All published articles of this journal are available on ScienceDirect.
Magnetic Resonance Imaging-Based Diagnosis of Occult Osseous Injuries in Traumatic Knees
Abstract
Background :
Occult osseous knee injuries, such as bone bruises, can produce persistent pain and functional loss. Although bone bruises cannot be identified through direct examination or traditional radiographs, magnetic resonance imaging (MRI) has emerged as an effective diagnostic method. Nevertheless, the natural history of these injuries remains to be fully defined. Therefore, we used MRI to detect and follow bone bruise injuries secondary to knee trauma.
Methods :
We retrospectively reviewed knee MRIs from patients with bone bruising caused by trauma. Occult injuries were initially identified by MRI and subsequently rescanned for follow-up at 3 and 9 months. All patients underwent physical examinations, direct radiological imaging, and MRI.
Results :
Although direct radiographs showed no abnormalities, we used MRI to identify a total of 22 patients (age range: 19–42 years; mean: 28 years) with bone bruising. After 3 months, injuries remained detectable in 68.2% of the subjects, whereas 18.2% displayed bone bruising after 9 months. The majority of Type I lesions resolved spontaneously, whereas 80% of Type II injuries remained following 3 months, and 30% persisted at 9 months. Ligament and meniscal lesions were observed in 63.6% of patients with bone bruising and appeared to hinder recovery.
Conclusion :
Bone bruises generally resolved within 3 to 9 months in subjects with no soft tissue lesions and minor trauma. However, ligament and meniscal lesions were observed in the majority of patients, and these individuals required longer treatment and recuperation. Overall, these findings can contribute to improving the management of occult osseous knee injuries.
INTRODUCTION
Occult bone lesions of the knee can present with substantial clinical symptoms, including acute pain and functional loss in the joint [1-3]. Nevertheless, despite these obvious manifestations, these injuries are called “occult” because conventional radiographs and arthroscopy cannot detect the associated lesions. In this regard, magnetic resonance imaging (MRI) of the knee has become an important, non-invasive diagnostic procedure for detecting occult injuries, such as fractures and bone bruises, as well as damage to the menisci, ligaments, and tendons of the knee.
Indeed, increased use of MRI technology to assess the acutely injured knee has led to greater awareness that bone bruising represents a distinct clinical entity [4]. Theseinjuries result from traumatic and forceful impacts that often occur during sports activities or accidents. Bone bruises are characterized by hidden fracturing in the inner layer of the bone, which produces severe pain that can last for weeks or even months. Although it has become increasingly apparent that bone bruises can be associated with soft tissue injuries [5-7], isolated bone bruise abnormalities can also produce severe clinical symptoms that require prompt therapy. In this respect, bone bruises typically require rest, support, and protection of the injured knee, as well as conventional trauma-related treatments.
It has been reported that bone bruises can be visualized via MRI as soon as 1 h after trauma, but may require up to 30 h before they can be detected [8]. These injuries are classically depicted as geographic, non-linear areas of signal loss on T1-weighted imaging and high signal intensity on T2-weighted imaging [2, 3]. Moreover, systems have been introduced for classifying such MRI-identified abnormalities [7]. However, although MRI has proven to be an effective manner for early detection of bone bruises, there is no consensus on the natural history of occult bone injuries secondary to knee trauma. Moreover, recent literature has suggested that further research is needed to improve the management and treatment of traumatic bone bruising, especially when associated with soft tissue injuries [9].
Therefore, in order to better understand the natural progression of occult osseous injuries secondary to knee trauma, we retrospectively reviewed MRIs to identify patients with bone bruises. The traumatic knees of these subjects were subsequently rescanned for follow-up at 3 and 9 months to determine characteristics that might contribute to prolonged recovery.
