REVIEW ARTICLE
Current Concepts in Paediatric Femoral Shaft Fractures
Rakesh John1, Siddhartha Sharma1, *, Gopinathan Nirmal Raj1, Jujhar Singh1, Varsha C.2, Arjun RHH1, Ankit Khurana1
Article Information
Identifiers and Pagination:
Year: 2017Volume: 11
Issue: Suppl 2: M4
First Page: 353
Last Page: 368
Publisher ID: TOORTHJ-11-353
DOI: 10.2174/1874325001711010353
Article History:
Received Date: 03/02/2016Revision Received Date: 09/07/2016
Acceptance Date: 15/07/2016
Electronic publication date: 28/04/2017
Collection year: 2017

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Pediatric femoral shaft fractures account for less than 2% of all fractures in children. However, these are the most common pediatric fractures necessitating hospitalization and are associated with prolonged hospital stay, prolonged immobilization and impose a significant burden on the healthcare system as well as caregivers. In this paper, the authors present a comprehensive review of epidemiology, aetiology, classification and managemement options of pediatric femoral shaft fractures.
INTRODUCTION
Pediatric femoral shaft fractures are uncommon, constituting less than 2% of all fractures in children; yet they are a significant burden on healthcare systems and families as they are the most common fractures requiring hospitalization in children [1, 2]. These injuries often require prolonged immobilisation or surgery [1]. This review will look at the epidemiology, classification and current concepts in the management of pediatric femoral shaft fractures.
EPIDEMIOLOGY
Pediatric shaft femur fractures are 2.6 times more common in boys than in girls [3-5]. A bimodal distribution has been noted, with the first peak occurring in the age group of 1-3 years (usually low energy) and the second peak during early adolescence period (high energy), which constitutes the majority of the fractures [3, 5]. Although, the etiology of the fracture varies with the age of the child, the most common cause of femur shaft fractures in children is fall from height and road traffic accidents [4, 6]. However, one should keep the suspicion of child abuse in mind while dealing with these fractures in young children as it has been observed that up to 80% of femur shaft fractures occurring in children before walking age are due to abuse [7, 8]. Coffey et al. [9] reported that 67% of lower limb fractures in children less than 18 months of age were as a result of child abuse. In children more than 3 years of age, abuse is unlikely to cause femur fractures since bone at this age is significantly stronger in resisting both torque forces and direct blows [4, 6].
Stress fractures of the femoral shaft and neck, although uncommon, are increasingly being noticed in adolescent athletes participating in soccer, basketball, athletics etc. and account for 4% of all stress fractures in children [10-12]. A high index of suspicion is needed to diagnose undisplaced stress fractures in order to prevent their eventual progression to a displaced fracture [10-12].
CLASSIFICATION
There is no universal classification system available for pediatric shaft femur fractures. Fractures are usually classified descriptively either on the basis of i) configuration - transverse/spiral/oblique ii) comminution - comminuted or non-comminuted and iii) presence/absence of soft tissue coverage around fracture- open/closed. The most common type of fracture is a simple, transverse, non-comminuted, diaphyseal fracture accounting for more than 50% of the cases [1].
According to the AO (Arbeitsgemeineschaft fur Osteosynthesefragen) paediatric comprehensive classification of long bone fractures, shaft femur fractures are classified as category 32-D [13]. Sub-categories 32- D 4.1 (complete transverse with an obliquity of 30º or less) and 32-D 5.1 (complete oblique or spiral more than 300) are simple fractures whereas subcategories 32-D 4.2 (multi-fragmentary transverse 300 or less) and 32-D 5.2 (multi-fragmentary oblique or spiral more than 300) are unstable patterns [13].
MANAGEMENT
Pediatric femur shaft fractures tend to unite rapidly and have a tremendous remodelling potential. Consequently, a wide range of deformity of the initial healed bone is considered acceptable. The acceptable angulation in the coronal and sagittal planes varies from 300 at birth to 150 at 10 years. Rotational malalignment does not remodel and deformity more than 100 in the axial plane is not acceptable [14]. Limb shortening of up to 15 mm can be compensated in children up to 12 years of age by growth acceleration [15].
