All published articles of this journal are available on ScienceDirect.
Arthroplasty in the Valgus Knee: Comparison and Discussion of Lateral vs Medial Parapatellar Approaches and Implant Selection
Abstract
Constrained implants are frequently used for primary total knee arthroplasty (TKA) in patients with moderate and severe genu-valgum (>10˚). This deformity presents corrective challenges for ligament release. The lateral-parapatellar approach has been advocated as an alternative to the traditional medial-parapatellar approach. Claimed advantages include better access for release of tight ligamentous structures, without requirement for release of the medial-collateral ligament.
We present our comparative experience of the use of an unconstrained knee-replacement prosthesis inserted by the lateral-parapatellar approach in comparison to a constrained-knee prosthesis inserted via the medial-parapatellar approach.
49 primary total knee-replacements in 48 (6 males, 42 females) patients were performed; 32 through a lateral-parapatellar approach (group L) using an unconstrained-prosthesis and 17 through a medial-parapatellar approach more often requiring a constrained-prosthesis (group M). Mean preoperative valgus angle was 18.5 (range 11-34˚). Patient demographics (p=0.7) and valgus correctability were similar between the two groups.
There was no significant difference in the mean post-operative valgus angle. This was 4.2˚ (range 1-9.5˚) using the lateral-parapatellar approach and 5.3˚ (range 0.3-10˚), p=0.12, using the medial-parapatellar approach.
Transient common peroneal injury occurred in 2 patients, both group L, in the presence of valgus angles of greater than 20˚. To date no joints have been revised, or are unstable.
The use of a lateral-parapatellar approach, appropriate soft tissue release, and an unconstrained PCL-preserving implant, yielded in all cases a stable, well aligned knee arthroplasty. This represents a viable alternative to the constrained-prosthesis using a medial-parapatellar approach in patients with moderate and severe genu-valgum.
INTRODUCTION
The valgus knee can present greater challenges of ligament balance in total knee arthroplasty in comparison to varus aligned knees [1]. Restoration of neutral mechanical axis and correct ligament balance are important factors to reduce incidence of complications relating to instability, loosening, premature wear and patella mal-tracking [2-5].
The option of using a constrained or an unconstrained (PCL retaining) implant for arthroplasty of the moderate to severely valgus knee remains an area of controversy [6]. Some surgeons consider the valgus knee to be a relative contraindication to implanting an unconstrained prosthesis [7].
Optimised survival rates have been reported with restoration of overall alignment between 2.4° and 7.2° valgus, with failure of varus aligned knees through medial bone collapse and valgus aligned knees with ligamentous instability [8]. Multiple papers support the importance of correct alignment in increasing implant longevity [9-12], through the reduction of strain at the implant bone interface [13].
Variability exists in the reported survivorship of unconstrained implants performed on valgus deformed knees, with some authors reporting Kapplin Meier survival at 10 years of 79% from all causes (80% with instability as an endpoint) [14], yet others suggesting a 96.2% 10 year survival in knees with 20° or more valgus [6].
There remains debate regarding the use of unconstrained prosthesis in the valgus knee. The lateral parapatellar approach has been advocated as an alternative to the medial parapatellar approach in the valgus knee as release of tight lateral structures is facilitated with the approach.
METHODS
Retrospective comparison was conducted on two groups of patients with surgery undertaken by two experienced knee surgeons (J.J. & N.C.), using two separate approaches and implant constraints. We sought to establish whether the use of a lateral parapatellar approach with an unconstrained implant provided similar angle of correction and stability as a medial parapatellar approach using mostly constrained prosthesis.
Patients with a preoperative valgus deformity >10o were identified from hospital medical records and radiographs. Tibio-femoral alignment (TFA) was assessed using a digital goniometer (IMPAX) and analysed by a single author (JR). Postoperative radiographs were analyzed in a similar way. Specific long leg films were not available.
Medical records and radiographs were reviewed for demographic details and for post-operative complications and revision surgery. Data handling and analysis was conducted using Microsoft Excel spreadsheet and SPSS.
Patients underwent a total knee arthroplasty through either a lateral parapatellar approach, as described by Fiddian [15], using an unconstrained implant in all cases (group L, surgeon J.J.) or through a medial parapatellar approach, as described by Ranawat [5], using a variety of constrained and unconstrained implants (group M, surgeon N.C.).
RESULTS
Forty-nine total knee replacements were performed in 48 patients (42 women and 6 men) with a tibiofemoral angle of greater than 10° who underwent primary total knee arthroplasty between September 2004 and October 2011. Thirty-two arthroplasties were performed through a lateral parapatellar approach of which all had an unconstrained AGC knee implanted (group L). 17 total knee arthroplasties were performed through a medial parapatellar approach using a variety of constrained and unconstrained implants as shown in Table 1 (group M).