MATERIALS AND METHODS
Patients and Study Design
This was a retrospective, multi-center study conducted at various hospitals in Istanbul, Turkey. We reviewed MRIs from patients with bone bruising caused by traumatic injury to the knee from March 2010 to September 2013. Only those patients showing no fracture on plain radiography were included. Knee MRIs were performed on patients showing no response to one week of conservative treatment, consisting of simple analgesics, cold application, and no weight bearing. Notably, intra-articular injections, steroids, and viscosupplementation were not employed. Soft tissue injuries received conservative treatment from orthopedists. Patients exhibiting any of the following characteristics were excluded from the study: previous symptom or pathology of the knee; severe injury (a trauma resulting in any bone fracture or a soft tissue problem which needs grafting or together of these clinical findings); rheumatoid arthritis causing degenerative arthropathy; or degenerative arthritis, psoriasis, and hemophilia. Also, patients who underwent surgery were excluded. Included patients were assessed by two more MRI examinations at approximately 3 months (range: 2.5-4 months) and 9 months (range: 8-10 months) after the initial trauma. Notably, the local ethics committee approved this study, and written informed consent was obtained from all participants.
MRI Analysis
Knee MRIs included coronal T1 sequences, sagittal T2 sequences, and sagittal-coronal T2 fat-suppressed sequences. All MRI data were analyzed based on double-blind interpretations made by two radiologists. Diagnoses of occult bone bruises were established based on the presence of decreased signal intensity on T1-weighted sequences along with increased signal intensity on T2- weighted and fat-suppressed T2-weighted sequences. Moreover, the MRI findings were classified based on criteria previously described by Lynch et al. [7]. Briefly, on short echo time (TE) and T2-weighted images, Type I lesions showed signal intensity loss that was primarily located within the medullar cavity of the bone, without cortical interruption. In contrast, Type II lesions were defined by a loss of signal intensity associated with interruptions in the black cortical line (defined as a fracture combined with bone bruising in the present study). Type III lesions were characterized by a loss of signal intensity without definite cortical interruption in the bone regions adjacent to the cortex. The radiologists also defined the soft tissue injuries.
RESULTS
In the present study, we retrospectively reviewed knee MRIs from patients with bone bruising caused by traumatic injury. A total of 22 patients were enrolled in the study (8 females and 14 males; age range 19-42 years; mean: 28 years). All patients were admitted to the hospital with knee injuries, which resulted from falling (from a height) in nine patients and sports trauma in thirteen patients. Notably, no pathological signs could be detected through direct radiological evaluations (Fig. 1). However, these patients presented bone bruise abnormalities in an initial MRI analysis, with bone marrow edema detected and classified as Type I lesions (Fig. 2) in twelve patients and Type II lesions (Fig. 3) in ten patients (see Table 1). We observed no Type III lesions.
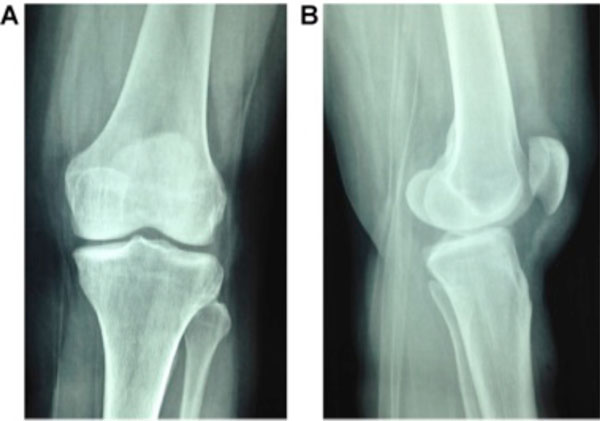
Post-traumatic normal radiographs: A) anteroposterior view; B) lateral view.
