All published articles of this journal are available on ScienceDirect.
Single Stage Knee Arthroplasty Revision Surgery: A Systematic Review of the Literature
Abstract
Total Knee Arthroplasty is an increasingly common procedure and revision surgery, particularly for infection, is associated with significant morbidity and healthcare costs. The current gold standard is a two stage revision procedure but single stage revision is increasingly being used in some departments to improve patient outcomes. We conducted a systematic review of the literature to determine the up-to-date evidence underlying the use of a single stage knee approach in revision surgery. A total of 12 studies were included in this review amounting to 433 revision surgeries. This is the largest review of single stage knee revision surgery. The procedures described were heterogenous and included the ‘two-in-one’ technique as well as other single stage revision procedures. There were also differences in implants and antibiotic regimens. The mean re-infection rates described in 10 studies was 9.4% (range 0-19.2%) after a mean follow-up of 40.3 months (range 7-180 months). The re-infection rates in the studies published over the last 30 years are falling, and this is not accounted for by any significant change in duration of follow-up during this period. The outcome scores varied, but patients generally showed an improvement. The Knee Society Score and the Oxford Knee Score were the most commonly used in five and three studies respectively. We conclude that the current evidence for single stage revision is variable and there is a lack of good quality evidence to address whether single stage revisions is thorough enough to eradicate deep infection and is able to restore adequate function. There is a need for larger prospective studies with standardised procedures and protocol, and with adequate follow-up. Till then, patients considered for a single stage approach should be thoroughly assessed and the surgery should be performed by a senior surgeon with experience in single stage knee revisions.
INTRODUCTION
The management of an infected Total Knee Arthroplasty (TKA) is a challenging process [1]. Although most studies globally report primary infection rates of about 2% [2-4], this still represents a significant burden on the NHS that performed 86,000 primary TKAs in 2013, a significant rise compared to 74,000 in 2007 [5]. The latest figures for knee revision surgery in England are 2749.2 per 1000 patients at risk [6]. However, the National Joint registry also reported a total of 6,009 knee revision procedures in 2012 with infection representing 23% of cases, an increase of 17% compared to 2011 [7]. Alongside the rising incidence of knee revisions, the cost of revision surgeries also posts a significant burden on the NHS with some studies estimating a cost of £75,000 per patient [8, 9]. A recent study comparing aseptic and septic knee revisions showed that the mean cost of a revision for infection was associated with a hospital stay that was twice as long and costs three times as much [10].
The current gold standard of revision surgery is a two stage process that has a re-infection rate of 0-41% [11], andis performed in three phases: (1) Debridement of the soft tissues and removal of the prosthesis and cement, (2) Two to six weeks of parenteral antibiotic therapy to treat the infection, and (3) Implantation of a new TKA. The goal of treatment is to eliminate the underlying infection and pain, restoring function back to the affected joint. However, it still remains a costly procedure that not only includes replacement of the prosthesis but extended in-patient stays and extensive drug therapy and monitoring. Considering that the average age of a patient who undergoes a primary TKA in the UK is 70 with multiple co-morbidities [6], it is paramount for the orthopaedic surgeon and the respective healthcare institutions to determine the most efficient management solution. Single stage knee revision is increasingly, routinely used in some departments to improve patient outcomes. We conducted a systematic review of the literature to determine the up-to-date evidence underlying the use of a single stage knee approach in revision surgery.
MATERIALS AND METHODS
A systematic review of literature was performed on 31 March 2015 to identify studies that had analysed single stage revision arthroplasties. MEDLINE was the database of choice and assessed via PubMed. The key words used to perform the search were “single-stage”, “one-stage”, “direct”, “knee revision”, “knee arthroplasty” and “infection”. Due to the small amount of evidence available, all the studies from 1985 onwards, including any non-English studies were included. The information obtained were: gender distribution, age range, procedure, total number of knees, type of procedure, average follow up period, re-infection rate, functionality and range of movement. Reports that considered both two stage and one stage revisions had the one stage data extracted and listed in the tables below by one of the authors (E.C.). The tables were then vetted by a second author (W.S.K.). A meta-analysis was not performed due to the clinical heterogeneity of the studies.