The decision to manage a femoral shaft fracture by conservative or operative means is affected by a wide number of variables, which include age and weight of patient, the type of fracture, associated injuries/polytrauma and socioeconomic status of the family [16].
Age is the main predictor of the treatment (Table 1). Fractures in children below 6 years of age are usually managed non-operatively due to the excellent remodelling potential of this age group. Various conservative modalities used include Pavlik harness, traction (Bryant’s traction, skin traction and skeletal traction), hip spica and functional bracing. Immobilization in a Pavlik harness works well for infants up to 6 months of age whereas hip spica is preferred for older children [16].
The treatment of fractures in the age group 5-16 years is controversial with multiple options available and no clear consensus on the preferred modality of management. Surgical options are external fixation, plating (conventional and submuscular bridge plating) and intramedullary nails which can be by flexible nails (titanium nail, Enders nail) or rigid nails [16]. The different treatment options are discussed at length.
| Age of child | Preferred management | Other modalities |
|---|---|---|
| 0-6 months | Pavlik harness | Hip spica |
| 6 months to 2 years | Hip spica | Traction followed by spica |
| 3-5 years | Hip spica | Traction followed by spica/orthosis External fixation (Rare) Flexible intramedullary nails (Rare) |
| 6-11 years | Flexible intramedullary nails | Traction followed by spica External fixation Submuscular plating |
| More than 12 years | Rigid intramedullary nails (Trochanteric entry) | Flexible intramedullary nails External fixation Submuscular plating |
CONSERVATIVE MANAGEMENT
i). Pavlik Harness
This orthosis is ideal for birth injuries with proximal or mid-shaft fractures in infants.1Both stable and unstable fractures can be managed using a Pavlik Harness and a wrap on around the thigh. The proximal fragment lies in flexion due to the pull of the iliopsoas; when the Pavlik harness is applied in moderate flexion and abduction, the distal fragment automatically aligns itself to the proximal fragment [1].
The use of Pavlik harness in infants with femur fractures was popularised by Stannard et al. [17] who noted acceptable alignment in all patients with less than 1cm shortening. Podezwa et al. [18] compared hip spica application to Pavlik harness application in children less than 1 year of age in a retrospective study. There was no difference in the radiological outcomes in both the groups. They noted that infants treated with spica cast had lower pain scores compared to those treated with Pavlik harness; however, one-third of the patients on hip spicas had skin complications whereas none of those treated with Pavlik harness reported skin complications. Based on the observations of Podezwa et al. [18], Pavlik harness application is now the recommended treatment for shaft femur fractures in children less than 1 year of age.
ii). Hip Spica Casting (Table 2)
In children 1-6 years of age, hip spica casting has traditionally been the treatment of choice unless there are associated injuries, excessive shortening (>2cm), skin complications which can preclude application of hip spica [19, 20].
Based on the timing of application of the spica, hip spicas have been arbitrarily classified into “immediate” and “early” spicas. When the spica is applied within minutes of presentation to the clinic, it is called “immediate spica casting” whereas when the spica is applied a few days after the injury, it is termed as “early spica casting”.
The ideal position for hip spica application has always been controversial. Numerous studies have reported excellent outcomes for ‘one and a half’ hip spica casting in the 90-90 position/ “sitting spica cast” (i.e both hips and knees in 900 of flexion) [21, 22]. Casting in the 90/90 position permits the child to be placed on a chair or to be easily carried in the lap of the parents and also obliterates the need of bedpans for toiletries [1]. It has also been observed that knee flexion greater than 600 improves maintenance of length and reduction [23]. However, Frick et al. [24] observed that excessive traction with increased knee flexion increases the chances of compartment syndrome and skin sloughing. The position of the knee (lesser than 900 flexion), lesser traction and cast padding are critical to avoid this complication.1 According to a recent Cochrane review, the safe and effective position is 300 of abduction, 300 to 400 of flexion and external rotation at the hip [25]. The fracture location may also the dictate the amount of flexion needed at hip with more proximally located fractures needing more amount of flexion [20]. All patients should be observed for 24 hours after hip spica application to rule out neurovascular compromise and compartment syndrome [1].
