All published articles of this journal are available on ScienceDirect.
The Lateral Meniscus as a Guide to Anatomical Tibial Tunnel Placement During Anterior Cruciate Ligament Reconstruction
Abstract
Purpose:
The aim of the study is to show, on an MRI scan, that the posterior border of the anterior horn of the lateral meniscus (AHLM) could guide tibial tunnel position in the sagittal plane and provide anatomical graft position.
Method:
One hundred MRI scans were analysed with normal cruciate ligaments and no evidence of meniscal injury. We measured the distance between the posterior border of the AHLM and the midpoint of the ACL by superimposing sagittal images.
Results:
The mean distance between the posterior border of the AHLM and the ACL midpoint was -0.1mm (i.e. 0.1mm posterior to the ACL midpoint). The range was 5mm to -4.6mm. The median value was 0.0mm. 95% confidence interval was from -0.5 to 0.3mm.
A normal, parametric distribution was observed and Intra- and inter-observer variability showed significant correlation (p<0.05) using Pearsons Correlation test (intra-observer) and Interclass correlation (inter-observer).
Conclusion:
Using the posterior border of the AHLM is a reproducible and anatomical marker for the midpoint of the ACL footprint in the majority of cases. It can be used intra-operatively as a guide for tibial tunnel insertion and graft placement allowing anatomical reconstruction. There will inevitably be some anatomical variation. Pre-operative MRI assessment of the relationship between AHLM and ACL footprint is advised to improve surgical planning.
Level of Evidence:
Level 4.
INTRODUCTION
Patients who have anatomical ACL reconstruction have been shown to have better function compared to those having non-anatomical reconstruction [1-3]. Accurate filling of the ACL footprint has been shown to improve antero-posterior laxity [4]. Double bundle ACL reconstruction has been shown to be biomechanically better than single bundle reconstruction at improving laxity and reducing pivot shift [5, 6] but no significant clinical difference has yet been demonstrated [7-9].
ACL reconstruction from the centre of the tibial footprint to the centre of the femoral insertion allows recreation of normal anatomy, especially in single bundle reconstruction, and it improves stability, both rotational and anteroposteriorly, so allowing improved patient functional outcome [10, 11]. Tibial tunnel malposition has been recognized as a common technical error and has been shown to significantly increase the rate of failure [12, 13].
Anatomical ACL graft placement should be performed using accurate and reproducible markers to allow accurate filling of this insertional area [10]. Placement of the ACL graft too anteriorly can cause notch impingement and placement too posteriorly will cause impingement of the graft with the Posterior Cruciate Ligament (PCL) [14].
Femoral foot print landmarks are well described. However some of the landmarks described for tibial tunnel placement, especially in the Sagittal plane, are not as robust and clinically relevant especially considering the wide variation in the footprint size and the need for individualised anatomic ACL reconstruction.
There are various bony and soft tissue landmarks described for tibial tunnel placement. The posterior border of AHLM is close to the ACL foot print and very easily identifiable during arthroscopy. Although it is described in some of the literature as one of the landmarks for tibial tunnel placement, these authors failed to find any objective data on the relationship between the posterior border of AHLM and the ACL foot print on an MRI scan, which these authors believe is clinically more relevant for individualised surgery rather than the relationship described on cadaveric studies [7, 9, 13-15].
Hypothesis
The posterior border of the AHLM is a reproducible and reliable marker for the midpoint of the ACL Tibial footprint in the sagittal plane and as such can potentially be a useful intra-operative landmark to plan and optimise tibial tunnel placement during ACL reconstruction. (Fig. 1)
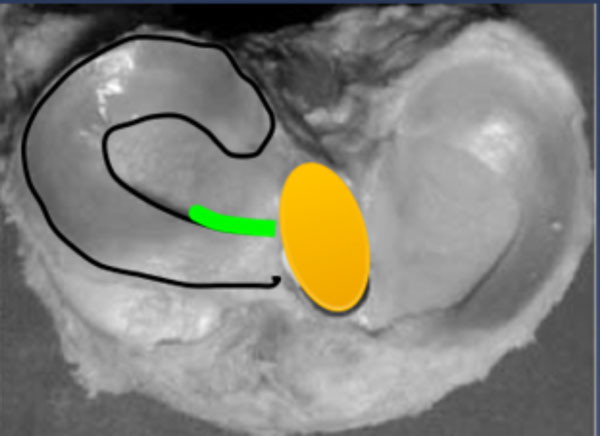
Axial slice of proximal tibia showing potential position of AHLM to tibial footprint to be investigated.

