All published articles of this journal are available on ScienceDirect.
Bilateral Simultaneous Total Knee Arthroplasty: A Patient-Matched Retrospective Observational Study
Abstract
Bilateral total knee arthroplasty can be performed either as a staged or simultaneous procedure. We conducted a retrospective comparative study to compare the need for transfusion, the length of procedure, the length of stay, and complications of bilateral simultaneous knee arthroplasty with those of unilateral knee arthroplasty. Sixty-nine patients who underwent bilateral simultaneous knee arthroplasty procedures were compared with a matched control group of 69 patients who underwent unilateral knee arthroplasty. Receiver Operating Characteristic (ROC) curve was used to determine optimum cut-off values. Both groups of patients had a similar age and gender distribution, preoperative haemoglobin and ASA scores. Cumulative transfusion episodes were lower in the bilateral group than twice that of the unilateral group. In multivariate analysis the preoperative haemoglobin level and bilateral procedures were independent factors predicting the need for transfusion. The average length of procedure and length of hospital stay in the bilateral group was less than twice than that of the unilateral group. Advanced age and bilateral procedures were independent predictors of prolonged length of stay. A haemoglobin level of 12.5 g/dL and age of 70 were most suitable cut-off points to predict need for transfusion and occurrence of medical complications respectively. We conclude that bilateral simultaneous knee arthroplasties are safe and cost effective in appropriately selected patients. We recommend avoiding bilateral simultaneous procedures in patients over the age of 70 years and with significant comorbidities.
INTRODUCTION
Total knee arthroplasty is a safe and effective treatment for end stage knee osteoarthritis [1-3]. When painful osteoarthritis occurs in both knees, bilateral procedures can be performed either simultaneously under the same anaesthetic or as staged procedures with two separate anaesthetics. Bilateral simultaneous knee arthroplasty (BSKA) decreases the cumulative length of stay in the hospital [4, 5]. It has also been shown to be associated with higher patient satisfaction [6] and convenience [7], quicker return to function [4], lower costs [5, 8] and decreased reimbursement [9] compared with bilateral staged knee arthroplasty.
Although several reports have shown similar rates of complications and morbidity [5, 6, 10, 11], concerns about increased intraoperative and postoperative complications with BSKA are debated. Higher rates of postoperative confusion [12, 13], cardiac complications [6, 12, 13], and need for blood transfusion [13] have been reported in the literature. We performed a retrospective study to compare the rate of perioperative complications and morbidities of BSKA versus unilateral knee arthroplasty (ULKA).
PATIENTS AND METHODS
The study was given as an exempt status by the Homerton University Hospital Institutional Review Board because all data were retrieved confidentially from hospital records and no change in patient management or any form of patient contact was needed for the purpose of this study. During the study period 69 BSKA and 554 ULKA procedures were performed. All patients who underwent BSKA were included in the study. For comparison an age-, gender- and risk factor-matched second group of consecutive 69 patients who had undergone the unilateral procedure was chosen. Data were retrieved from Homerton University Hospital’s Electronic Patient Record (EPR) system and electronic discharge summaries. The collected data included patients’ age and gender, past medical history, American Society of Anesthesiologists (ASA) grade, operation date, use of drain, length of procedure, preoperative and postoperative haemoglobin, need for Intensive Therapy Unit (ITU) admission, length of inpatient stay, and complications.
All patients underwent the standard identical preoperative, intraoperative, and postoperative protocols used for knee arthroplasty. Preoperatively patients underwent clinical and radiological assessment. The procedures were performed under general anaesthesia following informed consent. For the BSKA procedures, both legs were prepared simultaneously by two operative teams including surgeon, assistant and scrub nurse on each side. All procedures were performed using NexGen (Zimmer Inc., Warsaw, IN, USA) implants through the medial parapatellar approach. Patients were discharged home after they were deemed safe for discharge by the occupational and physiotherapy teams. The occupational therapy team and the physiotherapists supervised the continued rehabilitation by home visits. All patients had clinical and radiological follow-up at six weeks and three months postoperatively. Radiographs were obtained before discharge and as needed postoperatively.