Advantages of spica are excellent union rates, low cost, good safety profile, reduced need of specialised surgical instrumentation/tools and low rate of complications like limb length discrepancy, non-union etc [26, 27]. The complications associated with spica casting are maintenance of personal hygiene, transportation difficulties and intolerance of the child to cast [28]. It has been noted that the negative impact of spica casting is more on school going children (i.e. children more than 5 years of age) than in pre-school children [29].
iii). Walking Spica/Single Leg Hip Spica
Of late, there has been a renewed interest in the concept of “walking spica” or “single-leg hip spica” for selected indications. The walking spica is ideal in stable, low energy fractures in toddlers [30, 31]. It is applied with the ipsilateral knee in 450 of flexion and the hip in 450 of flexion and 150 of external rotation. The hip should be extensively reinforced anteriorly to avoid breakage. Additional advantages offered by walking spica over conventional hip spica are improved function and care and reduced chances of spica syndrome [30-35]. The disadvantage is the increased chance of loss of reduction compared to conventional spica [30, 32].
Epps et al. [32] reported that 90% children pulled to stand and 62% children walked independently by the end of the treatment with minimal complications. However, Flynn et al. in a comparative study noted that outcomes of children treated with walking and conventional spica were similar [30].
Leu et al. [31] too did not find a significant difference in radiological and functional outcomes between single leg and double leg spica casts at cast removal (mean 44 days in both groups). They observed that single-leg casts afforded more comfort during sitting and greater ease on leaving the family home. Fewer caregivers needed to take time off work in the single-cast group and for lesser time duration.
| Authors | Year | Study design | No. of fractures | Treatment | Results & complications | Remarks |
|---|---|---|---|---|---|---|
| Cassinelli et al. [33] | 2005 | Retrospective review | 145 | Immediate spica | Acceptable alignment in all patients. Low complication rate |
Immediate spica is a safe procedure |
| Illgen et al. [23] | 1998 | Retrospective review | 114 | Early spica | Successful in 86% patients | Procedure of choice <6 years |
| Czertak and Hennrikus et al. [34] | 1999 | Retrospective study | 23 | Early Spica | Average no. of days in cast 42 Mean shortening at cast removal 1 cm |
Procedure of choice <6 years |
| Epps et al. [32] | 2006 | Retrospective review | 45 | Single-leg spica cast | Failures (2) Repeat casting (2) Rotational malunion (1) No radiographic malunions |
Recommended in low energy fractures in young children |
| Flynn et al. [30] | 2011 | Prospective study | 45 | Traditional spica v/s “walking” spica | Similar outcomes in both More chances of wedge readjustment in walking spica |
Less burden of care on family in walking spica |
| Leu et al. [31] | 2012 | RCT | 52 | Single leg spica v/s double leg spica | Similar functional and radiological outcomes in both groups. Single-leg spica group was more likely to fit into car seats and chairs comfortably. Caregivers took less time off work. |
Single leg spica is effective and safe. |
iv). Traction Followed by Casting/ Functional Orthosis
The eponymous Bryant’s traction was introduced by Bryant in 1873, wherein vertical overhead traction was applied with both hips in 90o flexion and knees in full extension [36, 37]. Due to ensuing vascular complications in few patients, this method went out of vogue [38]. Modified Bryant’s traction was described by Ferry et al., [39] in 1966; knees were placed in 45o of flexion, which reduced vascular complications.
Application of traction before spica casting/functional bracing is indicated in length unstable fractures provided the family members agree to the long period of immobilisation.1 The Thompson’s telescope test can be used to detect length unstable fractures [40]. At the time of hip spica application, if > 3 cm shortening is demonstrable with gentle axial compression under fluoroscopic imaging, then the fracture is length unstable and traction should be used [40]. Both skin and skeletal traction can be applied, depending on the weight of the child. Skeletal traction is ideally used when > 5 lb of traction is needed [41]. The preferred choice of site for application of traction pin is the distal femur as proximal tibial pins have been known to cause recurvatum deformity subsequent to proximal tibial physeal plate damage and may also aggravate associated menisco-ligamentous injuries of the knee by over-distracting the knee joint [41-43].
SURGICAL MANAGEMENT
i). External Fixation (Table 3)
It is the recommended mode of treatment when fracture femur is associated with severe soft tissue injury, head injury and/or polytrauma (damage control orthopaedics) or when the fracture is pathological in nature (Fig. 1) [1, 44].