Summary of results.
| Group L | Group M | P Value | |
|---|---|---|---|
| Patient number | 32 M:F = 1:9.7 |
17 M:F = 1:4.7 |
0.7 |
| Age (years) | 73.7 | 70.1 | 0.3 |
| BMI | 31.7 | 29.9 | 0.6 |
| Pre-op correctability (clinically judged) |
0.76˚ | 0.83˚ | 0.07 |
| Level of prosthesis constraint | 32 unconstrained | 6 unconstrained 5 posterior stabilised 5 high post/varus-valgus constrained 1 fully constrained |
|
| Mean pre-op TFA | 18.5˚ ( range 13-29˚) | 18.4˚ ( range 10.1-34˚) | |
| Mean post-op TFA | 4.1˚ (range 1-9.5˚) | 5.6˚ (range 0.3-10˚) | 0.05 |
| Complications | Transient common peroneal nerve palsy: 2 patients | Superficial wound infection: 3 patients |
There were no significant differences between group L and M regarding age, BMI or preoperative TFA.
Group L had a statistically significant lower TFA postoperatively in comparison to group M (4.1˚ vs 5.6˚, respectively, p=0.05). Furthermore there were 4 knees with a postoperative TFA greater than 8° in group M, and only 1 in group L.
There were no reported cases of patella maltracking, instability or revision from any cause in either group. There were also no proven deep infections in either group, however, group M had 3 superficial wound infections; group L did not have any. There were two cases of common peroneal nerve injury, both were found in group L.
DISCUSSION
Approximately 15% of patients have significant valgus deformity (>10 degrees) [16]. There remains debate as to what the most effective and reliable method of achieving patient satisfaction, deformity correction and long-term prosthesis survival.
Different options exist for surgical approach and prosthesis selection. The traditional medial parapatellar approach in the valgus knee requires access to the lateral structures to achieve balance [5]. In the experience of one of the authors (J.J.) this can present difficulty of clear access and identification of these structures.
As shown in Fig. (1), medialising the mechanical axis in the corrected valgus knee overcomes the medial collateral ligament laxity, resulting in a stable and functional joint achieved using an unconstrained prosthesis. Fig. (2) shows this concept with a highly valgus knee of 20o being overcorrected to 3o of valgus.
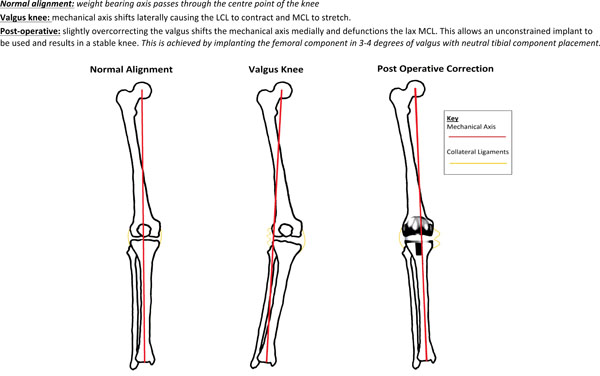
Diagram illustrating slight overcorrection of valgus deformity with an unconstrained implant to achieve a stable and well balanced knee.

Pre and post-operative radiographs of unconstrained implant in corrected valgus knee.
The alternative use of the lateral parapatellar approach, as described by Fiddian, allows for easier access to tight lateral structures which can be sequentially released [15]. Additionally no further release of the already stretched medial collateral ligament is required in this approach.
We recognise limitations exist within our study, including: limited formal post-operative follow-up beyond 1 year, although it is assumes that patients with significant problems would re-attend.
Apostolopoulos et al. [16] also described the value of a lateral parapatellar approach for patients with severe valgus deformity (15-35o, mean = 23o), reporting good outcomes in correction of deformity (2-7o, mean = 5.5o) and osteotomy union in all 24 patients. Their approach also incorporated tibial tubercle osteotomy to improve access and for mechanical realignment purposes, which we found not to be necessary in our patient group. They described the value of the lateral parapatellar approach in the valgus knee as giving improved access to release tight lateral structures and the potential to incorporate lateral release as part of the surgical approach.
Our study highlights that the lateral parapatellar approach is a safe option in correcting the moderate to severe valgus knee, with appropriate soft tissue release, and an unconstrained PCL-preserving implant as a viable alternative to the use of the medial parapatellar approach and greater levels of implant constraint.
In all cases the lateral approach yielded a stable, well aligned knee arthroplasty.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors acknowledge the permission of Mr N, Coleman for inclusion of his patients in this study.