Statistical analysis was performed using the SPSS software. Data was checked for normality using Q-Q Plot analysis. Student t-test was used for parametric data. Mann-Whitney test was used to compare the outcomes for non-parametric data for independent samples. Chi square test was used for categorical data. Logistic regression analysis was used to identify the factors that predicted increased length of stay (defined as stay longer than nine days postoperatively) and need for transfusion. Receiver operating characteristic (ROC) curve analyses was used to determine whether preoperative haemoglobin level could effectively be used to predict the need for transfusion [14]. This method assesses the diagnostic strength of a test and calculates the best cut-off point for differentiating between a positive and a negative test result. Sensitivity is plotted against 1-specificity and the area under the curve (AUC) is calculated from the plot. An AUC of 0.5 indicates that a test has no diagnostic strength; as the AUC increases to a maximum of 1, the diagnostic strength improves. A test with an AUC greater than 0.9 is considered an excellent diagnostic test. Youden’s J statistic was used to determine optimum cut-off values for predicting the need for transfusion. According to this rule, a test’s best diagnostic threshold occurs at the value for which the sum of the test’s sensitivity and specificity is maximized. A p value of less than 0.05 was considered significant.
RESULTS
Sixty-nine patients were included in each group (22 males and 47 females). Details of the patients’ demographic data, ASA grade and Charlson score, length of procedure, preoperative haemoglobin, haemoglobin drop (checked 24-48 hours postoperatively), need for transfusion, ITU admission and length of stay are summarized in Table 1. Medical complications are summarized in Table 2.
Transfusion rate was higher in the BSKA group (36%) than in the ULKA group (20%) (Table 1). After adjustment for relevant factors, results of logistic regression analysis showed that preoperative haemoglobin (p< 0.001; OR=0.35; CI=0.23-0.56) and BSKA (p=0.03; OR=0.15; CI=0.03-0.85) were the only factors that had a significant effect on the need for transfusion. ASA grade, age, gender, length of procedure, and use of drain did not show a statistically significant effect on the need for transfusion. ROC analysis further confirmed the diagnostic capability of preoperative haemoglobin level in predicting the need for transfusion. The AUC was above 0.80 in both groups, indicating a high-strength diagnostic test (Fig. 1). ROC curve analysis demonstrated an AUC of 0.84 (95% CI = 0.74-0.94) for BSKA, and 0.81 (95% CI=0.70-0.91) for ULKA. The optimum haemoglobin threshold in predicting the need for transfusion was 12.75 g/dL (sensitivity 80.0%, specificity 70.0%) for BSKA, and 12.20 g/dL (sensitivity 86.0%, specificity 73.0%) for ULKA.
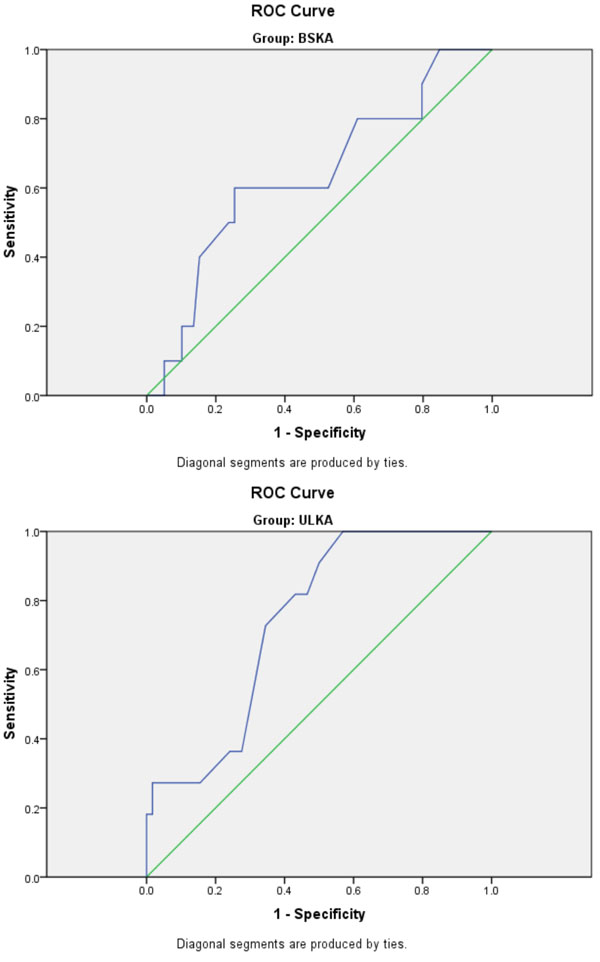
Receiver operating characteristic (ROC) curves are shown for (A) BSKA; (B) ULKA.
