All published articles of this journal are available on ScienceDirect.
Repair of Double Head Pectoralis Major Tendon Avulsion into its Native Footprint Using Bi-cortical EndoButtons and Tendon Sliding Technique
Abstract
Injuries to the pectoralis major muscle are relatively infrequent. The mechanism of injury is usually an eccentric shortening of the pectoralis major under heavy load, such as when performing a bench press exercise. We report a case that presented to us with a history of sudden pain in the left pectoral region while doing heavy bench press exercise. The patient sustained a type III D pectoralis muscle –tendon avulsion. Surgical repair was done through a bi-cortical tendon sliding technique using two cortical buttons. In this article we describe our modifications to the previously described surgical technique for the pectoralis major tendon repair using the EndoButton and tension – slide technique, aiming to overcome the possible complications.
INTRODUCTION
The pectoralis major is at risk of injury during any activity, in which the arm is extended and externally rotated, while under maximal contraction [1, 2]. Rupture is often followed by an audible pop, a tearing sensation, immediate pain and/or weakness [3-5]. By far, the single most common activity that has precipitated pectoralis major rupture is the bench press exercise [6].
Compared to the unicortical button technique, the existing Bi-cortical EndoButtons and tendon sliding technique has many drawbacks. Since two huge bicortical drill holes are made to incorporate the tendon into the bone tunnel, there is always a risk of stress riser and a secondary fracture at this site.
CASE REPORT
A 29-year-old, otherwise healthy male, presented with a history of sudden pain in the left pectoral region while doing a heavy bench press exercise. On examination, the deltopectoral region was swollen, tender, and bruised. Movement of the shoulder was reduced and associated with pain during adduction and forward flexion of the arm. Magnetic resonance imaging (MRI) scans were taken and showed a Tietjen Type III D, i.e. complete pectoralis major muscle tendon avulsion, which is the most common type of pectoralis major injury [7]. Two days later, the patient underwent surgical repair by a bi-cortical tendon sliding technique using two EndoButtons.
SURGICAL TECHNIQUE