sagittal image showing posterior border of the AHLM.
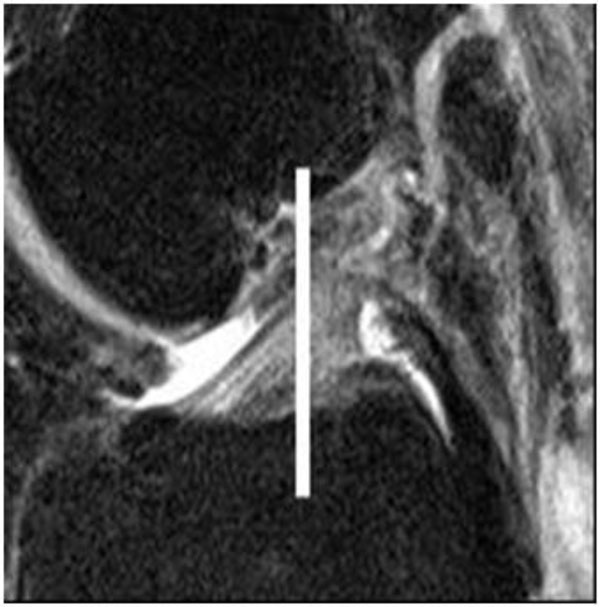
Sagittal image showing midpoint of ACL tibial footprint.
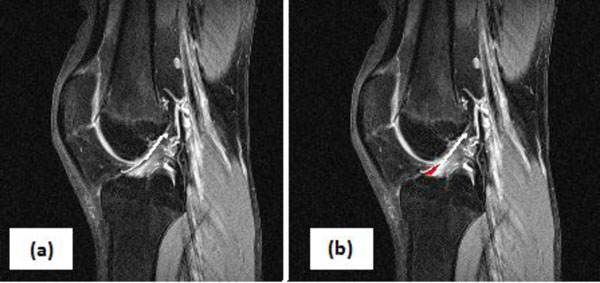
(a) Marking of anterior border of proximal ACL (b) Following border down to delineate the anterior flare (marked in red) which is to be avoided in calculations.
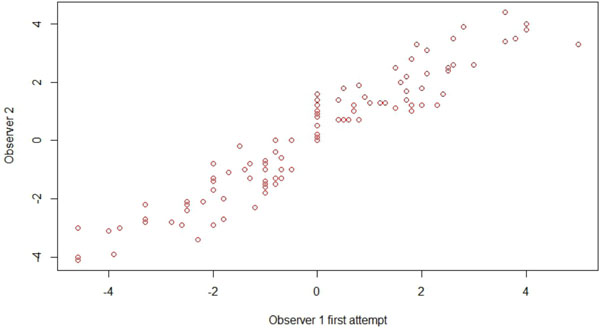
Intra-observer variability.
Distance between posterior border of AHLM and midpoint of tibial footprint using students T-test.
| Mean Difference (mm) | 95% Confidence Interval of the Difference | ||
|---|---|---|---|
| Lower | Upper | ||
| Distance between posterior border of AHLM and midpoint of ACL footprint | -0.10 | -0.52 | 0.32 |
Summary of literature for markers of ACL footprint position.