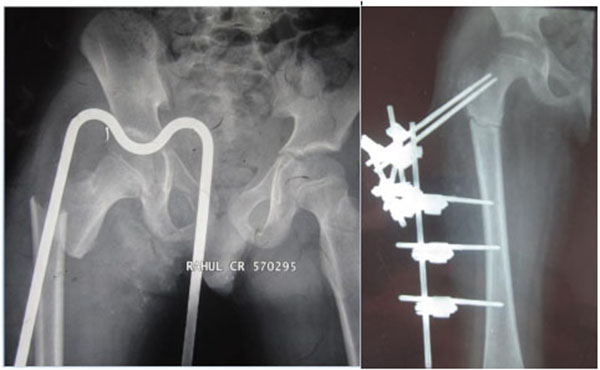 |
Fig. (1). Preoperative and post operative images of an open subtrochanteric femur fracture in a 7 year old male managed by external fixator. |
External fixator application is associated with complications manifold [45-48]. The main complication is pin tract infection which can occur in up to 72% of patients [45]. Other complications are secondary fractures after implant removal with an incidence ranging from 1% to 22% [45-49]. This means that the fixator should be left in situ for a long period of time until bridging callus is seen in atleast 3 cortices in 2 orthogonal radiological views. They are difficult to use in proximal/distal fractures due to difficulty in placement in the physeal regions. Hip or knee joint stiffness may develop when major soft tissue injuries are present [46].
Fixator removal is usually done after 3-4 months when bridging callus is noted in at least 3 of the 4 cortices on AP and lateral views. An alternative strategy (“portable traction”) is to remove fixator at around 6-8 weeks when early callus is noted and to apply a walking spica. This method minimises stress shielding and allows pin tracts to ossify with the spica acting as a protective splint [1].
| Authors | Year | Study design | No. of fractures | Treatment | Results & complications | Remarks |
|---|---|---|---|---|---|---|
| Aronson et al. [50] | 1992 | Retrospective review | 44 | Primary external fixation | 10% re-application or casting 8.5% pin tract infection |
Recommended Primary EF use. |
| Matzkin et al. [51] | 2006 | Retrospective review | 40 | External fixation f/b dynamization | Refractures rate 2.5% 100% union rate in those with cortical contact (25) 72.5% EF dynamized prior to EF removal |
Pin tract infections common (52.5%) |
| Bar-on et al. [52] | 1997 | RCT | 20 | External fixation v/s flexible nails | Early post-op course similar More callus, faster union, shorter recovery time, better muscle strength in nailing group |
EF recommended only for open/severely comminuted fractures Flexible nail use recommended |
| Kapukaya et al. [53] | 1998 | Retrospective review | 57 | EF in closed femur fractures | Low complication rates Pin tract infection (3) Refractures (1) |
Recommended EF use |
| Davis et al. [54] | 1995 | Retrospective review | 15 | Orthofix EF | 100% fracture union Pin tract infection (5) Refractures (1) |
Recommended EF use |
| Hedin et al. [48] | 2004 | Prospective study | 98 | External fixator | 59 cases of LLD, 35 pin tract infections and 2 re-fractures | Recommended EF use |
| Sola et al. [55] | 1999 | Retrospective study | 39 | Orthofix EF | Auxiliary pin used in 16 cases | Use of auxiliary pin reduced malunion and re-manipulation rates. |
| Domb et al. [56] | 2002 | RCT | 53 | Static v/s dynamic EF | Similar results in both groups | No effect of dynamization on union time and complication rate |
| Gregory et al. [47] | 1996 | Retrospective study | 27 | EF | 8 major complications in 6 patients 29 minor complications in 20 patients |
Careful attention to operative technique and post-operative care needed |
| Barlas et al. [57] | 2006 | Prospective study | 40 | EF v/s flexible IM nails | More complications with EF: Pain (3) LLD (2) Malalignment (4) No complications in nailing group |
Flexible nail use recommended. EF recommended only for open/severely comminuted fractures. |
ii). Intra-Medullary Nailing
Elastic Stable Intramedullary Nails (Esin) (Table 4)
Developed by the Nancy group in France [58, 59] in the early 1980’s, this is the most popular method of fracture fixation in the age group of 5-11 years as fractures tend to angulate and/or shorten with spicas due to the bulkier frame. Flexible intramedullary nails are load sharing devices which offer good fixation (relative stability and subsequent fracture union by indirect bone healing/callus formation), are relatively cheaper and have a short learning curve as it is relatively easier to insert and remove these nails [60]. Bone growth is affected minimally, as the need to cross physis can be avoided with these nails; the mean femur overgrowth is 1.2 mm. Operating time and blood loss is significantly reduced [60, 61].