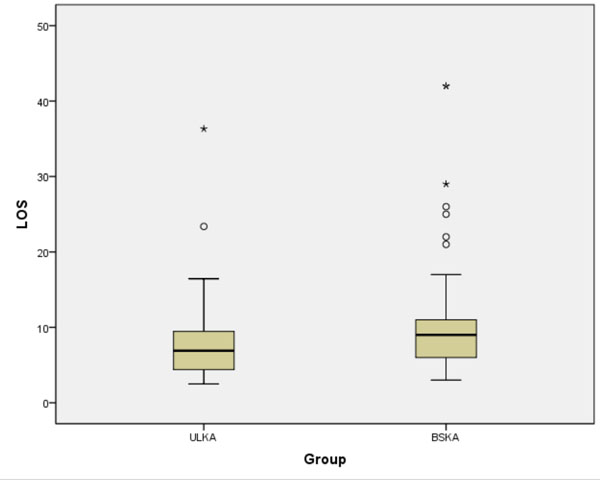
Box plot graph showing the length of stay for 2 groups (one case with length of stay =157 days was not included as it would distort the graph dimensions).
Demographic data and incidence of need for blood transfusion and ITU admission in both groups.
| ULKA | BSKA | P | Confidence Intervals | ||
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| Age mean (SD) | 67.65 (9.57) | 65.88 (9.79) | 0.29* | -1.49 | 5.03 |
| ASA grade (1,2,3) | 3,38,28 | 3,48,18 | 0.19£ | 0.18 | 0.20 |
| Charlson (0,1,2) | 3,58,8 | 0,65,4 | 0.08 | 0.07 | 0.09 |
| Pre-op haemoglobin | 12.8 (1.40) | 12.8 (1.54) | 0.89* | -0.53 | 0.46 |
| Length of procedure in minutes (SD) | 90 (33) | 141 (66) | < 0.001* | -70.00 | -33.31 |
| Haemoglobin Drop | 3.59 (1.07) | 3.78 (1.34) | 0.35* | -0.60 | 0.21 |
| Transfused | 14 (20%) | 25 (36%) | 0.04£ | - | - |
| ITU admission | 2 | 3 | 0.5$ | - | - |
| length of stay (Range) | 6.9, 3-36 | 9, 3-157 | 0.005† | ||
* = independent t test, £= Chi square test, $= Fishers exact test, †= Mann Whitney U Test, SD=Standard deviation, ASA= American Society of Anaesthesiologists, ITU= Intensive Therapy Unit.
Summary of medical complications.
| ULKA | BSKA | |
|---|---|---|
| MI/arrhythmia | 1 | 2 |
| ITU | 2 | 3 |
| Prolonged ITU | 1 | 1 |
| LRTI | 3 | 5 |
| AKI | - | 2 |
| Ileus/constipation | 2 | 1 |
| Confusion | 2 | 1 |
| CVA | - | 1 |
| UTI | 1 | - |
| PE | 3 | 0 |
| GI bleed | 1 | - |
| Total | 16 | 16 |
| Patients* | 11 | 10 |
*= Total number of patients in which the complications occurred, MI= Myocardial infarction, ITU= Intensive therapy Unit, LRTI= Lower Respiratory tract Infection, AKI= Acute Kidney Injury, CVA= Cerebrovascular Accident, UTI= Urinary Tract Infection, PE= Pulmonary Embolism, GI= Gastrointestinal.
The median length of stay was seven days in the ULKA group and nine days in the BSKA group. One patient in the BSKA group had a prolonged stay of 157 days due to a postoperative lower respiratory tract infection and atrial fibrillation requiring anticoagulation, and subsequent unilateral wound infection necessitating removal of the implant. The length of stay had an abnormal distribution in both groups (Fig. 2), ranging from 3-157 days. This difference was statistically significant (p= 0.005; Mann-Whitney Test). Prolonged length of stay (defined as stay longer than 10 days) was seen in 17% of the UKLA patients and 29% of the BSKA patients. The cumulative length of stay for all patients was 532 days for the UKLA group and 884 days for the BSKA group. The results of binary logistic regression analysis showed that age (p<0.001, OR=1.12, CI=1.06-1.19) and BSKA procedure (p=0.04, OR=0.39, CI=0.16-0.95) were independent predictors of increased length of stay. Gender and preoperative haemoglobin did not have a significant effect.
Two surgical complications were seen in the BSKA group including one case of foot drop due to peroneal nerve palsy that was treated non-operatively and the weakness partially resolved without a brace at one year follow up. There was also one case of deep infection that needed revision. Medical complications occurred in 21 patients. One patient in the ULKA group developed bilateral pulmonary emboli despite mechanical and chemical prophylaxis and subsequently developed upper gastrointestinal bleeding. An inferior vena cava filter was inserted and patient was discharged. One patient in the BSKA group with a prolonged length of stay is discussed above. The full list of medical complications is summarized in Table 2.