The patient is positioned in a beach chair position and the arm is placed on a padded Tri-mano stand. We prefer this position, which allows for better control of the operative extremity and improved visualization. The arm is placed in slight forward flexion, abduction, and internal rotation.
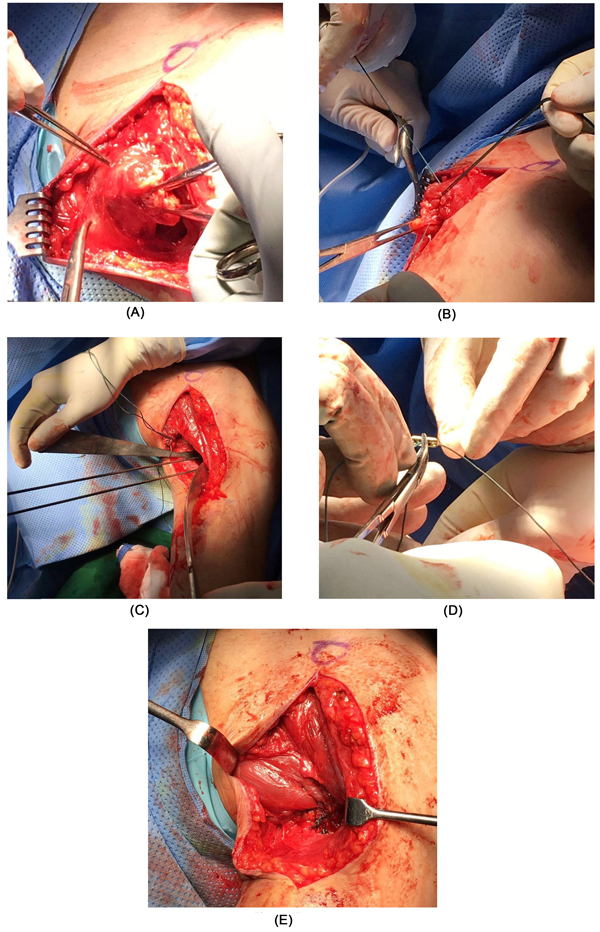
A limited 4-5 cm deltopectoral incision is made. The cephalic vein is identified and retracted laterally with the deltoid. The biceps tendon is identified, gaining access to the insertion of the pectoralis major, just lateral to the biceps tendon on the proximal humerus. A small Hohmann retractor placed laterally to the long head of the biceps tendon and around the cortex of the medial humerus, will subluxate the biceps medially, out of its groove, for protection. Medial dissection is then performed to identify the retracted tendon. In this case, since the patient suffered a muscle-tendon avulsion of the pectoralis major, we could identify and isolate the sternocostal and clavicular portions (Fig. 1A). These two muscle-tendon edges are freshened and number 5 synthetic polyester sutures (Ethibond Excel, Ethicon Inc; Johnson and Johnson, USA) are used to stitch the sternocostal and clavicular tendon ends separately by a modified Mason Allen suture technique (Fig. 1B). The pectoralis major has a very short tendon; therefore the repair construct must extend approximately 2 to 3 cm into the muscle to create an adequately strong repair.
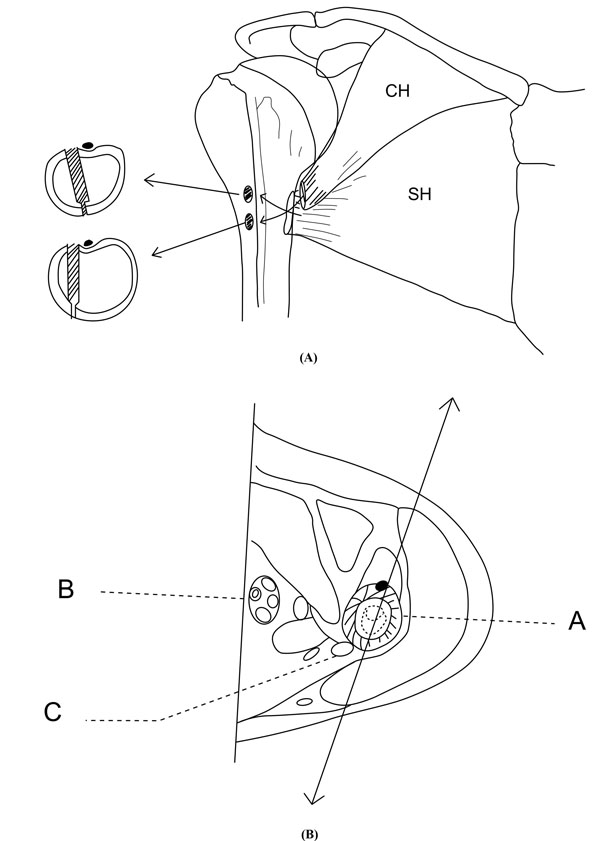
The anatomical insertion site of the pectoralis major tendon at the lateral edge of bicipital groove is then prepared [8]. It is important for the drill bits to be in the anatomic insertion point of the pectoralis major tendon to stay out of the bicipital groove (Fig. 2A and B). If too medial (in the biceps groove), the biceps may be incarcerated and potentially injured, thus having the potential to cause persistent pain.
The pectoralis major tendon inserts on the lateral lip of the bicipital groove of the humerus, with an average distance of 1.7 mm from the deltoid insertion [9]. The average length of this insertion point is 5.4 cm, which increases superiorly to inferiorly. The average width is 4.2 mm, decreasing lateral to medial [9, 10]. An electrocautery device is used to mark the button placement sites.