The preferred technique for insertion of these nails is a retrograde technique with 2 small incisions (medial and lateral) just above the distal femoral physis (Fig. 2) [1]. Antegrade nailing from the subtrochanteric area avoids post-operative knee complications [62]. The diameter of the nail should be two-fifths of the diameter of the medullary canal and should be calculated preoperatively [1]. During insertion, it is important to prebend the nails so that the apex of the bend lies across the fracture site [59, 60, 63]. The elastic deformation of the pre-bent nail in a straight medullary canal imparts a bending moment which tends to angulate the fracture. The insertion of another nail of the same diameter from the opposite side balances this moment leading to good stability against bending and torsional forces. This principle is referred to as ‘trifocal buttressing’ [59, 60, 63]. Frick et al. [64] observed that retrograde double C configuration is better than antegrade C or S pattern as it offers greater resistance to torsional forces.
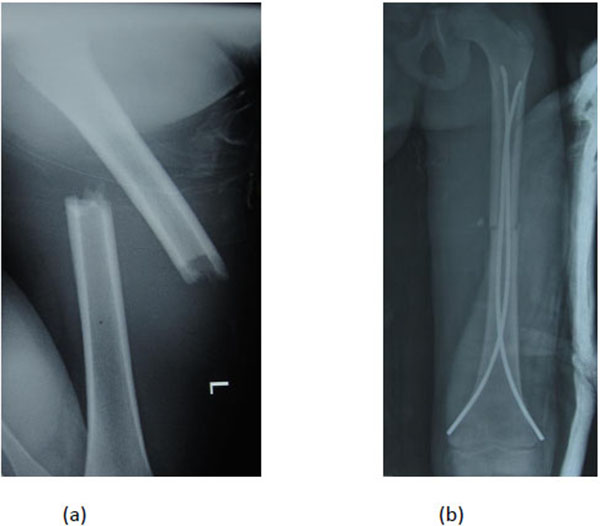 |
Fig. (2). Preoperative and postoperative images of a femoral shaft fracture in a 6 year old girl treated by retrograde elastic stable intramedullary nailing. |
Complications include excessive shortening which leads to nail protrusion and limb length discrepancy. The most common complication is pain or skin irritation at the nail insertion site caused by a prominent nail end [63, 66]. Higher rate of unplanned surgeries and malunions have been observed in length unstable fractures and heavy (>50 kg) children [63, 65-67].
• Antegrade vs retrograde insertion of flexible nails
Frick et al. [64] conducted a biomechanical study to evaluate the stability of simulated transverse and comminuted femoral fractures after retrograde and antegrade flexible nail insertion in five synthetic adolescent-sized femoral bone models each respectively. They noted that retrograde nail fixation demonstrated significantly less axial range of motion and greater torsional stiffness than antegrade fixation in both fracture patterns. However, antegrade nails demonstrated greater resistance to shortening [64].
Mehlman et al. [68] conducted a mechanical study to determine whether the stability of ESIN constructs differ in terms of antegrade versus retrograde insertion for the fixation of pediatric distal-third transverse femoral-shaft fractures in 10 synthetic composite adolescent-sized femur models. All the specimens were subjected to 4-point bending followed by axial torsion. They observed that flexural stiffness was significantly greater in the retrograde group (350±72 N/mm) compared with antegrade (195±95 N/mm; p = 0.02). Although antegrade nail insertion is recommended for distal-third femur fractures, Mehlman et al. demonstrated that given satisfactory cortical starting points in the distal fragment, retrograde insertion provides greater stability [68].