RESULTS
A total of 12 studies were included in this review amounting to 433 revision surgeries [12-23]. The demographic details and details of the procedures performed are included in Table 1. Table 2 outlines the outcomes for the studies. The patient age range was from 47-89 years with an average age stated by some studies from 61.4-70.7 years. The studies which provided information on gender distribution generally had more female than male participants apart from one study [21].
Procedures Performed
Table 1 outlines the procedure carried out in the included studies where details were provided. The single stage revision procedure generally involves removal of the implant followed by extensive debridement of the soft tissues and direct re-implantation of the new prosthesis. Bone cement augmented with appropriate antibiotics is usually used and the patient is placed on a six week post-operative antibiotics regime. The possible benefits include a faster recovery of function, shortened hospital admission and a reduced exposure to surgery. However, procedures tend to differ across centres. The study conducted by Parkinson et al. used a ‘two-in-one’ technique which is similar to a two-stage procedure but the second stage immediately follows the first. In between stages the patient is re-draped, the surgeon re-gowned and the instruments replaced [19]. Whiteside et al., reporting on 18 knees infected with Methicillin Resistant Staphylococcus aureus (MRSA), also had a different technique that involved an uncemented revision of total knee components followed by an intra-articular infusion of 500mg of vancomycin via a Hickman catheter once or twice daily for six weeks. The infection rate of the former study was 0% and the latter 5.6% with a follow up period of 24 and 62 months, respectively. A significant proportion of studies failed to indicate the details of the procedure that was used.
Re-Infection Rates
Table 2 outlines the outcomes including re-infection rates in the included studies where details were provided. This varied from 0-19% in the 10 studies that provided this information. A major concern with single stage approaches is the ability to successfully eradicate underlying infection. The current gold standard is a two stage approach but it has a very variable re-infection rate of 0-41% [11]. The number of studies conducted using the two stage approach vastly outnumbers the single stage approach.
In this review, a total of 10 studies were eligible for analyses. The largest study that focused primarily on re-infection included 104 patients at Endo-Klinik in Germany with an infection rate of 19% over a follow-up period of 5-15 years [13]. Goksan et al. analysed 18 patients of which, 10 had a diagnosis of rheumatoid arthritis and six patients were on corticosteroids [14]. All of the patients involved had a gram positive infection and the patients with rheumatoid arthritis had additional risk factors with another focus of infection and skin necrosis. The study reported two knees developing a recurrence of infection (11%). However, the authors made it clear that both patients were immunosuppressed and only one patient was proven to have a recurrence of the same organism. A literature review comparing infection rates of single stage revisions with arthroscopic debridement and open debridement also produced similar results of 10.8%, 47.8% and 67.4% respectively [15]. The latest studies were performed by Tibrewal et al. [22] and Haddad et al. [23] with re-infection rates of 2% and 0%, respectively. Other smaller retrospective studies till date have shown rates of between 0%-10% [15, 20, 22-24].
If we look at re-infection rates across all ten studies that provided the data, this is 33 cases out of 352 (9.4%) after a mean follow-up of 40.3 months. If we exclude the Endo-Klinik study that had the highest number of re-infections but also one of the longest follow-up [13], we have 13 cases out of 248 (5.2%) after a mean follow-up of 27.5 months. We plotted the re-infection rates against year of publication (Fig. 1), and the graph suggests that re-infection rates are falling. We wanted to determine whether these better results are due to a shorter follow-up. We also plotted the mean follow-up rates for these studies against year of publication (Fig. 2), and the graph suggested that the mean follow-up has not significantly changed over the time period of the studies. This suggests that the re-infection rates in the studies published over the last 30 years are falling, and there has not been any significant change in duration of follow-up. Fig. (3) demonstrates that the longer the follow-up, the greater the re-infection rate.