Two 2.7mm x 15” guide wires are drilled at an angle of 90º at the marked site and placed 3 cm apart. Care should be taken to avoid skydiving off the edge of the humeral shaft (Figs. 1C, 3A and 4). We left sufficient amount of bone bridge (3cm) between each button placement site to avoid increasing the risk of fracture. The guide wires should be stopped as soon as the pin penetrates the posterior cortex. This is followed by drilling the anterior cortex over the guide wires with a cannulated drill, the size of which should be the same as the measured diameter of the tendons (in this case, a 8-mm drill for a 8-mm tendon) (Figs. 3B and 4). Care is taken to only drill up to the posterior cortex without engaging the cortex or plunging through. Finally, the posterior cortex is drilled through with the 4.5-mm drill to allow for the passage of the EndoButtons (Figs. 3C and 4).


We used two 4 holed EndoButtons (one for the sternocostal head and another for the clavicular head) without a continuous loop (4.0 mm × 12 mm Endo-Button CL Ultra, Smith and Nephew, Andover, MA, USA) (Figs. 4 and 5). One limb of suture from the tendon end was threaded through the central two holes of the EndoButton (inside out – outside in). The other suture end from the tendon was passed through the terminal two holes of the EndoButton in a reverse manner i.e. from outside in – inside out) (Figs. 1D and 4). It is important to make certain that the suture limbs are not tangled. A 180° twist is then performed with the two strands of sutures, bringing the inferior portion of the sternal head proximal and deep to the clavicular head, thus re-creating the anatomic rotation of the tendon. The arm is placed into an adducted, neutral rotation position before fixation of the repair.

The EndoButton is loaded onto the Button deployment device and passed through each bone tunnel. Once the button clears the posterior cortex, the deployment instrument can be removed while the button deploys itself, locking into place on the posterior cortex. Pulling on the sutures shuttles both heads of the pectoralis major tendons into the humerus. The sutures are tensioned until the tendons are in contact with the posterior cortex (Figs. 3D and E). Finally, we advocate using a free needle to pass one suture through the tendon and tie down to the second suture to reinforce the fixation.
Unlike the use of the Biceps Button in the elbow, an additional interference screw is not required to achieve adequate fixation of the tendon. Rather, we use an additional suture, passed through the tendon of the pectoralis major, once it is shuttled through the humerus. This provides additional fixation strength to withstand physiologic loads. At this stage, additional few simple sutures with 2-0 absorbable sutures are used, connecting the tendons of the sternal and clavicular parts, thus making them as a single unit (Fig. 1E). Intra-operative radiographs are taken to confirm the position of EndoButton. After wound irrigation and closure, the patient is placed into a sling with the arm in an adducted position for the initial 2 weeks.
POSTOPERATIVE REHABILITATION
Early rehabilitation is started under the care of a trained physical therapist and focuses on early-passive and active-assisted range of motion. We allow flexion to 90°, abduction to 30° to 45°, and external rotation to 20° in the first 2 weeks. After that, range of motion is advanced progressively, as tolerated. Resistance training begins at 6 to 12 weeks postoperatively. A follow-up radiographic image showed well-positioned endobuttons (Fig. 6).

RESULT
Our patient was followed up to 13 months post operatively. He achieved full range of motion and strength by 3 months and started contact sports activities within 6 months, without any postoperative complications.
DISCUSSION
Pectoralis major tears typically occur from rapid eccentric loading, most commonly while performing bench press-type exercises [6]. This relation must be restored to achieve optimum function. Anatomical relations of the pectoralis major and the deltoid are best described by Klepps et al. [9] and Fung et al. [10]. The sternocostal and clavicular segments of the pectoralis major converge to form the tendon at the muscle’s insertion on the lateral lip of the bicipital groove of the humerus, which averages 1.7 mm from the deltoid insertion, bridging and acting as a retinaculum for the long head of the biceps [8, 9]. The average length of this insertion point is 5.4 cm, increasing superiorly to inferiorly, and the average width is 4.2 mm, decreasing lateral to medial [9, 10]. The superior two segments have unipennated and parallel fibers that insert most anteriorly and inferiorly (distally) on the humerus, whereas the inferior segment is multipennated with fibers that twist 180o to insert most posteriorly and superiorly (proximally) on the humerus. In exercises such as a bench press, the arm is adducted leading to muscle lengthening as the scapula protracts. This leads to lengthening of the insertion point relative to its origin, thus making it an eccentric contraction. For this reason, the sternocostal segment often ruptures first, thus placing greater stress on the remaining muscle and risking further rupture. This relation must be restored to achieve optimum function [2, 3, 8, 11].