| Author | Marker | Detail |
|---|---|---|
| Zantop et al. [2] | Anterior insertion of Lateral Meniscus (LM) | Anterior insertion of LM 11.2mm (+/- 1.2mm) anterior and 4.1mm (+/- 0.6mm) laterall to posteriolateral bundle of ACL |
| Ziegler et al. [3] | LM | LM is 7.5mm (+/- 0.5mm0 lateral to ACL in coronal plane |
| Luites et al. [17] | Medial Tibial Spine (MTS) | ACL is 5.1mm (+/- 1.7mm) lateral and 9.8mm (+/- 2.1mm) anterior to MTS |
| Edwards et al. [19] | Over the back ridge of knee | PL bundle of ACL is 10mm (+/-1 mm) anterior to over the back ridge |
| Edwards et al. [19] | MTS | Distance between laterla border of MTS is 4mm (+/- 1 mm) to the PL fibre bundle and 5mm (+/- 1 mm) to the AM bundle |
| Jackson et al. [18] | PCL | Midpoint of ACL footprint is 7mm anterior to anterior border of PCL |
| Kongcharoensombat et al. [21] | Transverse ligament | Transverse ligament is 18.7% (+/- 3.3%) of sagitall wdth of tibia from midpoint of ACL footprint |
| Ferretti et al. [22] | Intermeniscal ligament and medial tibial eminence | ACL centre 9.1mm (+/- 1.5 mm) posterior to the intermeniscal ligament and 5.7mm (+/- 1.1 mm) anterior from apex of the medial tibial eminence |
PATIENTS AND METHODS
After receiving institutional review board approval, one hundred anonymised MRI scans of adult knees were analysed using the Philips Radio-Viewer (accurate to 0.1mm). All MRI’s at the authors’ institution are performed with a standardized protocol and positions of the knee. Inclusion criteria were all adults (over age of 16) with an MRI scan reported by a Consultant Radiologist as having no cruciate ligament injury (either ACL or PCL) nor any meniscal or collateral injuries. The database was obtained from anonymised, consecutive scans performed in the Radiology department at the authors’ institution. Exclusion criteria included any scans with any multi-ligament injury, prior meniscal or ACL surgery or injury or patients with significant osteoarthritis.
Standardised protocols were used for all MRI scans and there was no evidence of rotation on any scans. T2 weighted coronal and sagittal images were used. The posterior border of the anterior horn of the lateral meniscus was marked on the sagittal image immediately lateral to the ACL tibial foot- print. The two points were normally separated by 2 MRI slices (approximately 7mm distance in coronal plane) (Fig. 2).
The midpoint of the ACL footprint (in the sagittal image that showed the maximal width) was marked on another sagittal image (Fig. 3). These two images were superimposed to establish the relationship between the marked points.
The midpoint of the ACL was measured excluding the anterior flare of the ACL at the tibial footprint, which is part of the normal anatomy of the ACL [15]. The distal ACL flares anteriorly to accommodate the contour of the intercondylar roof when the knee is extended [11, 16, 17]. A tubular graft is unable to replicate this flare and if the flare is accounted for in calculations, there is a potential for placement of the graft too anteriorly so causing impingement of the graft in the intercondylar roof on extension [5]. On a high resolution computer, the anterior flare is easily identified on the sagittal view by delineating the anterior border of the proximal ACL and following this line distally. As the midpoint of the ACL border is reached this line should be continued in its pre-determined direction to avoid the anterior flare (see Fig. 4). Calculations were performed by two Specialist Registrars in Trauma and Orthopaedic Surgery using the same protocol.
Intra-observer variability was measured by repeat assessment of the same scans two weeks later by the same observer. Inter-observer variability was assessed by a second investigator independently reviewing the same scans.
For the purposes of calculation, a positive value implied that the posterior border of the AHLM was anterior to the midpoint of the ACL footprint. Conversely, a negative value was used to show the border being posterior to the midpoint of the footprint.
Statistical Analysis
Statistical analysis was conducted using the Statistical Package for the Social Sciences version 13.0 (SPSS Inc, Chicago, IL, USA). Sample size was determined with an effect size of 5mm and a power calculation of 90% with Type 1 error of 5%. This required a sample size of 71 and this was subsequently rounded up to 100 to further power the results.
Distances between the AHLM and the midpoint of the ACL footprint were compared using students T-Test. Comparison of the differences between the intra-observer groups was performed using the Pearsons correlation test, while Interclass Correlation was applied to compare differences between observers (inter-observer correlation). In all the tests, an alpha level of 0.05 was considered to be significant.
RESULTS
The average age of the patient presenting for the MRI scan was 37.6 years (Range 16-80). The scan cohort included 52 males and 48 females with scans of 45 left knees and 55 right knees.
Scans demonstrated that the posterior border of the AHLM lies, on average, 0.1mm (mean = –0.1mm) posterior to the midpoint of the ACL footprint (range 5mm to - 4.6mm). The median distance is 0.00mm with a 95% confidence interval of 0.32:-0.52 (Table 1).
Repeat measurements taken 2 weeks later, by the same investigator, using the same scans, showed an average distance of 0.0mm with significant correlation (p<0.05) between the 2 measurements (Pearson Coefficient 0.95). Thus no significant intra-observer variability is demonstrated.