• Steel vs titanium flexible nails
Wall et al. [69] compared stainless steel to titanium elastic nails and found that the cheaper stainless steel nails were superior to titanium nails owing to a lesser rate of malunion (6.3% vs. 23.2%). However, in an experimental study by Perez et al. [70] it was noted that stainless steel nails were associated with increased gap closure and nail slippage; titanium nails, on the other hand, offered greater stability. It was also observed that stainless steel nails hamper re-modelling and consequently increased the chances of re-fracture [71].
• Flexible interlocked nailing
Linhart and Roposch [71] described a method of “locking” flexible Enders rods to maintain leg length and alignment without compromising early postoperative mobility. Cramer et al. [72] reported a different locking technique and reported no clinically significant malunions, motion loss, or leg length discrepancy. They recommended Enders nail over TENS system due to the locking capability of Enders nails although they are limited by the canal size [73].
Ellis et al. [73] conducted a retrospective review to study locked versus unlocked Ender’s nails in length unstable femur shaft fractures (defined as either a comminuted fracture or a spiral fracture longer than twice the diameter of the femoral shaft). They identified a total of 107 length unstable fractures fixed with Enders nails, of which 37 cases had both Enders rods “locked” through the eyelet in the distal femur with a 2.7mm fully threaded cortical screw. They observed that shortening of the femur and nail migration at 1-6 weeks post-operatively was significantly greater in the non-locked nails group. Also, there were significantly more clinical complaints in non-locked group including limp, clinical shortening, and painful, palpable rods. Based on these observations, they concluded that locked Enders rods are an excellent option to prevent shortening in length unstable fractures and result in no additional complications or added surgical time or increased blood loss [73].
| Authors | Year | Study design | Mean age | No. of patients | Treatment | Results & complications | Remarks |
|---|---|---|---|---|---|---|---|
| Flynn et al. [60] | 2001 | Prospective Review | 10.2 | 58 | ESIN | Excellent/ satisfactory outcome in 57 of the 58 cases | TENS may be an ideal implant to stabilize paediatric femur fractures. |
| Aktekin et al. [74] | 2007 | Prospective Study | 9.6 | 21 | ESIN | Mean time to union 13 weeks No malunion. |
ESIN is treatment of choice in 6-12 year age group. |
| Carey et al. [75] | 1996 | Retrospective review | 12.5 | 25 | Antegrade flexible nails | No non-union/malunion | Treatment of choice in 6-12 years age group |
| Singh et al. [76] | 2006 | Prospective study | 11.26 | 35 | ESIN (retrograde) |
100% union rate Mean time to union 9.6 weeks. |
Ideal implant for pediatric femur fractures |
| Li Y et al. [77] | 2008 | Experimental study | - | - | ESIN | Obese children undergoing stabilization of mid-shaft femur fracture with TENS are at risk for loss of reduction. | - |
| Saikia et al. [78] | 2007 | Prospective study | 10.8 | 22 | ESIN | 100% union rate Mean time to union 8.7 weeks |
Ideal implant for pediatric femur fractures |
| Narayana et al. [79] | 2004 | Retrospective study | 13.7 | 78 | ESIN | Proper nail advancement and fracture comminution are important factors regarding complications of ESIN | Ideal implant for pediatric femur fractures. Most complications are minor. |
| Sagan et al. [80] | 2010 | Retrospective review | 10.7 | 70 | ESIN | Anterior bowing greater than 15 degrees is the most common malunion noted with TENS. | Bowing may be reduced if at least 1 of the nails is inserted with the tip pointing in an anterior direction |
| Luhmann et al. [66] | 2003 | Prospective study | 6 | 39 | ESIN | Technical pitfalls with TENS can be minimized by leaving less than 2.5 cm of nail out of the femur and by using the largest nail sizes possible | Outcomes were associated with the patient's weight and size of the nails implanted |
| Reynolds et al. [81] | 2012 | Retrospective cohort study | 12.6 | 22 | Adolescent Lateral femoral (ALFN) nail Vs. ESIN |
Older, heavier pediatric patients treated with ALFNs had a shorter recovery time compared to ESIN group. |
Mean time to full weight-bearing significantly less for the ALFN group. However, the outcomes for both groups were satisfactory |
| Houshian et al. [82] | 2004 | Prospective review | 6 | 31 | ESIN | All fractures united at a median of 7 weeks. LLD was up to 1 cm in 6 children. | ESIN is a safe method for the treatment of femoral shaft fractures in children between 4-11 years |
| Anastasopoulos et al. [83] | 2010 | Retrospective study | 10.3 | 36 | ESIN | 50% children had a LLD without functional disability. No clinical mal-alignment observed. |
Flexible nailing of diaphyseal fractures of the femur is a reliable method; small learning curve; allows early mobilisation |
| Sink et al. [84] | 2005 | Retrospective review | 8.9 | 39 | ESIN (stable V/s unstable fracture pattern) | 62% complications recorded. 8 patients (21%) underwent unplanned surgery prior to complete fracture union | “Length-Unstable” femur fractures require methods of treatment other than TENS |
Rigid Intramedullary Nails (Table 5)
Rigid intramedullary nails initially fell out of favour compared to flexible intramedullary nails as these nails had a piriformis entry and hence were associated with avascular necrosis (AVN) of the femur head and with injuries to the growth plate leading to growth arrest [85]. However, with the introduction of trochanteric entry nails (Fig. 3), which has reduced the chances of osteonecrosis, the use of rigid intramedullary nails in adolescents is on the rise again [86, 87].