The published literature describes several techniques for the fixation of a ruptured pectoralis major tendon: transosseous suture, suture anchor, and the pec button technique [12-15]. Load-to-failure testing showed no significant differences among the different fixation methods [12]. Rabuck et al. [13] conducted a cadaveric study with 30 specimens. They studied three different groups based on fixation method: a bone trough group, a cortical button group, and a suture anchor group. Load-to-failure testing showed no statistical differences between the bone trough group and the cortical button group. Although the bone trough fixation method has been widely used, it yields a higher propensity for fracture compared to the other methods of fixation [14].
In this article, we described a technique of repairing a ruptured pectoralis major tendon, in which we considered the best possible modifications to the previously described techniques, aiming to simplify the surgical procedure, achieve a very strong fixation, excellent patient outcome and avoid the possible surgical complications.
The use of a padded TriMano stand to support the operative extremity allows for greater control and exposure. The standard deltopectoral approach along with centering the incision slightly medially, allow for easier identification of the retracted tendon. Finally, the residual tendon aids in the identification of the pectoralis major insertion footprint. Our technique is an anatomic repair of the tendon with reattachment of the tendon to its footprint, recreation of the native anatomic course of the tendon and the native length-tension relation of the muscle. This optimizes the functional status of the muscle as close to pre-injury level as possible [15]. The limitation of this technique is that its role is limited to tendon avulsions and intratendinous injuries. It cannot be used for more proximal injuries at the myotendinous junction or intrasubstance tears of the muscle [15]. The strength of the repair is maximized by the use of two cortical buttons to bring the broad insertion of the avulsed tendon into the bone tunnel and bicortical contact.
Compared to the unicortical button technique, the existing Bi-cortical EndoButtons and tendon sliding technique has many drawbacks. Since two huge bicortical drill holes are made to incorporate the tendon into the bone tunnel, there is always a risk of stress riser and a secondary fracture at this site. Keeping maximum bone bridge between the two drill holes and drilling in a slightly different plane can avoid this. Moreover, the other drawback is the risk of injuring the radial nerve while passing the guide wires, drilling and flushing the EndoButton on the posterior cortex. Passing the guide wire and drill under intra-operative radiographic image guidance and knowing the anatomic landmarks of the radial nerve pathway can avoid this.
The advantages of the Bi-cortical EndoButtons and tendon sliding technique we describe, compared to the unicortical button technique are many. Our technique achieves a stronger and better incorporation of the tendon with bone, considering the wider surface area of contact between them. Moreover, the direction of pull of muscle and the position of the endobuttons are not in the same plane i.e. the direction of the muscle pull is along coronal plane, whilst the direction of the drill is in the sagittal plane. Therefore, the pull out strength of this repair is theoretically better, hence leading to better internal rotation power of the arm. In the unicortical button technique, the bone surface has to be prepared with a rasp or burr for better incorporation, this can thin out the cortex and lead to the endobutton cutting-through the cortex. Finally, if the unicortical technique fails, the EndoButton can be lost in the medullary canal, contrary to the bicortical button technique.
CONCLUSION
The Bi-cortical EndoButtons and tendon sliding technique is a safe, reliable, easy to reproduce, cost-effective, less time consuming and effective method in achieving the goals of a strong fixation and an anatomic repair of the tendon back into its native footprint. However, further biomechanical and clinical studies are needed to compare the outcomes and complication rates of this technique with other described repair techniques.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


