All published articles of this journal are available on ScienceDirect.
Surgical Management of the Forefoot in Patients with Rheumatoid Arthritis - A Review Article
Abstract
Foot and ankle pathologies cause a significant disease burden on rheumatoid patients. Forefoot pathologies causes pain, callosities and possibly ulceration, and can cause problems with footwear. Forefoot correction in rheumatoid patients has historically comprised of excision of diseased joints. While satisfaction was high with this procedure, complications, changing expectations and improvement in medical therapy have raised expectation of patients, physicians and surgeons alike. This review assesses the role of joint preserving osteotomies and arthrodesis, as well as associated complications. It also describes the role of the multidisciplinary team in the management of these patients.
INTRODUCTION
Foot and ankle problems become increasingly common in rheumatoid patients with time. Over 50% of patients may have a foot and ankle problems at any time [1-3], with a lifetime prevalence of up to 90% [4, 5]. Over 65% patients have forefoot involvement at presentation, and lesser toe deformities are more common [6]. In the primary care population, foot and ankle problems are twice as common in rheumatoid patients [7].
Ulceration of the rheumatoid foot is also a significant issue with a prevalence of nearly 10% in the forefoot, with the dorsum of the interphalangeal joints, lesser metatarsal heads and the first metatarsalphalangeal joint in hallux valgus being common sites [8]. Foot wounds have previously prompted investigation and treatment with one study reporting foot wounds at presentation in 13% and active ulceration in 5% [4]. Where possible, non-surgical and surgical management should be initiated prior to the development of foot wounds.
Hallux valgus has the same etiology in the rheumatoid population as it does in non-rheumatoid population. This may be idiopathic, hereditary, or related to joint laxity and shoe wear. It is however undoubtedly worsened by the ligamentous laxity, soft tissue synovitis and destruction, and eventual joint instability of progressive rheumatoid disease.
Initial assessment should always include detailed history taking and a thorough clinical examination. It is important to identify patient expectations, and common presenting complaints include deformity with or without pain, difficulty in shoe wear, decreased mobility and balance along withcallosity formation and ulceration. Examination of the forefoot should focus on deformity of the first ray (hallux valgus) and its ability to perform its weight-bearing mechanical function. Prominence of a painful medial eminence or bunion with or without inflamed bursa, deformities of the lesser toes, commonly claw and hammer toes, with painful callosity formation over the dorsum of the interphalangeal joints and under the exposed metatarsal heads should be sought. Frank dislocation of the lesser metatarsal phalangeal joints (MTPJs) is not uncommon. Deformities of the lesser toes should be assessed to determine if they are passively correctible or not. Care should be taken to assess the quality of the soft tissue and look for and document areas of active or healed ulceration, or any areas of threatened skin. Examination should also include gait assessment and power of the hallux tendons. Early management of patient with rheumatoid foot problems should include referral to podiatric and foot health services to manage corns and calluses, and provide appropriate orthoses or surgical footwear. This intervention alone will manage a significant proportion of patients who are having symptoms from friction or ill-fitting foot wear secondary to deformity. Studies have shown this intervention to result in an improvement in pain and function for up to 30 months in a rheumatoid population [9]. In addition, patients will often be taking oral therapies to control flare-ups of disease or at initial presentation. The use of immunosuppressants and Disease Modifying Anti-Rheumatic Drugs (DMARDs) has been reported to significantly reduce the need for surgical intervention since 1985 [10]. One cross sectional study of consecutive rheumatoid patients referred for orthopaedic assessment found that 89% used at least one DMARD. This was more likely to be the case in those with a more recent diagnosis [11]. Van der Leeden et al. found that 30% of patients who achieve medical remission of their disease still have pain and or swelling of at least one MTPJ [12]. Often patients present for surgical intervention with an established diagnosis, medical therapy regimen including cytotoxic drugs and biological therapy, and having been seen by the podiatric services.
Common procedures for the forefoot in rheumatoid arthritis can be divided into joint preserving and joint sacrificing surgeries. They include soft tissue procedures such as tendon release, corrective osteotomies, arthroplasty, arthrodesis and excision arthroplasty. Over the past 20-30 years, there has been a decrease in surgical intervention with the development of better medical management of the rheumatoid patient [10]. Matricali et al. however found that earlier interventions in the foot were still being performed in view of increased patient expectations [4] and this was associated with a trend towards more join preserving surgery. Joint sacrificing procedures, however, remain the mainstay of foot and ankle surgery in the rheumatoid population [4, 11].