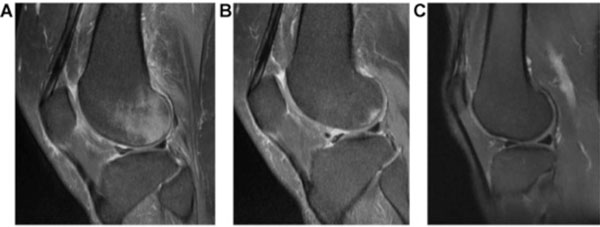
Magnetic resonance T2-weighted images of Type I injury: A) first sagittal MRI of the knee; B) second sagittal MRI of the knee (after 3 months); c) third sagittal MRI of the knee (after 9 months).
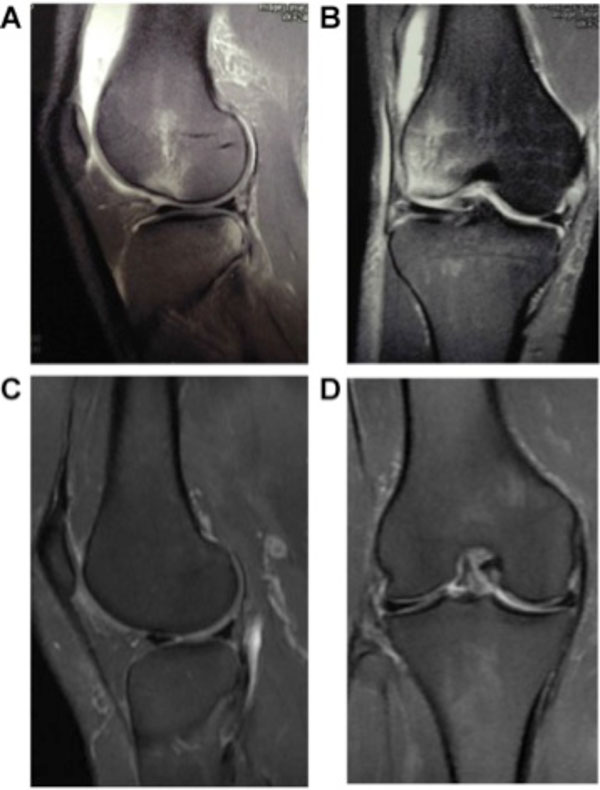
Magnetic resonance T2-weighted images of Type II injury: A) first sagittal MRI of the knee; B) first coronal MRI of the knee; C) third sagittal MRI of the knee (after 9 months); D) third coronal MRI of the knee (after 9 months).
Classification of initial and follow-up MRI findings*.
| MRI | Type 1 | Type 2 |
|---|---|---|
| First | 12 | 10 |
| Second | 7 | 8 |
| Third | 1 | 3 |
* Classification of images according to the criteria defined by Lynch et al. [7].
MRI, magnetic resonance imaging.
Other lesions found in patients with MRI-detected bone bruises.
| Number of Patients | No Other Lesions | Total ACL Rupture | Interstitial ACL Rupture | MCL Lesion | Meniscal Lesion |
|---|---|---|---|---|---|
| 22 | 8 | 4 | 4 | 3 | 3 |
MRI, magnetic resonance imaging; ACL, anterior cruciate ligament; MCL, medial collateral ligament.
Follow-Up MRI Examinations
Patients were subsequently assessed by two more MRI examinations at 3 and 9 months following the initial injury. The 3-month MRI revealed that bone bruising was still present in 68.2% of the patients, whereas 18.2% continued to display bruising after 9 months (Table 1). Moreover, when considering the type of injury, our findings indicated that while 58.3% of the Type I lesions were still apparent after 3 months, most resolved by 9 months (only 8.3% remaining) (Table 1). In contrast, 80% of the Type II lesions persisted at 3 months, with 30% remaining for at least 9 months (Table 1). Thus, Type II lesions required longer treatment and recovery.