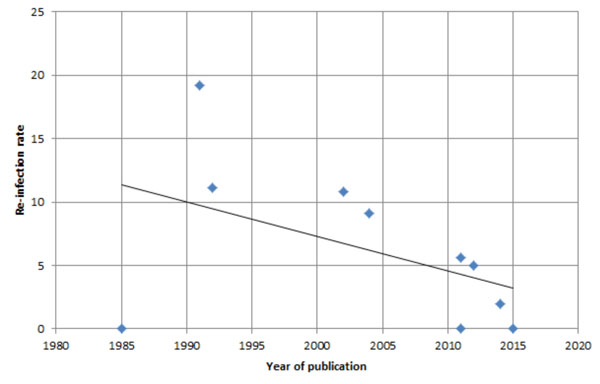
A graph demonstrating the re-infection rates (y-axis) for studies where the data was available, plotted against year of publication (xaxis). The line of best fit suggests that re-infection rates are falling with time.
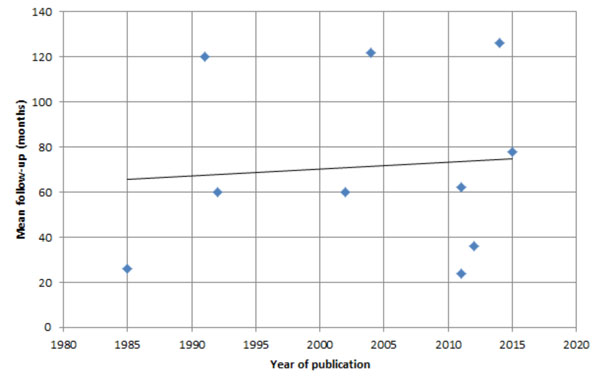
A graph demonstrating the mean follow-up rates (y-axis) for studies included in Fig. (1), plotted against year of publication (x-axis). The line of best fit suggests that the mean follow-up has not significantly changed over time.
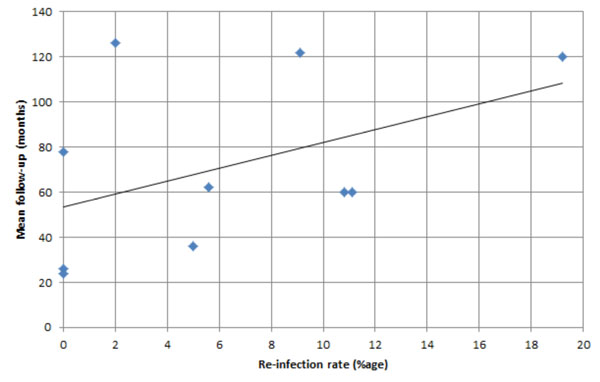
A graph demonstrating the mean follow-up rates (y-axis) for studies included in Fig. (1), plotted against re-infection rates (x-axis). The line of best fit suggests, as expected, the longer the follow-up, the greater the re-infection rate.
Demographics details and procedures performed for the studies included in the review.
| Author | Year | Gender | Mean Age/Age Range | Number of Knees | Procedure details | Average Follow-up |
|---|---|---|---|---|---|---|
| Freeman [12] | 1985 | 6F/2M | 47-78 | 8 | Prosthesis and all suspicious tissue removed, joint washed with saline, new prostheses implanted with Gentamicin-impregnated cement | 12-40 months |
| Von Foerster [13] | 1991 | Not Reported | Not reported | 104 | Components removed, joint debrided with suspicious tissue removed, washed with saline and packed with iodine soaked swabs. Team changed gowns and instruments and new prostheses implanted with gentamicin-impregnated cement | 5-15 years |
| Goksan [14] | 1992 | 12F/6M | 61.4 (42-74) | 18 | Components removed, joint debrided with suspicious tissue removed, washed with saline and packed with iodine soaked swabs. Team changed gowns and instruments and new prostheses implanted with gentamicin-impregnated cement | 5 years |
| Silva [15] | 2002 | Not Reported | Not reported | 37 | Not reported | 5 years |
| Buechel [16] | 2004 | Not Reported | 58-86 | 21 | Not reported | 10.2 years |
| Bauer [17] | 2006 | Not Reported | Not reported | 31 | Not reported | 52 months |
| Whiteside [18] | 2010 | 11F/7M | 69 (58-84) | 18 | One stage revision protocol that included debridement, uncemented revision of total knee components, and intraarticular infusion of 500mg vancomycin via Hickman catheter once or twice daily for 6 weeks. No intravenous antibiotics after the first 24 hours | 62 months |
| Parkinson [19] | 2011 | Not Reported | Not reported | 22 | ‘Two in one’ technique | 24 months |
| Singer [20] | 2012 | 32F/31M | 70.7 (31-89) | 63 | Not reported | 36 months |
| Baker [21] | 2012 | 15F/18M | 69.4 (SD 10.7) | 33 | Not reported | 7 months |
| Tibrewal [22] | 2014 | 33F/17M | 66.8 (42-84) | 50 | Components removed, joint debrided with suspicious tissue removed, washed with saline and packed with iodine soaked swabs. Team changed gowns and instruments and new prostheses implanted with gentamicin-impregnated cement | 10.5 years |
| Haddad [23] | 2015 | 14F/14M | 65 (45-87) | 28 | Components removed, joint debrided with suspicious tissue removed, washed with saline and packed with swabs. Team changed gowns and instruments and new prostheses implanted with gentamicin-impregnated cement | 6.5 years |
Outcomes for the studies included in this review including infection rate, function and range of movement.