INDICATIONS FOR SURGERY AND NON-SURGICAL MANAGEMENT
Once the diagnosis of rheumatoid arthritis has been made, the primary aim is to refer to a rheumatologist to optimise medical therapy. Patients with ongoing foot and ankle problems should then be referred for non-surgical intervention via the orthotics and physiotherapy routes with the aim to provide relief of painful areas in the forefoot and hind foot with cushioned or recessed support, mechanical support for the arch and appropriate heel wedge to correct flexible hindfoot deformity. This should be combined with physiotherapy exercises to strengthen the dynamic support to the arch. Significant forefoot deformity in patients with largely shoe wear problems can be appropriately managed with accommodative surgical footwear in the first instance. Treating hardened painful corns and cushioning specific points of pressure or using spacers between toes that cause pain or ulceration helps prevent complications. When these methods fail, patients with painful synovitis in joints or tendon sheaths can undergo steroid injection usually under ultrasound or radiographic guidance. Selective local anaesthetic injection can aid the diagnostic process in determining which joints are contributing to the patient’s pain.
Indications for surgery include failure of non-surgical measures with ongoing pain or deformity. This will commonly include painful bunion or painful stiff first MTPJ, combined with pain under the lesser metatarsal heads from synovitis, destruction of the plantar plate or frank dislocation of the MTPJ. Pain under the tips or over the PIPJ of clawed, hammer or mallet toes or ulceration/callosity is also an indication for surgery. Any worsening deformity or deformity interfering with shoe wear should also be considered an indication for surgery.
METHODS OF FOREFOOT RECONSTRUCTION: SURGERY TO THE FIRST RAY
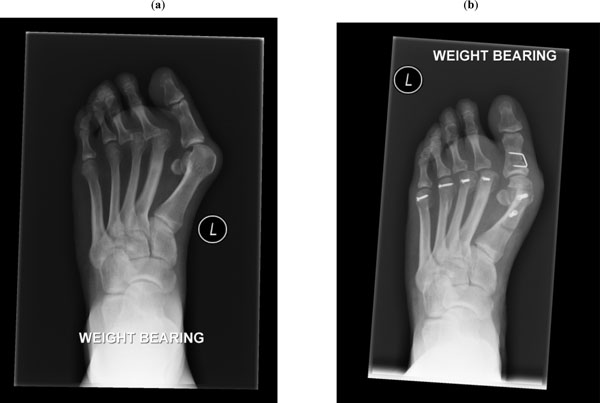
First MTPJ arthrodesis - this remains the gold standard with preparation of both joint surfaces and fusion in approximately 10-15 degrees of valgus and 10 degrees of dorsiflexion from plantar surface (Fig. 1). Several methods of fixation exist such as simple lag screws and dorsal low profile plates produced by several manufacturers. These act only as a temporary fixation to allow bony union. Often depending on the method of fixation to be used, the joint can be approached from the dorsal or medial aspect. We found 10 articles specific to forefoot correction in the rheumatoid population performing arthrodesis of the first MTPJ. Patient satisfaction was consistently high with good or excellent results in 85-96% [13-17]. The largest study was by Dai et al. who reported 129 feet followed for 37 months average. They reported overall improvement in Japanese Society for Surgery of the Foot (JSSF) scores from 33 to 67 and correction of the hallux valgus angle from a mean pre-operative angle of 50 degrees to 21 degrees post-operatively [18]. They had a 3.1% non-union rate at 37 months, the lowest amongst the aforementioned studies (3.1-8%). Most studies report significant improvement in patient reported outcome measures [13,15,16,18] and correction of the hallux valgus angle [13, 15, 18-20]. Studies reported a varied re-operation rate for lesser toe recurrent deformity, metatarsalgia and removal of metalwork of up to 30% [19].

(a) Pre-operative forefoot with significant hallux valgus and subluxation of 2nd MTPJ, (b) Post-operative foot having undergone 1st MTPJ fusion with locking plate, lesser metatarsal Weil osteotomies and 2nd PIPJ fusion with intramedullary smart-toe™ device.
(a) Pre-operative forefoot with significant hallux valgus and disloacation of the 2nd and 3rd MTPJs, (b) Post-operative forefoot having undergone joint preserving Scarf and Akin osteotomy with incomplete correction combined with lesser metatarsal Weil’s osteotomies.