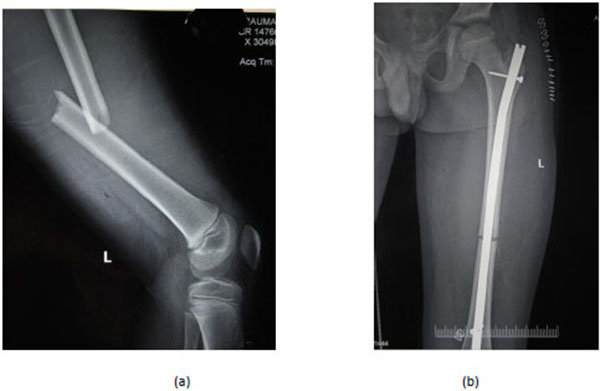 |
Fig. (3). Pre-operative and post-operative radiographs of an 11 year old male with femoral shaft fracture treated by a trochanteric entry rigid intramedullary nail. |
Current literature suggests that rigid intramedullary nail with a trochanteric entry point is the preferred mode of fixation of shaft femur fractures in adolescents [1]. However, growth disturbance due to physeal plate damage is still a concern with these nails and hence it is not preferred for use in children less than 12 years.
| Authors | Year | Study design | Mean age/Range | No. of patients | Treatment | Results and complications | Remarks |
|---|---|---|---|---|---|---|---|
| Reeves et al. [88] | 1990 | Retrospective Study | 13.9 | 90 | Traction + cast (41 patients) v/s Intramedullary nailing (49 patients) | The operative group had a mean hospital stay of 9 days vs 26 days for non-operative group and had fewer complications. | IM fixation better than conservative management |
| Kirby et al. [89] | 1981 | Retrospective Study | 11.6 | 25 | (Traction + cast) v/s Intramedullary nailing | IM fixation better than conservative management | |
| Beaty et al. [85] | 1994 | Prospective Study | 10-15 | 30 | IM nail | 100% fracture union. 1 case of asymptomatic AVN of femur head | IM nail reasonable alternative for the treatment of isolated femur shaft fractures in adolescents with polytrauma. |
| Momberger et al. [90] |
2000 | Prospective cohort study | 10-16 | 48 | IM nail | All fractures united. No significant deformity/shortening/malunions/ AVN. | IM nailing through trochanteric point is safe & effective for treating femur fractures in adolescents. |
| Kanellopoulos et al. [91] |
2006 | Prospective Study | 11-16 | 20 | IM nail | No major complications. All fractures healed within 9 weeks and patients returned to pre-injury activity level. | Excellent results with good surgical technique involving GT entry point. |
| Townsend & Hoffinger et al. [92] | 2000 | Retrospective Study | 12-17 | 34 | IM nail | No patient had AVN of the femoral head or other major complications. | The trochanteric tip entry point is recommended for IM nailing of femoral shaft fractures in children and adolescents. |
iii). Plate Fixation
Pediatric trauma surgeons have largely moved away from the traditional open reduction and compression plating to the more modern submuscular bridge plating which offers stability without disturbing the vascularity of the fracture fragments hence leading to early union.