| Author | Reinfection (Number / Percentage) | Function | Average Range of Movement | Additional Comments |
|---|---|---|---|---|
| Freeman [12] | 0 | Time spent walking improved in all cases, improvement in range of knee flexion | Not reported | None |
| Von Foerster [13] | 20 (19.2%) | Not reported | Not reported | None |
| Goksan [14] | 2 (11.1%) | Pain free walking (8/18), no need for walking aids (7/18) | 87o flexion | Patient population: 10 Rheumatoid Arthritis, 7 Osteoarthritis, 1 post traumatic arthritis. Two patients with reinfection - both had severe rheumatoid arthritis and suffered several recurrences of infection |
| Silva [15] | 4 (10.8%) | Not reported | Not reported | Factors associated with successful single stage revisions - Infections by Gram positive organisms, absence of sinus formation, and use of antibiotic-impregnated bone cement for the new prosthesis and 12 weeks of antibiotic therapy |
| Buechel [16] | 2 (9.1%) | Mean Knee Society Score 79.5 85.7% good or excellent results |
Not reported | None |
| Bauer [17] | Not reported | 40% of the knees had an excellent outcome, 30% a good outcome and 30% a fair or poor outcome. Knee Society Score (function) 62.5. Functional outcome was fair or poor in 55% of patients |
Not reported | Article in French. Length of infection before re-implantation, number of surgical procedures and bacterial virulence/resistance were not predicting factors for failure. Unfavourable systemic and local conditions decreased the rate of success after revision |
| Whiteside [18] | 1 (5.6%) | All patients achieved full weight bearing by 3 months after surgery. Mean Knee Society Score 78±8 at 1 year, 83±9 at 2 years, 84±8 at 5 years, 85±10 at 6 years, and 84 at 8 years |
Not reported | All patients were infected with MRSA. All patients had important comorbidities: 9 patients had Type II diabetes, 12 had chronic dependency oedema and stasis dermatitis, 9 had morbid obesity, and 15 had malnutrition and hypoalbuminemia. 17 of the 18 patients had two or more comorbidities |
| Parkinson [19] | 0 | Significant improvement in SF-12 PCS, WOMAC pain and stiffness scores | Not reported | Presentation at Liverpool Congress 2008 |
| Singer [20] | 3 (5%) | Improvement in clinical scores in all 60 patients who did not have a reinfection. Mean pre-operative Knee Society Score 22, mean function score 21, and mean Oxford Knee Score 48. Mean post-operative (24 months) Knee Society Score 72, mean function score 71, and mean Oxford Knee Score 27 |
104o +/- 11 | Excluded MRSA/MRSE. 11/63 patients infected with anaerobic bacteria |
| Baker [21] | Not reported | Oxford Knee Score: 24.9 (SD 13.1), EQ5D: 0.495 (SD 0.397). Patient satisfaction excellent, very good or good: 20/33 patients (61%). Operation success: 21/32 patients (66%). Complication score: 84% (29/33) had complications including post-operative bleeding, wound problems, requirement for further surgery and requirement for readmission |
Not reported | Satisfaction is assessed by asking the patient: ‘How would you describe the results of your operation?’ Possible responses are Excellent/Very Good/Good/Fair/Poor. Success after surgery was similarly assessed with the question ‘Overall, how are your knee problems now compared to before your operation?’ with the corresponding responses: Much better/A little better/Much the same/A little worse/ Much worse. Questions relating to complications are derived from the patient’s experience of surgery questionnaire which has previously been used to audit complications after day-case surgery |