First metatarsal osteotomy (Scarf/Chevron/Hohman) - Joint preserving surgery is becoming more popular in the rheumatoid foot, providing stable correction of deformity along with maintaining mobility of the joint (Fig. 2). This will not always be applicable to all patients especially those with significant stiffness, joint destruction, or secondary degenerative changes. In mild to moderate hallux valgus disease, this provides significant improvement in hallux valgus angle and patient reported outcomes. Barouk et al. (2007) reported 95% good correction with Scarf osteotomy at 2 years in 55 patients with rheumatoid hallux valgus [21] Niki et al. (2010) reported improvement in JSSF from 52 to 89 at 3 years follow-up with hallux valgus correction improving from 47 to 9 degrees post-operatively [22]. Bhavikatti et al. (2012) reported similar improvements in American Orthopaedic Foot and Ankle Society (AOFAS) score from 39 to 88, and in the hallux valgus angle from 32 to 14 degrees at a longer follow-up period of 51 months [23]. Modified Mann proximal crescentric osteotomy was used by Takakubo et al. (2010) in significant hallux valgus resulting in improved patient reported outcome measures (JSSF improved from 44 to 72) and a correction of the hallux valgus angle (39 to 29 degrees) in 11 feet at 3.6 years. They reported 3 cases of recurrence of hallux valgus (27%) [24]. Overall complications were relatively few. In the study by Barouk et al., only one patien had to be revised to an arthrodesis (1.8%) [21], while the studies by Niki et al. and Bhaviktti et al. reported rates of residual stiffness as 28.2% and 22.4% respectively [22, 23].
First MTPJ excision (Keller’s/Mayo excision arthroplasty) - Excision of the first metatarsal head for significant destructive synovitis has historically been a useful operation. With improved medical therapy however the destructive disease burden is less, and this procedure is now reserved as a salvage procedure. Complications associated with Keller’s excision arthroplasty include recurrence of hallux valgus, cock-up deformity and flail toe [25]. Transfer metatarsalgia secondary to defunctioning of the first ray was also demonstrated by Henry et al. (1975) who used foot printing to establish the ability of the first ray to bear weight. They found that only 40% of the weight of the foot was taken by the first ray after excision arthroplasty. Following first ray arthrodesis, this value was 80% [26]. Nevertheless, there is literature to support the use of this procedure in the right patient. Vahvenan et al. (1980) reported 93% good or fair results following excision arthroplasty in 179 feet at 5 years follow-up [27]. Thomas et al. (2006) also achieved good correction and standardised AOFAS scores at 5.5 years without revision [28]. Grondal et al. (2006) performed a prospective randomised trial comparing arthrodesis and Mayo excision and found no significant differences between the groups in terms of disability scoring, correction or pressure measurements. While this study displays very positive results for excision, it was limited by a short follow-up and relatively small patient numbers [20]. Other studies found dissimilar results. Mulcahy et al. (2003) demonstrated improved disability scores and decreased pressures under the lesser toes with arthrodesis compared with excision for the 1st MTPJ in 138 feet [29]. Torikai et al. (2008) found that significant improvement in hallux valgus angle could not be achieved by excision whereas it could be achieved with arthrodesis [5].
First MTPJ silastic implant - Use of silastic implants (polymeric silicone) e.g. Swanson hinges, hemiarthroplasties and spacer devices have fallen out of favour due to osteolysis, loosening and granulomatous reaction to silicone particulate matter [30]. Rahman & Fagg (1993) reviewed 78 feet at 4.5 year follow-up who had undergone silastic implant to the first MTPJ for either hallux valgus or hallux rigidus and found 72% had radiological loosening [31]. In rheumatoid forefeet, Fujioka et al. (1999) achieved good correction of hallux valgus at 8 years follow-up with Swanson silastic implants, but found significant rates of implant breakage (77%) and loosening (63%). Despite the complications, they reported 95% patients achieving pain relief and only one undergoing revision surgery [32].