Our second investigator assessed the mean distance between the posterior border of the AHLM at the midpoint of the ACL was 0.8mm (i.e. 0.8mm anterior to the midpoint of the ACL) with a ANOVA Interclass correlation coeffi- cient (F) of 9.93 which was significant (p=0.002, Fig. 5).
DISCUSSION
To the authors’ knowledge, this is one of the only studies assessing the position of the ACL footprint in relationship to the posterior border of the anterior horn of the lateral meniscus on an MRI scan. Our results have shown that the posterior border of the Anterior Horn of the Lateral Meniscus (AHLM) is closely related with the centre of the ACL footprint in the sagittal plane (average 0.1mm posterior) with low variance (up to 5mm). The AHLM is easily visible during arthroscopy and is rarely damaged either during the initial injury or during the operative procedure. We can therefore deduce that the posterior border of the AHLM is a pertinent arthroscopic landmark for the positioning of the tibial tunnel.
Zantop et al. found, in a cadaveric study, that the anteromedial bundle of the ACL aligns with the centre of the anterior horn of the lateral meniscus and centre of the posterolateral bundle was located 11.2 mm (+/- 1.2) posterior and 4.1 mm (+/- 0.6) medial to the anterior insertion of the lateral meniscus (2). This helps validate our findings and we believe that the posterior horn of the AHLM is an accurate marker for the midpoint of the footprint to allow accurate placement of both AM and PL bundles.
Our study has shown that the AHLM correlates closely with the midpoint of the ACL footprint in the sagittal plane. It has already been shown that the AHLM is beneficial in allowing placement of the ACL graft in the coronal plane [18]. Zeigler et al. have also measured the distance from the lateral meniscus to the centre of the ACL footprint in the coronal plane and have shown it to be 7.5mm +/- 0.5 [3]. These markers can be used in conjunction with our findings (which show the distance between AHLM and ACL midpoint in the sagittal plane), to allow anatomical placement of the graft intra-operatively, in both the sagittal and coronal planes, to reduce the risks of graft impingement, graft failure and poor functional outcome.
The AHLM can allow an anatomical ACL reconstruction, which is specific and accurate for each individual patient, by allowing pre-operative assessment and planning to confirm the position in relation to the ACL tibial footprint. This planning will allow intra-operative, anatomical tibial tunnel placement to allow a more accurate and anatomical ACL reconstruction thus improving patient outcome including prior to revision ACL reconstructions when other anatomical markers (medial tibial spine, ACL remnant) are unlikely to be present so making anatomical ACL reconstruction difficult. In the majority of cases the posterior border of AHLM is closely related to the centre of the ACL foot print but there are circumstances where it is either too anterior or too posterior and identifying this variation preoperatively on MRI scan will help to place the tibial tunnel in the true anatomic centre for each individual patient.
A decision was taken to perform an MRI study, instead of a cadaveric study, as MRI is the commonest pre-operative investigation performed for both primary and revision ACL reconstruction. Identification of the relationship between the lateral meniscus and the centre of the ACL footprint on an MRI scan rather than in a cadaver is clinically and surgically relevant, for individualized anatomical ACL reconstruction, as this would allow planning of surgical graft placement pre- operatively and intra-operatively.
Various landmarks for placement of the ACL graft on the tibia have been described in the literature and these are summarized in Table 2. Luites et al. have shown, in a cadaveric study, that the ACL centre is 5.1mm (+/- 1.7mm) lateral and 9.8mm (+/- 2.1mm) anterior to the medial tibial spine [17]. Edwards et al. [19] have also suggested, in cadaveric, dis-articulated knees, that the over the back ridge of the knee along with the medial tibial spine are markers for tibial graft placement. These are difficult to identify intra- operatively as both are routinely covered by the ACL remnant and identification requires clearance of this. This is not routinely recommended as the torn remnant contains mechanoreceptors and proprioceptive fibres, which can improve post-operative proprioception and functional recovery [13, 20, 23]. This makes the medial tibial spine a difficult anatomical landmark to identify and utilise as a marker intra-operatively in all cases.
The Posterior Cruciate Ligament (PCL) has been used as a guide to ACL graft positioning. The posterior border of the ACL footprint has been shown to be 7mm anterior to the PCL but this does not give a measurement to the centre of the ACL footprint and so would not allow anatomical filling of the centre of the footprint. There would be a significant risk that, using the PCL as a marker, the graft would be placed too posteriorly in the knee and would risk impinging on the PCL or creating a more vertical graft, which would have increased risk of failure [18].