| Tibrewal [22] | 1 (2%) | Oxford Knee Score increased by a factor of 2.4 from 14.5 (6-25) pre-operatively to 34.5 (26-38) one year after surgery. A mean absolute improvement of 20.0 points (95% CI: 17.8 to 22.2, p < 0.001) |
Not reported | Four patients were infected - 1 reinfection, 3 with new infection which did not require another revision (2 with rheumatoid arthritis, 1 severely obese). Ten patients underwent revision due to loosening |
| Haddad [23] | 0 | Knee Surgery Score: Average 56 point (32-88) increase over 2 years to 88 (38-97). Visual analogue scale: 7.82 |
Not reported | Radiographic findings showed a well-fixed prosthesis in all patients of with no evidence of loosening at the most recent follow-up |
Effect of Microbiologic Profile
Almost 70-80% of TKA infections are caused by gram positive staphylococci and streptococci, 10-20% aerobic gram-negative and 10% anaerobic bacteria [24]. Two recent studies have also taken into account resistant bacteria, one study in particular focusing primarily on patients infected with MRSA [18, 20]. The relatively larger retrospective study conducted by Singer et al. [20] on 63 patients specifically excluded MRSA and Methicillin Resistant Staphylococcus epidermidis (MRSE) but retained 18% of patients infected with anaerobic bacteria (Enterococcus faecalis and Propinoibacterium acnes). The patients were then divided based on the new prostheses implanted (unicompartmental, primary total knee and hinged) and analysed. Three patients from the hinged prostheses group suffered re-infections with none from either of the other two groups. However, it is unclear what the three patients were infected with before revision surgery. Compared to Singer et al., Whiteside et al. had a smaller study that focused primarily on 18 knees infected with MRSA [18]. The patients had significant co-morbidities such as Type II diabetes, morbid obesity, chronic dependency oedema, stasis dermatitis, malnutrition and hypoalbuminuria with 17 out of the 18 patients having two or more co-morbidities. Additionally, the single stage procedure also involved an intra-articular infusion of 500mg vancomycin via a Hickman catheter once or twice daily for six weeks and no intravenous antibiotics after the first 24 hours. Patients were then followed up for a minimum of 27 months with only one patient developing a recurrence of infection.
Functional Outcome
Table 2 outlines the functional outcomes in the included studies where details were provided. For most of the studies, knees scoring systems were used to assess function, pain and other symptoms. The scores can be divided into clinician-based outcome measures (CBOMs) and patient reported outcome measures (PROMs). The most commonly used CBOM was the Knee Society Score [25] that split into two parts. The first part assesses pain, flexion contracture and extension lag, total range of flexion, alignment and stability [26]. The second part focuses on functionality such as walking, climbing stairs and whether walking aids are used. Studies which analysed the Knee Society Scores of patients have produced results ranging from 62.5-88 [16-18, 20, 23]. In Whiteside et al.’s study, the mean Knee Society Score was 78 ± 8 at 1 year, 83 ± 9 at 2 years, 84 ± 8 at 5 years, 85 ± 10 at 6 years, and 84 at 8 years. Two studies have also showed a significant improvement of preoperative scores of 50 [20] and 56 points [23] over 24 months.