METHODS OF FOREFOOT RECONSTRUCTION: SURGERY TO THE LESSER RAYS
Lesser MTPJ surgery includes closed osteoclasis, surgical debridement or arthrolysis, oblique shortening Weil’s osteotomy and excision arthroplasty (Figs. 1, 2). Excision arthroplasty is popular for rheumatoid patients and is essentially unchanged from the original description by Hoffman in 1911 [33]. Assessing the differences between these procedures is difficult as in practice Weil’s osteotomy and excision arthroplasty will be combined with soft tissue procedures such as debridement of synovitis and arthrolysis. Trieb et al. (2013) reported on 72 rheumatoid feet undergoing Weil’s osteotomy for lesser toe dislocations with 54 months follow-up [34]. Lesser toe specific AOFAS outcomes improved from 21.9 to 63.3 post-operatively. Decrease in joint stiffness and severe pain was noted in 96% and 97% of patients respectively. Overall satisfaction was high in 88% and recurrent or persistent subluxation occurred in onlt 14% of joints. Bolland et al. (2008) combined Scarf with Weil’s osteotomy for the lesser toes and reported a lesser toe recurrence of pain in 12% [18]. Krause et al. (2011) reported on first ray arthrodesis of 24 feet followed for 133 months combined with either arthrolysis or excision of the lesser metatarsal heads [35]. They reported that while AOFAS scores improved for both groups, those that had metatarsal head excision were more likely to have sagittal malalignment. The Stainsby procedure that involves excision of part of the proximal phalanx, reduction of the plantar plate and kirschner wire fixation, is a variant of an excision
arthroplasty. This was described by Briggs & Stainsby (2001) in their original paper where 29 patients, not all rheumatoid, had multiple toe surgery and were followed up for a mean of 5 years with 81% patients remaining symptoms free [36]. This procedure allows the preservation of the metatarsal head for weight bearing. Dodd et al. (2011) were able to demonstrate an improvement in walking and pain scores in 16 consecutive cases at a minimum 6 month follow-up [37]. Both the Weil and Stainsby procedure have a theoretical advantage over excision arthroplasty by preserving the plantar attachment and the windlass mechanism for the lesser rays to bear weight [38]. Interestingly Siddle et al. (2013) found no difference in pain or outcome score in patient randomised to combined therapeutic assessment with or without sharp scalpel debridement of painful callosities [39].
LESSER TOE CORRECTION
Fixed interphalangeal joint flexion leading to hammer toe deformity or claw toe deformity often requires surgical correction in combination to lesser ray surgery. Flexible deformities can be treated with selective tenotmy. Fixed deformity can undergo a closed osteoclasis (snapping of the fixed structures) or arthrodesis and intramedullary fixation with either kirschner wires or memory metal devices such as the smart toe ™ (Stryker, NJ, USA). Both aim to arthrodese the flexed joint. Scoll et al. (2013) retrospectively compared 117 lesser toe fusions (not exclusively in rheumatoid patients). No difference was found in terms of position, and rates of non-union and revision between buried kirschner wire and smart toe implant [40].
SURGERY TO THE MIDFOOT AND HINDFOOT
While the focus of this article is the forefoot, this cannot obviously be considered in isolation. Problems of the forefoot are combined with degenerate collapse of the midfoot and hindfoot valgus. Patients with rheumatoid arthritis develop destructive ankle disease that will lead to instability and degenerative changes. The end stage for planovalgus collapse can also result in significant degenerative ankle changes, making ankle arthroplasty and ankle arthrodesis more common procedures amongst the rheumatoid group. The rates of both of these procedures however have been declining since the 1990s [41]. Correction of hallux valgus will sometimes require lapidus arthrodesis procedure of the 1st tarsometatarsal joint for instability. Shi et al. (2000) evaluated the Lapidus procedure in 21 rheumatoid patients with good satisfaction rates and powerful initial correction reducing pre-operative hallux valgus angle from 44.1⁰ to 10.6⁰ post-operatively. At final follow-up however the angle had increased to 29⁰ [42]. A study by Popelka et al. (2008) retrospectively reviewed 143 Lapidus procedures in rheumatoid feet. This showed good correction at 6 months follow-up along with significant improvement in AOFAS scores. They noted a 4.9% non-union rate at the 1st TMTJ and a 10.5% rate of delayed wound healing beyond 21 days [43]. It is worth noting however that in this study, 14% patients underwent first MTPJ arthrodesis as well for significant hallux valgus.
CONCLUSION
Foot and ankle disease cause a significant burden on patients with rheumatoid disease. Forefoot disease in particular causes pain, callosities and possibly ulceration. Shoe wear is a significant problem. Forefoot correction in rheumatoid patients has traditionally been through excision of joints destroyed by disease. While satisfaction was historically high with this procedure changing expectations and improvement in medical therapy have raised the expectations of patients, physician and surgeon alike. Transfer metatarsalgia and non-functioning first ray are concerns with excision. Several studies have reported good outcomes with joint preserving osteotomy particularly in moderate hallux valgus disease, however there is a risk of recurrence and stiffness. Arthrodesis remains the gold standard with consistently good results. Arthrodesis carries a non-union risk of up to 8%, but gives both powerful correction and longevity in significant disease. All surgical intervention for the rheumatoid forefoot should involve a multidisciplinary approach with medical control of the disease and podiatric input to provide orthoses and surgical shoe wear.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


