, the existing literature did not lead to a safe consensus about the superiority of any approach. Consequently, further research based on large well-designed studies is required in order to further explicate the efficacy and safety of MIS approaches.
DISCLOSURE
The authors and their immediate families did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.