The primary PROM used was the Oxford Knee Score [27] that is a knee-specific, patient-administered questionnaire exploring the patients’ subjective assessment of pain and functional capacity. It is a reliable scoring system with a score of 40-48 indicating satisfactory joint function with a decreasing value representing increasingly severe knee arthritis [28]. The study by Baker et al. specifically analysed the Oxford Knee Score (OKS), Euroqol-5D (EQ5D) and patient satisfaction with the aim of investigating whether single or two stage revision for infection resulted in better knee function, overall perception of health status and better patient perceived success and satisfaction [21]. The results for the single stage procedure were an OKS of 24.9, EQ5D of 0.495 and 61% of patients perceiving their operation to be excellent, very good or good. The low OKS and EQ5D score could possibly be explained by the high complication rate of 84% that included post-operative bleeding, wound problems, requirement for further surgery and requirement for readmission. However, the complication rate was not significantly different from the two stage revision. A more recent study by Tibrewal et al. also analysed the OKS of 14 out of 50 patients and showed an improvement of 20 points from a mean score of 14.5 pre-operatively to 34.5 post-operatively over a year [22].
Duration of Follow-Up
The average follow up periods varied greatly between studies from 7 months to 15 years. We plotted the mean follow-up rates for these studies against year of publication (Fig. 2), and the graph suggested that the mean follow-up has not significantly changed over time. Although most studies were assessing re-infection rates, only two mentioned prosthesis loosening over a period of 10.5 and 6.5 years [22, 23]. The study by Tibrewal et al. that followed up 50 knees over 10.5 years reported that 10 knees had to undergo further revision surgery due to prosthesis loosening. However, the latest study by Haddad et al. showed no loosening of prosthesis at 6.5 years.
DISCUSSION
This is the largest published systematic review of single stage knee revisions. The evidence behind the use of single stage knee revisions is gradually increasing. Despite many studies showing positive results, few studies are powerful enough to show any meaningful benefit. The studies included in this review have mainly been retrospective studies with a small patient cohort, leading to confounding, bias and difficulties in reaching statistical significance. The evidence so far would prove difficult to justify against the proven track record of a two stage technique. In view of this, the ideal study would be a prospective randomised control trial comparing infection rates, knee scores and patient quality of life post-surgery in both single and two stage approaches. The study would need to be conducted internationally to take into consideration different patient populations, the seniority of the surgeon and gain enough numbers to be powerful enough. Furthermore, a consensus would have to be reached in the technique of performing a single stage approach as there are currently no broadly agreed standards. This should hopefully lead to different centres adapting their techniques to improve patient outcomes.
There are many factors that make confound matters and the studies included in this review are heterogenous. In view of the limited studies available, we are analysing the ‘two-in-one’ technique with other single stage revision procedures, and ignoring differences in cemented and uncemented implants as well as antibiotic regimens. This would not be the case if larger number of studies were available.
However, considering the rate of recurrence of infection alone, all of the studies to date have shown a high percentage of successful outcomes. Generally, the revisions that failed were in patients with an underlying rheumatologic condition, poor physiological status and an infection with an atypical organism. Silva et al. in 2002 [15] looking at 37 knees identified four factors that predicted successful clearance of infection: (1) Infections with Gram positive organisms, (2) Absence of sinus formation, (3) Use of antibiotic-impregnated bone cement with the new prosthesis and (4) 12 weeks of antibiotic therapy following surgery. It could be argued that a single stage approach would be appropriate for patients who have multiple co-morbidities and are not able to tolerate a period of limited mobility and a second anaesthetic.
To date, only two studies have taken into consideration both the Knee society score and the OKS. However, the results of all studies have shown a wide variation for both scoring systems. It can be assumed that a successful single stage revision does improve pre-operative scores. However, whether the scores differ from a two stage approach would only be determined by analysing and accumulating more single stage studies looking into patient outcomes.
CONCLUSION
Single stage knee revision has the potential to be more beneficial to patients compared to a two stage approach. However the current evidence for single stage revision is variable and there is a lack of good quality evidence to address whether single stage revisions is thorough enough to eradicate deep infection and able to restore adequate function. This emphasizes the need for larger prospective studies with standardised procedures and protocol, and with adequate follow-up. Till then, patients considered for a single stage approach should be thoroughly assessed and the surgery should be performed by a senior surgeon with experience in single stage knee revisions.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