Soft Tissue Involvement
Soft tissue lesions were observed in 63.6% of the patients with MRI-detected bone bruises, including anterior cruciate ligament (ACL) ruptures, medial collateral ligament (MCL) lesions, and meniscal lesions (Table 2). Notably, at the 3-month follow-up, bone marrow edema was resolved in seven patients, all of which displayed no soft tissue lesions. At the 9-month MRI, bone marrow edema was still detectable in four patients (18.2%), and these patients all had suffered total ACL rupture. However, all four subjects refused reparative surgery due to their sedentary lifestyles.
DISCUSSION
Here, we found that MRI-detected bone bruising generally resolved within 3 to 9 months in patients without soft tissue lesions and minor trauma. However, a longer recuperation period was required for individuals with bone bruises in combination with ligament and meniscal lesions.
Although MRI has been used to accurately diagnose knee joint injuries for decades, the terms bone bruising and bone marrow edema have only been around for the last decade and appear to be used synonymously [10-15]. That being said, in 1988, Wilson et al. [10] had already reported ill-defined bone marrow hyperintensities on T2-weighted MRI performed in patients with persistent knee and hip pain, but normal radiographic results. These findings resolved spontaneously in all cases, and it was proposed that this MRI phenomenon might be related to a transient increase in bone marrow water content.
Indeed, injuries that result from knee trauma generally resolve in a short period [11]. In fact, for some patients, implementing precautions that prevent weight load on the knee joint are sufficient for treatment. However, there is no definite consensus on the natural history of occult bone injuries secondary to knee trauma. In this regard, we found that most of the Type I lesions spontaneously resolved. However, it has been reported that 66% of Type II lesions persist, leading to subchondral sclerosis, cartilage thinning, osteochondral defects, or cortical impaction [3, 13]. Here, we observed that 80% of Type II lesions remained for 3 months, and 30% lasted for at least 9 months, confirming the notion that Type II injuries require longer treatment and recovery.
Notably, no pathological signs could be detected in direct knee radiographs following injury in our patient cohort. However, MRI findings revealed bone contusions characterized by low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Nevertheless, obvious fracture lines were not detected on the trauma-exposed bone surfaces. Notably, occult osseous injuries that could not be detected on direct radiographs were the most common lesions detected by MRI in our study, highlighting the power of MRI technology for assessing knee trauma.
Although the cause of post-traumatic arthritis following knee injury is likely to be multifactorial, it was suggested that it might develop secondary to chronic knee instability. In this regard, soft tissue lesions that can destabilize the knee were detected in almost all patients with bone bruising [12, 16-18]. Moreover, these injuries appeared to be more serious when bone marrow edema was present, especially with regard to ligament injuries [16, 17, 19]. Thus, it is possible that bone bruising represents a useful prognostic sign in predicting which patients will go on to develop degenerative arthritis. Indeed, bone bruising can indicate an overlying osteochondral injury, particularly if a pattern of resolution towards an articular surface is demonstrated during follow-up MRI. Further research will be required to determine the potential relationship between bone bruises and post-traumatic arthritis.
This study presented certain limitations. Indeed, the small sample size may not have been sufficient to draw definitive conclusions regarding the course of bone bruise injuries. In addition, the restricted age of our cohort may have biased our conclusions, affecting applicability of these findings to older or younger subjects. However, our patients acquired bone bruising through sports trauma and falls, which are common causes of these impact-induced injuries. Nevertheless, further study may be required in a larger more diverse patient population.
CONCLUSION
MRI-detected bone bruising generally resolved within 3 to 9 months in patients with no soft tissue lesions and minor trauma. However, ligament and meniscal lesions were observed in the majority of patients with bone bruising, and these individuals required longer recovery periods. In addition, also spontaneous osteonecrosis of the knee (SONK) can be detected earlier and its treatment can be achieved better in by using MRI. Thus, the combination of occult bone injury and osteochondral trauma might indicate a more severe injury needing prolonged and careful treatment. These findings contribute to our understanding of the natural progression of MRI-detected bone bruises secondary to knee trauma and can contribute to improved management of patients with occult osseous knee injuries.