SUBMUSCULAR BRIDGE PLATING (Table 6)
Submuscular bridge plating provides excellent stability; it is especially useful in the management of proximal/distal fractures that are not suitable for IM nailing/external fixation (Fig. 4) [93, 94]. This method can also be used in pathologic fractures and associated head injuries. Disadvantages are the difficulty in implant removal due to cold welding of locking screws to the plate, significant blood loss and relatively higher learning curve [93-100].
| Authors | Year | Study design | Mean age | No. of patients | Treatment | Results & complications | Remarks |
|---|---|---|---|---|---|---|---|
| Eidelman et al. [95] | 2010 | Retrospective Review | 8-16 | 11 | Submuscular plating | All fractures united in proper alignment without deformity. 1 patient had 2 cm shortening. No complication related to hardware failure | Submuscular plating of adolescent femoral fracture with precontoured plate is effective. |
| Sink et al. [96] | 2006 | Retrospective study | 27 | Submuscular Bridge Plating | 100% union rate. No intraoperative/postoperative complications | Reasonable option for operative stabilization of comminuted and unstable fractures. | |
| Agus et al. [98] | 2003 | Retrospective Study | 11.3 | 14 | Submuscular Bridge Plating | Mean healing time 12.4 weeks. Angulation >100 seen in 1 patient. |
Bridge plating is effective treatment method for the closed comminuted fractures of the proximal and distal thirds. |
| Hammad et al. [99] | 2008 | Retrospective study | 9.4 | 15 | Submuscular Bridge Plating | 100% union rate. Screw failure in form of bending or breakage occurred in 2 patients, without clinical consequences. Average femoral lengthening 2.3 mm in 6 patients and 2 mm tibial lengthening in 4 patients. | Reliable method for the treatment of femoral shaft fractures in skeletally immature patients. |
| Abdelgawad et al. [100] |
2013 | Retrospective Review | 9 | 58 | Submuscular Bridge Plating | All fractures healed well and all patients returned to full activity. 1 patient had implant failure and other, deep infection in an old open fracture. | Submuscular bridge plating is preferred method for unstable fractures or fractures of the proximal and distal shaft. |
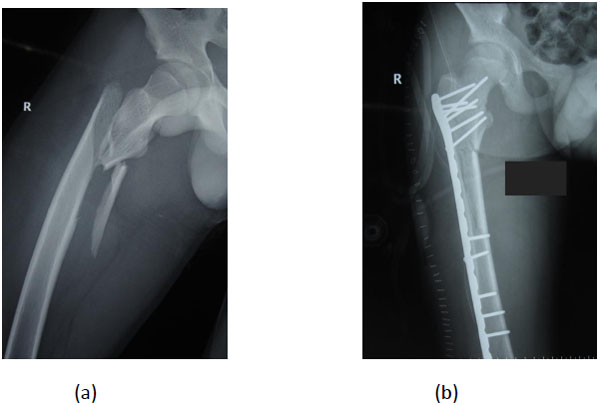 |
Fig. (4). Preoperative and post operative radiographs of a comminuted subtrochanteric fracture with extension into the femoral shaft managed by submuscular bridge plating. |
CONCLUSION
Femoral shaft fractures in children are amongst the commonest fractures necessitating hospitalization. The major determinant of treatment modality is age of the child. Fractures in children below 6 years of age can be managed non-operatively with excellent outcomes. Elastic stable intramedullary nails are preferred for children < 11 years of age or those with body weight < 50 kg with a length stable transverse or short oblique fracture. Length unstable fractures and fractures at the proximal ends of femur may be managed by submuscular plating or external fixation. For children above 11 years of age or those with body weight > 50 kg, rigid intramedullary nailing or submuscular plating is preferred. Piriformis fossa entry nails should be avoided to prevent the complication of avascular necrosis of femoral head.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
Declared none.
LIST OF ABBREVIATIONS
| ALFN | = Adolescent Lateral Femoral Nail |
| AVN | = Avascular Necrosis |
| EF | = External Fixator |
| ESIN | = Elastic Stable Intramedullary Nail |
| GT | = Greater Trochanter (of femur) |
| IM | = Intramedullary |