The PCL can be difficult to visualize due to fat covering its anterior border and any anterior translation of the tibia can change the relationship between the PCL and ACL footprint. Any translation as a result of ACL injury will not have an effect on the relationship between the AHLM and the ACL footprint.
A recent MRI study [10] studied the position of the ACL and its centre in relation to the width of the tibia in the sagittal plane. The authors concluded that the centre of the ACL is measured at 46 +/- 4 % of the total sagittal width of tibia. This measurement is useful as a preoperative and post operative assessment of tibial tunnel placement but does not help intraoperative positioning of the ACL graft. Other studies have also attempted to describe the position of the ACL in relation to the sagittal width of the tibia and identified differing results. Takahashi et al. found that the AM and PL bundle centres around 29 and 32% of the overall AP width of the proximal tibia [9], whereas Staubli and Rauschning found the overall centre of the ACL tibial attachment at 43% in their cryosections [24]. Edwards et al. [19] reported the bundle centres at 29 and 46%, and the centre of the ACL attachment at 36% of the AP depth of the tibia. All these results show a large variation in the values and so are difficult to interpret accurately and utilise.
Anatomical variance is to be expected with a range of tibial footprint sizes described in the literature [19]. Our results have shown that the midpoint of the ACL footprint can be up to 5mm from the posterior border of the AHLM. This can easily be identified on pre-operative MRI scan and the authors would recommend review of the lateral meniscus on pre-op MRI and correlation to the ACL stump. This will allow accurate assessment of the posterior border of the AHLM to the midpoint of the ACL allowing accurate graft placement intra-operatively for each individual patient.
Our method involved excluding the anterior flare of the ACL at the tibial footprint which is part of normal knee anatomy and allows the knee to extend fully without any ACL impingement on the femur [5, 11, 25]. If the anterior flare was included in the calculations, there would be a risk of graft placement too anteriorly, especially if the graft is covering the majority of the footprint or whilst performing AM bundle reconstruction. This would increase the risk of graft impingement in knee extension and, subsequently, graft failure [6].
The embryologic development of the lateral meniscus is closely related to that of the ACL and occurs from the same blastoma. As a result, the attachments of the lateral meniscus are quite consistent with those of the ACL [26-28]. This is very relevant in view of wide variety of size and shapes of the ACL tibial footprint [17].
LIMITATIONS
This is a retrospective study assessing sagittal MRI images only. No correlation between the AHLM and ACL footprint is made on any coronal images. No intra-operative measurements were made of the relationship between the posterior border of AHLM and the midpoint of the ACL footprint. As with much of the literature on anatomical ACL reconstruction, no clinical results are available to suggest that anatomical tibial tunnel position correlates with improved clinical outcomes or improved patient functional improvement.
These measurements are taken from MRI scans of intact ACL’s. We are currently investigating the relationship and ease of calculations in an ACL deficient knee to help further our knowledge of optimum tibial tunnel placement. We are also planning a study to assess position of the tibial tunnel post-operatively using our AHLM measurements.
CONCLUSION
The posterior border of the AHLM is an easily identifiable (both pre-operatively on an MRI scan and intra- operatively) and reproducible marker for the middle of the ACL footprint. It is located on average 0.1mm posterior to the middle of the ACL footprint with low variance (+/- 5mm). This relationship can be studied and planned pre- operatively and its position utilised intra-operatively to allow individualised, anatomical placement of the tibial tunnel.
We recommend assessment of the pre-operative MRI to assess the position of the AHLM in relation to the ACL stump. Our results have shown that the ACL tibial footprint can be up to 5mm anterior or posterior to the AHLM and this position can be calculated pre-operatively on the MRI scan and then used intra-operatively to create the tibial centre in a patient specific, anatomical position.
CONTRIBUTORS
AM Kassam – Study design, Data acquisition and analysis, Manuscript preparation.
L Tillotson – Data acquisition and analysis, Manuscript preparation.
PJ Schranz – Study design, Data acquisition and analysis, Manuscript preparation.
VI Mandalia – Study design, Data acquisition and analysis, Manuscript preparation.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Dr. Doyo Gragn Enki, Statistician, University of Plymouth, 1 Davy Road, Plymouth, PL6 8BX.