A haemoglobin level of 12.5 g/dL and age of 70 were most suitable cut-off points to predict need for transfusion and occurrence of medical complications respectively.
DISCUSSION
We report a comparison of outcomes of a series of 138 patients (207 knees) who underwent BSKA or ULKA at our institution. Patients undergoing ULKA would have the same risks and complications at their subsequent admission when they undergo a surgery for their contralateral knee, unlike BSKA patients [15].
In our series the preoperative haemoglobin was 14.1g/dL for males and 12.4 g/dL for females. Forty-seven percent of females and 14% of males in the BSKA group needed blood transfusion whilst 28% of females and 5% of males needed blood transfusion in the ULKA group. The higher transfusion rate in females is possibly due to the lower preoperative haemoglobin. Although higher transfusion rate was seen in patients undergoing BSKA (36%), the cumulative number of transfusions needed was less than twice that of the ULKA group (20%). On multivariate analysis preoperative haemoglobin and BSKA procedure were independent factors predicting the need for transfusion. Although both groups had similar preoperative haemoglobin and haemoglobin drop levels, the higher need for transfusion in the BSKA group may be explained by the increased variance in haemoglobin drop (SD 1.03 vs 1.34).
Jankiewicz et al. [11] suggested a more invasive preoperative workup and use of preoperative marrow stimulants and autologous blood transfusion might reduce the need for homologous blood. Preoperative autologous donation was also suggested by Cushner et al. [16]. Transfusion rates as low as 5% have been reported by Nikki et al. [17]. These authors suggested that postoperative drain clamping and tranexamic acid administration were the main causes for reduced blood transfusion rates in their series. A combination of different strategies including preoperative injections of bone marrow stimulants [18], routine use of auto-transfusion and tranexamic acid, and rapid recovery pathway [19] have a role in reducing transfusion requirements.
The length of the procedure has been shown to be a predictor of prosthetic joint infection [20, 21]. Ritter et al. [22] reported higher risk of medical complications, but interestingly lower wound infection rates with the bilateral procedure. We believe that performing the bilateral procedure simultaneously decreases the cumulative operating time and hence should reduce the infection rate. Postoperative infection however is multifactorial and we found no significant difference between the two groups of relatively small number of patients. Large randomised trials are needed to evaluate the effect of cumulative procedure length on infection rate.
Advanced age and BKSA procedures were independent predictors of prolonged length of stay. Assuming that patients would have a similar length of procedure and length of stay in the hospital if they needed arthroplasty of the other knee, the average length of procedure would be 39 minutes shorter and the average length of stay would be 4.8 days shorter for BSKA. This would result in significantly reduced costs. Although this economic assessment is rather simplistic as it does not consider hidden community costs which are difficult to determine [23], theatre time and length of stay are considered to be the largest contributors to the total cost [24].
Although two surgical complications were seen in the BSKA group and none in ULKA group, one case was due to patient anticoagulation following a medical complication. We do not believe that BSKA procedure has a negative effect on surgical complications. Advanced age is another factor that has been implicated in increasing complications after BSKA. Adili et al. [25] reported increased risk of cardiovascular complications in a group of 82 patients aged 75 or more. Dennis [26] suggested avoiding the procedure in patients older than seventy years of age. In our patients ROC analysis showed an AUC of 0.68 (CI=0.56-0.80) with optimum age of 70.5 years to give a sensitivity of 67.0% and specificity of 69.0% to predict medical complications. Although the cumulative medical complications were lower for BSKA, the complications were more severe and ITU stays were longer. We found patients with pre-existing cardiopulmonary disease were at increased risk of cardiovascular complications, consistent with published literature [6, 13].
The strength of our study was accurate and prospective documentation in the EPR system. The postoperative course and patients’ medical problems and medications were available in the electronic discharge summaries. Our study does have limitations. The retrospective nature of the study increases the risk of selection bias. The bilateral operation was offered to patients who were deemed fit for the procedure by the anaesthetists and patients with ASA score of greater than 3 were excluded. In an attempt to overcome this issue we compared the variables of interest to our matched control group but it would not be possible to omit the potential confounders that we were unaware of.
In conclusion, BSKA seems to be a safe procedure and is not associated with increased surgical risks. We recommend selecting patients carefully, and avoiding BSKA in patients with advanced age and significant comorbidities.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We thank Mr. Abdulkarim Zurgani for allowing us to use his patients’ data for this study.


